- Department of Neurosurgery, King Edward Medical University, Mayo Hospital, Lahore, Punjab, Pakistan,
- Department of Neurosurgery, Punjab Institute of Neurosciences, Lahore General Hospital, Lahore, Punjab, Pakistan.
DOI:10.25259/SNI_11_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Sundus Ali1, Adnan Qasim1, Bilal Anwar2, Nabeel Choudhary2, Muhammad Akmal2. Intradural extension of mucocele secondary to giant frontal sinus osteoma: Diagnostic pitfalls. 31-May-2021;12:252
How to cite this URL: Sundus Ali1, Adnan Qasim1, Bilal Anwar2, Nabeel Choudhary2, Muhammad Akmal2. Intradural extension of mucocele secondary to giant frontal sinus osteoma: Diagnostic pitfalls. 31-May-2021;12:252. Available from: https://surgicalneurologyint.com/surgicalint-articles/10831/
Abstract
Background: Paranasal sinus osteoma in association with intracranial mucocele is a rare entity while intradural extension is even rarer. Our aim of presenting this case is to highlight the diagnostic pitfalls and reiterate the importance of prompt treatment of expected complications.
Case Description: A 35-year-old known epileptic, for the past 5 years, presented with altered sensorium for the past 2 days. Computed tomography (CT) of the brain plain showed ventriculomegaly and cystic lesion in the left frontal lobe adjacent to a calvarial osteoma. A ventriculoperitoneal (VP) shunt was done which resulted in tension pneumocephalus and led us to discover the origin of osteoma from the left frontal sinus on CT functional endoscopic sinus surgery (FESS) protocol. He underwent left frontal craniotomy. The osteoma and mucocele were excised completely and watertight primary dural closure was done. Postoperative meningitis was treated with antibiotics according to the culture report.
Conclusion: Intracranial extension of mucocele led to meningitic hydrocephalus, prompting us for VP shunt. Resulting tension pneumocephalus revealed what was missed on preop CT, a small pocket of air adjacent to osteoma intracranially. Therefore, this case underscores the importance of obtaining a preoperative CT FESS to elaborate the origin of osteoma, thus planning approach differently.
Keywords: Frontal sinus, Intradural extension, Mucocele, Osteoma
INTRODUCTION
Osteomas are slow-growing benign tumors of unknown etiology, affecting population in the 2nd and 3rd decades with slight male preponderance (2:1). The proposed etiologies are developmental, posttraumatic, or postinfectious. About 3% occur in association with paranasal sinuses (PNSs) having predilection for fronto-ethomid sinus.[
CASE DESCRIPTION
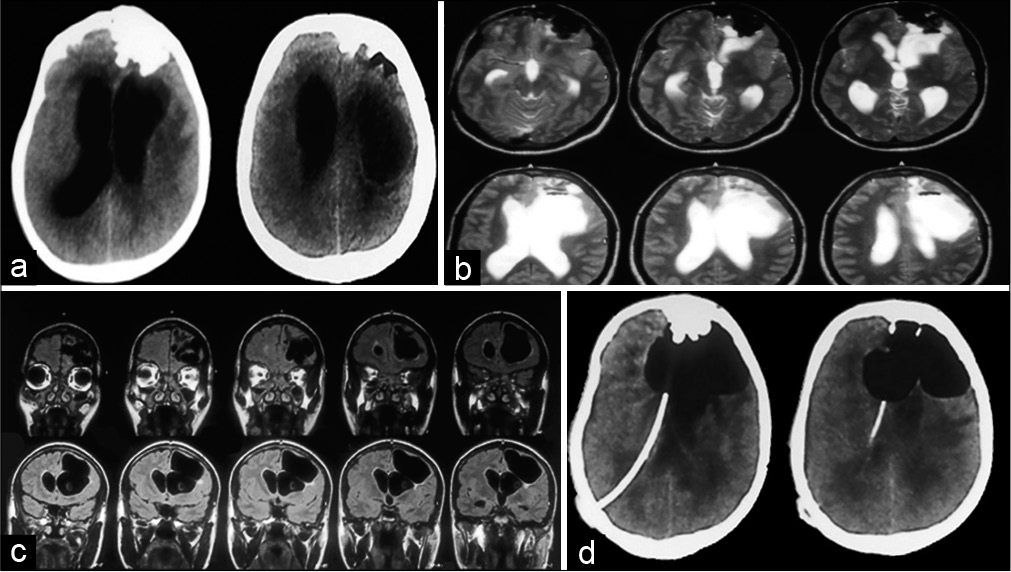
A 35-year-old male known epileptic, presented with altered sensorium for the past 2 days. On local examination, a 5 × 3 cm irregular bony swelling noted on the left forehead. There was no focal neurological deficit and no signs of meningeal irritation. Computed tomography (CT) of the brain plain showed a calcified lesion in the left frontal region along with ventriculomegaly and a huge cystic lesion in the left frontal region [
Figure 1:
(a) Plain computed tomography (CT) brain showing left frontal irregular bony growth with intracranial projection, ventriculomegaly and left paraventricular cystic SOL. (b) Magnetic resonance imaging (MRI) brain plain T2 axial images showing irregular hypointense left frontal lesion encroaching on left frontal lobe, paraventricular cystic lesion of cerebrospinal fluid intensity is noted with air-fluid level in it. (c) T1 coronal MRI depicting relation of cyst to ventricle. (d) Post-op CT brain plain following ventriculoperitoneal shunt done for hydrocephalus showing enlargement of aerocele.
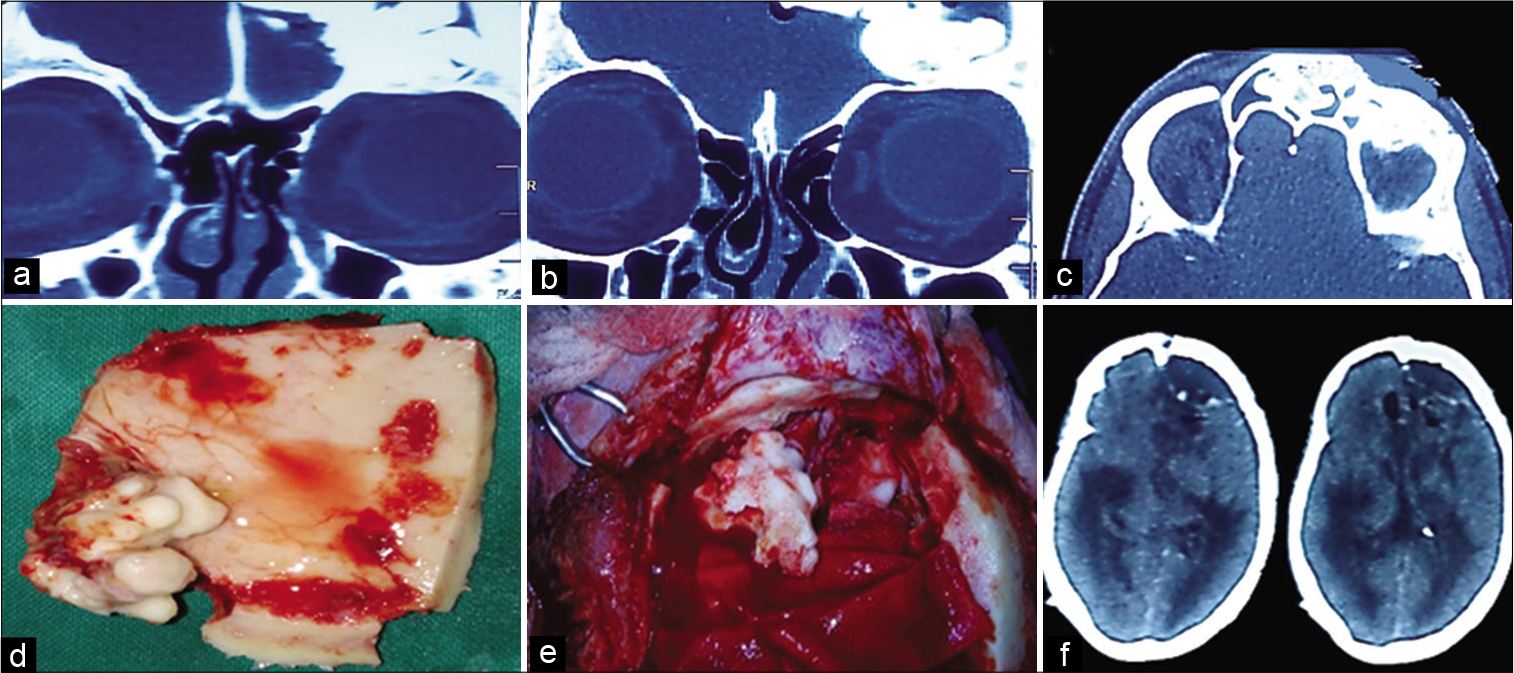
CT bone window was done, which elaborated details of osteoma [
Figure 2:
Computed tomography (CT) bone window (a and b) coronal view showing attachment of osteoma to the roof of orbit, lateral to the lamina paprycea signifying no ethmoidal involvement (c) axial view showing AP diameter of lesion filling >75% of frontal sinus respectively. (d) Inner aspect of free bone flap incorporating part of osteoma. (e) Remaining osteoma projecting from left frontal sinus (f) postop scan showing complete excision of osteoma but delayed extradural collection.
DISCUSSION
In neurosurgical emergency, cases of hydrocephalus presenting with altered sensorium are routinely shunted. Here, we attempt to highlight a simple but rare cause of hydrocephalus, in which the underlying cause was overlooked being rare as well as lack of detailed 3D imaging in ER.
In this case, osteoma was assumed to be of calvarial origin as no apparent association with cyst or any sinus was appreciated on routinely done CT. More than 1 cm slice thickness, bony lesion overlapping orbital roof and acquisition only in axial view are the potential pitfalls of routine scan which can be resolved by CT functional endoscopic sinus surgery (FESS). It was the enlargement of aerocele after shunt which raised the suspicion of relation of osteoma with PNS. To confirm, CT FESS was done, which revealed the exact anatomical details of osteoma in 3D. Retrospective review of imaging revealed small foci of air entrapped between osteoma and adjacent brain on plain CT and air-fluid level within cyst on MRI brain.
We speculate that the meningitis due to intradural extension of mucocele was the cause of altered sensorium as well as hydrocephalus. This is supported by CSF pleocytosis found after shunting. The absence of signs of meningitis at presentation and negative culture after shunt cannot reliably exclude meningitis. The existing guidelines for surgical management are based on the grading system proposed by Chiu,[
Our case belonged to grade III (high grade) so we chose transcranial route to achieve near-total removal of bony lesion and effective dural repair. We speculate that dural disruption due to mucocele was culprit for bacterial meningitis, and it was there long before cultures were positive.
CONCLUSION
We speculate that the meningitis was the cause of altered sensorium as well as hydrocephalus. The absence of signs of meningitis at presentation cannot reliably exclude meningitis. Small foci of air on CT and fluid level on MRI also provide clue to the underlying pathology. Through evaluation of apparently calvarial bony lesions adjacent to PNS, via CT FESS should be the rule, and if implemented earlier in this case, not only a single procedure dealing with osteoma and CSF diversion would suffice, but later could be temporary thus avoiding permanent shunt hardware.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Cheng KJ, Wang SQ, Lin L. Giant osteomas of the ethmoid and frontal sinuses: Clinical characteristics and review of the literature. Oncol Lett. 2013. 5: 1724-30
2. Chiu AG, Schipor I, Cohen NA, Kennedy DW, Palmer JN. Surgical decisions in the management of frontal sinus osteomas. Am J Rhinol. 2005. 19: 191-7
3. Earwaker J. Paranasal sinus osteomas: A review of 46 cases. Skeletal Radiol. 1993. 22: 417-23
4. Erdogan N, Demir U, Songu M, Ozenler NK, Uluç E, Dirim B. A prospective study of paranasal sinus osteomas in 1,889 cases: Changing patterns of localization. Laryngoscope. 2009. 119: 2355-9
5. Fu CH, Chang KP, Lee TJ. The difference in anatomical and invasive characteristics between primary and secondary paranasal sinus mucoceles. Otolaryngol Head Neck Surg. 2007. 136: 621-5
6. Gezici AR, Okay O, Ergün R, Dağlıoğlu E, Ergüngör F. Rare intracranial manifestations of frontal osteomas. Acta Neurochir. 2004. 146: 393-6
7. Ledderose GJ, Betz CS, Stelter K, Leunig A. Surgical management of osteomas of the frontal recess and sinus: Extending the limits of the endoscopic approach. Eur Arch Otorhinolaryngol. 2011. 268: 525-32
8. Novaes V, Pinaud M, Paranhos JL, D’Alessandro JR. Aspectos neurocirúrgicos dos osteomas fronto-etmoidais: Relato de 6 casos e revisão da literatura. Arq Neuropsiquiatr. 1977. 35: 197-209
9. Seiberling K, Floreani S, Robinson S, Wormald PJ. Endoscopic management of frontal sinus osteomas revisited. Am J Rhinol Allergy. 2009. 23: 331-6