- Department of Surgery, Jawaharlal Nehru Institute of Medical Sciences, Imphal, Manipur, India.
- Department of Neurosurgery, Jawaharlal Nehru Institute of Medical Sciences, Imphal, Manipur, India.
- Department of Orthopaedics, Jawaharlal Nehru Institute of Medical Sciences, Imphal, Manipur, India.
Correspondence Address:
Boris Kangabam
Department of Orthopaedics, Jawaharlal Nehru Institute of Medical Sciences, Imphal, Manipur, India.
DOI:10.25259/SNI_197_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Boris Kangabam1, Thokchom Amataleima1, Mayanglambam Amitkumar2, Takhelmayum Umesh3. Intradural extramedullary tuberculoma of the thoracic spine – A rare case report of paraparesis. 08-Apr-2021;12:136
How to cite this URL: Boris Kangabam1, Thokchom Amataleima1, Mayanglambam Amitkumar2, Takhelmayum Umesh3. Intradural extramedullary tuberculoma of the thoracic spine – A rare case report of paraparesis. 08-Apr-2021;12:136. Available from: https://surgicalneurologyint.com/surgicalint-articles/10707/
Abstract
Background: Intradural extramedullary tuberculoma of the spinal cord (IETSC) is an extremely rare form of spinal tuberculosis (TB) that is believed to be due to a host’s immune reaction against the Mycobacterium protein derivatives.
Case Description: A 25-year-old male with human immunodeficiency virus, hepatitis C virus, and disseminated TB on antitubercular therapy for the past 8 months, presented with paraplegia of 2 months duration. When the MRI spine revealed multiple peripheral rim enhancing intradural extramedullary lesions from T6 to T8 and dorsally from T10 to T11, the patient was diagnosed with IETSC. At surgery, we countered cystic lesions adherent to the dura and the spinal cord, containing a whitish material. Postoperatively, the patient showed clinical improvement in motor power and sensation.
Conclusion: Intradural extramedullary spinal tuberculomas in patients with a history of TB and spinal cord compression, although rare, should be considered among the differential diagnoses.
Keywords: Intradural extramedullary, Spine, Tuberculosis
INTRODUCTION
Intradural spinal tuberculomas are extremely rare (i.e., 5% of cases) and intradural extramedullary tuberculoma of the spinal cord (IETSC) is even less frequently encountered.[
CASE REPOR
A 25-year-old male with known case of disseminated tuberculosis (TB), hepatitis C, and human immunodeficiency virus (HIV) presented with a progressive paraparesis and loss of sphincter control (T8 level) of 2 months duration. He had already been on antitubercular therapy for the prior 8 months and had been taking antiretroviral therapy medication for HIV since 2018, although on an irregular basis.
MR study
The thoracic MRI revealed multiple peripheral rim enhancing contiguous intradural extramedullary lesions along the right side of the dura from T6 to T8 thoracic, and dorsally from T10 to T11. This was accompanied by diffuse pachymeningeal enhancement resulting in moderate/severe cord compression at T7-T8 and diffuse cord edema from T5-T11. Lesions were hyperintense on T2-weighted images and hypointense on T1-weighted images [
Lumbar cerebrospinal fluid (CSF) findings
The lumbar CSF puncture revealed colorless fluid with a protein of 58 mg%, glucose of 43 mg%, and cell count of 80 per cumm (all lymphocytes). The CSF Ziehl–Neelsen stain and cartridge-based nucleic acid amplification test yielded negative results.
Surgery, cultures, and pathology
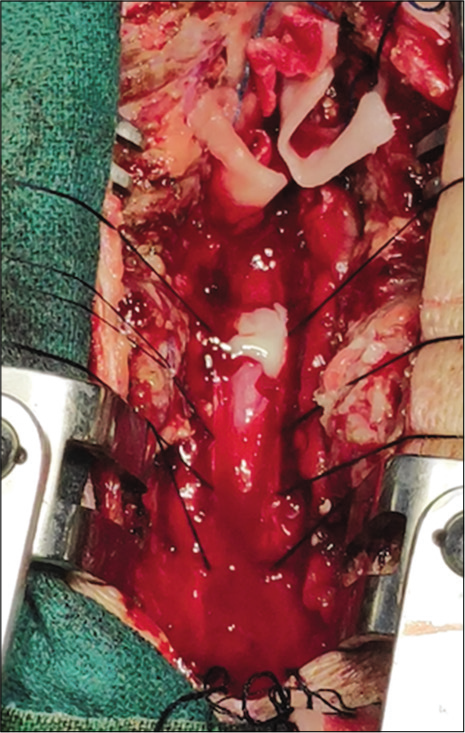
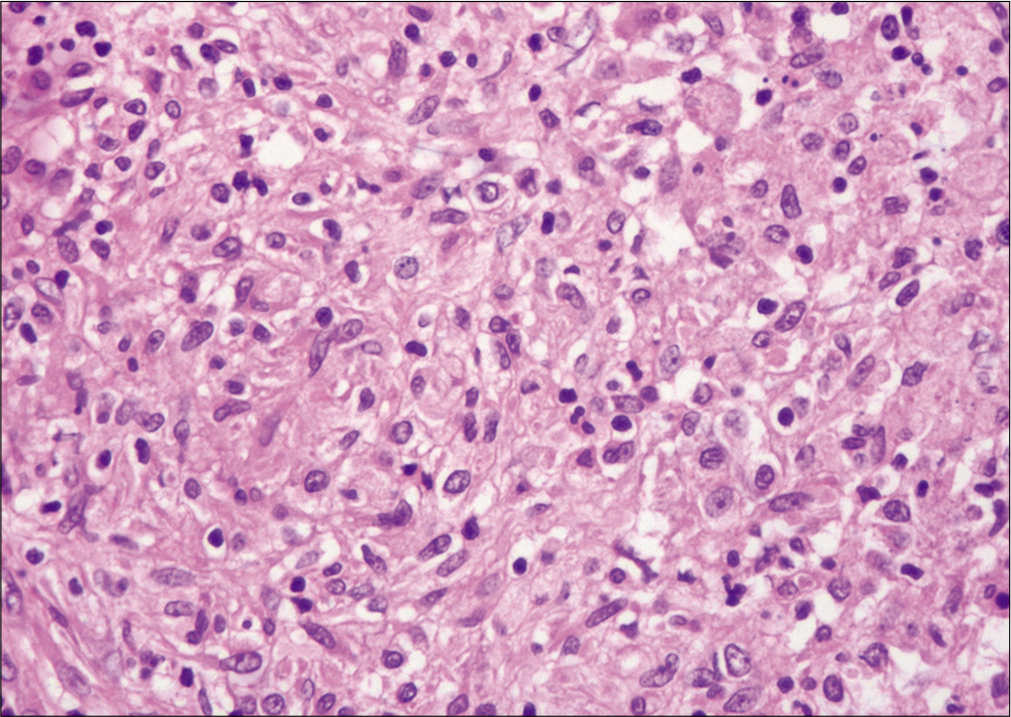
The patient underwent a laminectomy from T5 to T8. At surgery, a cystic lesion measuring 3 cm×1.5 cm×1 cm was found adherent to the dura and spinal cord; the capsule contained 3 cc of a whitish material that was positive for acid-fast bacilli Ziehl–Neelsen staining [
Postoperative course
Postoperatively, there was gradual but only slight clinical improvement. Two weeks following surgery, motor power was 3/5 in both lower extremities, while the prior sensory and sphincteric deficits fully resolved.
DISCUSSION
TB can present 10% of the time in the central nervous system.[
IETSC is the rarest type of spinal TB seen only in 1 out of 50,000 cases, and is usually found in young individuals presenting with three variants; in healthy individuals with no primary TB history, in those with disseminated TB, and in those with recent TB history previously treated with antitubercular therapy successfully.[
Although medical therapy is the mainstay of treatment, prompt surgical intervention may be warranted for those with significant neurological deficits attributed to cord compression.[
CONCLUSION
Although IETSC is an extremely rare form of spinal TB, it must be considered among the differential diagnoses for those presenting with a known history of TB and spinal cord compression. Where patients present with significant deficits secondary to cord compression, prompt surgical intervention/decompression may be warranted.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Dastur HM. Diagnosis and neurosurgical treatment of tuberculous disease of the CNS. Neurosurg Rev. 1983. 6: 111-7
2. Jeong DK, Kwon YM. Intradural extramedullary tuberculoma of the spinal cord following tuberculous meningitis. Korean J Spine. 2015. 12: 107-10
3. Kaur H, Mittal GK, Singhdev J. Intradural extramedullary tuberculoma of the spinal cord in patient of tubercular meningitisan uncommon scenario. Indian J Tuberc. 2020. 67: 426-9
4. Takahashi H, Ito S, Kojima S, Tanno T, Hattori T. Intradural extramedullary tuberculoma of the thoracic spine: Paradoxical response to antituberculous therapy. Intern Med. 2008. 47: 797-8
5. Verma K, Crothers T, Neuman B, Vaccaro A, Heller J. A case of intradural extramedullary spinal tuberculosis diagnosed 8 years after treatment of the primary infection. JHN J. 2013. 8: 14-7