- Department of Neurosurgery, Federal University of Ceará, Sobral, Ceará, Brazil.
Correspondence Address:
Samuel Teixeira de Oliveira, Department of Neurosurgery, Federal University of Ceará, Sobral, Ceará, Brazil.
DOI:10.25259/SNI_180_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Samuel Teixeira de Oliveira, Joaquim Francisco Cavalcante-Neto, Luís Eduardo Oliveira Matos, Paulo Roberto Lacerda Leal, Espártaco Moraes Lima Ribeiro, Gerardo Cristino-Filho, Keven Ferreira da Ponte. Intraparenchymal pericatheter cyst as an indicator of ventriculoperitoneal shunt malfunction: A case-based update. 06-May-2022;13:195
How to cite this URL: Samuel Teixeira de Oliveira, Joaquim Francisco Cavalcante-Neto, Luís Eduardo Oliveira Matos, Paulo Roberto Lacerda Leal, Espártaco Moraes Lima Ribeiro, Gerardo Cristino-Filho, Keven Ferreira da Ponte. Intraparenchymal pericatheter cyst as an indicator of ventriculoperitoneal shunt malfunction: A case-based update. 06-May-2022;13:195. Available from: https://surgicalneurologyint.com/surgicalint-articles/11577/
Abstract
Background: Intraparenchymal pericatheter cysts (IPCs) are a rare ventriculoperitoneal shunt (VPS) complication, with only a few cases recorded in the literature.
Case Description: We report a 22-year-old woman admitted with headache, papilledema, vision loss, and a history of leukemia. Lumbar puncture revealed idiopathic intracranial hypertension (IIH). Three months after VPS implantation, she was readmitted with headache and worsening of visual impairment. CT evidenced a IPC with perilesional edema. Intraoperatively, a shunt revision and cyst drainage were opted for. We present a discussion and literature review on this unique complication of VPS, with emphasis on management.
Conclusion: It is important to understand and consider IPCs as complications of VPS surgery, including in adult patients and IIH cases.
Keywords: Catheter obstruction, Cerebrospinal fluid edema, Idiopathic intracranial hypertension, Intraparenchymal pericatheter cyst, Ventriculoperitoneal shunt
INTRODUCTION
Ventriculoperitoneal shunt (VPS) is the main surgical intervention for communicating or obstructive hydrocephalus and idiopathic normal-pressure hydrocephalus. It can also be performed in idiopathic intracranial hypertension (IIH) when there is no response to medical therapy or there is visual dysfunction worsening. Although standard in several conditions, the procedure shows a considerable rate of complications (~23.8% in adults).[
Intraparenchymal pericatheter cyst (IPC) is a rare complication of VPS, occurring mainly in children. To date, only 35 cases have been reported in the literature, of which, 14 were in adults, and four were in IIH patients. The aim of this article is to present a case of IPC formation in an adult, as well as to review the literature on the subject.
CASE PRESENTATION
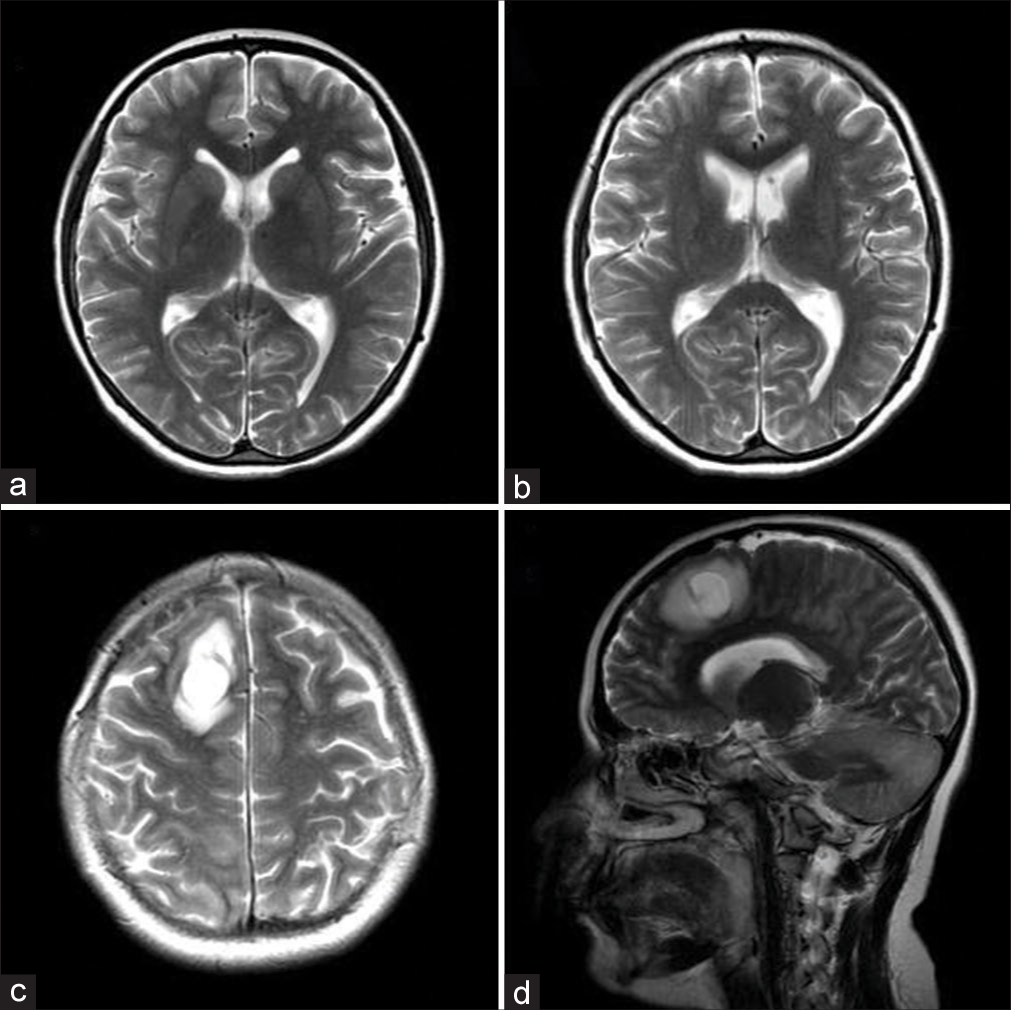
A 22-year-old woman with a history of leukemia presented with progressive headache, papilledema, and visual loss at admission. Magnetic resonance imaging (MRI) was normal [
Figure 1:
Imaging comparison. MRI at admission (before VPS surgery): (a) axial T2 view demonstrating no hydrocephalus. The lumbar puncture confirmed the diagnosis of idiopathic intracranial hypertension. MRI at revaluation (3 months later): (b) lower axial T2, (c) upper axial T2, and (d) parasagittal T2W1 views demonstrating the catheter pathway with an intraparenchymal pericatheter cyst and perilesional edema.
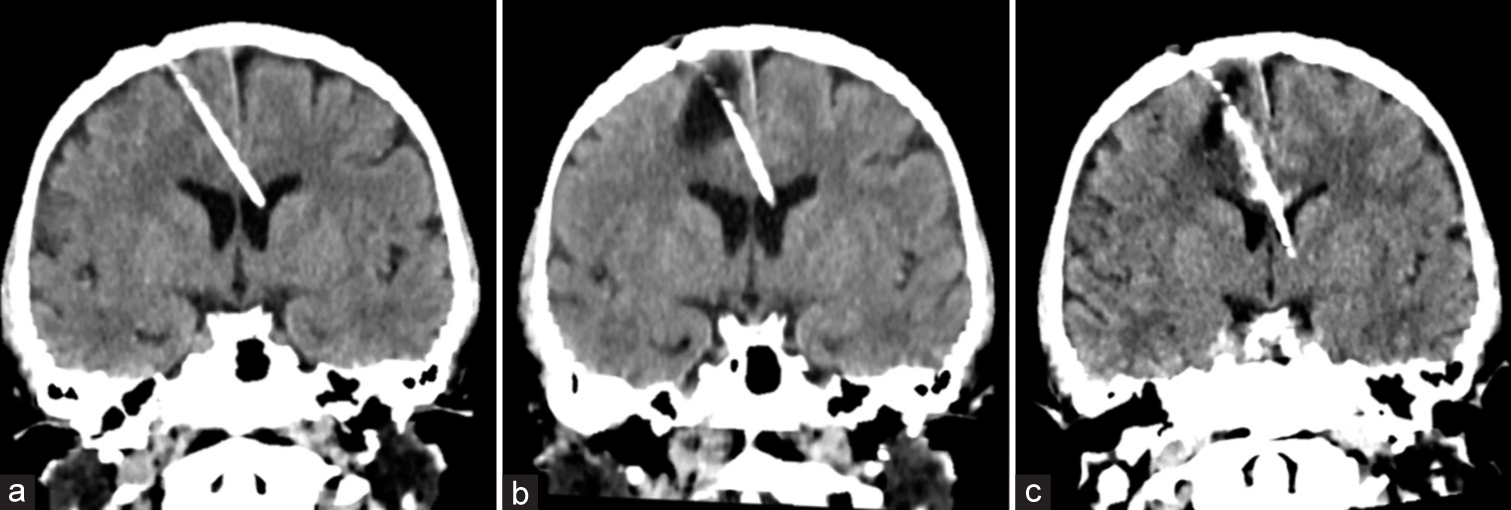
Figure 2:
Imaging comparison. CT after VPS surgery: (a) coronal view demonstrating the catheter pathway without any parenchymal lesion. CT at revaluation (3 months later): (b) coronal view demonstrating the catheter pathway with an intraparenchymal pericatheter cyst and perilesional edema, without hydrocephalus. CT after shunt revision (postoperative): (c) coronal view demonstrating the new catheter pathway with cyst regression and mild intracystic hemorrhage.
The patient was readmitted 3 months later due to the recurrence of headache symptoms and visual impairment. Computed tomography (CT) [
VPS revision was performed, and a proximal obstruction identified [
DISCUSSION AND LITERATURE REVIEW
VPS is a very common procedure, used mainly for treating hydrocephalus or idiopathic normal-pressure hydrocephalus. However, it is also an alternative for IIH, particularly in refractory cases or those involving visual deterioration.[
IPCs, however, are very rare complications of VPS. Although they can also appear in Ommaya reservoirs, only VPS cases were considered in this review. Furthermore, only reports with adequate clinical and imaging descriptions were included in the study [
Patients with this complication present with varied symptoms, the most frequent being headache (~40%), vomiting (~27%), and visual changes (~10%). There have also been reports of decreased levels of consciousness, hemiparesis, speech and gait disorders, tinnitus, and epileptic seizures. One patient was asymptomatic at re-evaluation, and the IPC was found by routine imaging tests.[
Imaging tests are of utmost importance to make a differential diagnosis of parenchymal lesions in VPS patients as well as to identify concomitant conditions significant to the therapeutic approach. The CT examination can assist in the diagnosis of IPCs, and it is very often the initial imaging test. However, MRI is the most helpful examination as it allows the correct distinction between cysts and their differential diagnoses due to its better resolution.[
CSF edema, tumors, abscesses, and dysembryogenetic lesions are all considered cyst-like lesions.[
Early recognition and treatment of an IPC can provide complete clinical improvement and cyst regression.[
Some authors have questioned the necessity of shunt revision, especially in asymptomatic patients. Revision was not performed in four cases, three of them being managed conservatively with clinical and imaging surveillance,[
CONCLUSION
Although rare entities, it is important to understand and consider IPCs as complications of VPS surgery, including in adult patients and IIH cases. Shunt revision is the standard approach, though conservative treatment has been performed in specific conditions.
Declaration of the patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Aly B, Hammad W, Elkhouly H. Uncommon complications of ventriculoperitoneal shunt: Experience in 22 cases. Al-Azhar Assiut Med J. 2015. 13: 360-73
2. Amans MR, Dillon WP. Cerebral parenchymal cyst: A rare complication of ventriculoperitoneal shunt malfunction in an adult. Radiol Case Rep. 2015. 8: 784
3. Balasubramaniam S, Tyagi DK, Sawant HV. Intraparenchymal pericatheter cyst following disconnection of ventriculoperitoneal shunt system. J Postgrad Med. 2013. 59: 232-4
4. Bianchi F, Frassanito P, Tamburrini G, Caldarelli M, Massimi L. Shunt malfunction mimicking a cystic tumour. Br J Neurosurg. 2017. 31: 484-6
5. Chiba Y, Takagi H, Nakajima F, Fujii S, Kitahara T, Yagishita S. Cerebrospinal fluid edema: A rare complication of shunt operations for hydrocephalus. Report of three cases. J Neurosurg. 1982. 57: 697-700
6. Iqbal J, Hassounah M, Sheikh B. Intraparenchymal pericatheter cyst. A rare complication of ventriculoperitoneal shunt for hydrocephalus. Br J Neurosurg. 2000. 14: 255-8
7. Jena RK, Agrawal A, Sandeep Y, Shrikhande NN. Intraparenchymal pericatheter cyst in a patient with cerebral shunt malformation. Narayana Med J. 2016. 5: 145-7
8. Kale HA, Muthukrishnan A, Hegde SV, Agarwal V. Intracranial perishunt catheter fluid collections with Edema, a sign of shunt malfunction: Correlation of CT/MRI and nuclear medicine findings. AJNR Am J Neuroradiol. 2017. 38: 1754-7
9. Kalovidouri A, Boto J, Vargas MI. Cerebral CSF cyst as a rare complication of ventriculoperitoneal shunt. J Neuroradiol. 2016. 43: 303-5
10. Karydakis P, Nikas I, Panagopoulos D, Filippidou M, Sfakianos G, Themistocleous M. Intraparenchymal pericatheter cyst after cerebrospinal fluid shunt: A rare complication with challenging diagnosis case presentation and review of the literature. Asian J Neurosurg. 2019. 14: 581-4
11. Merkler AE, Ch’ang J, Parker WE, Murthy SB, Kamel H. The rate of complications after ventriculoperitoneal shunt surgery. World Neurosurg. 2017. 98: 654-8
12. Mollan SP, Davies B, Silver NC, Shaw S, Mallucci CL, Wakerley BR. Idiopathic intracranial hypertension: Consensus guidelines on management. J Neurol Neurosurg Psychiatry. 2018. 89: 1088-100
13. Motomochi M, Nakata K, Shindoh H, Minami S, Fukami M, Ueda K. Case of reversible porencephalic cyst during malformation of VP shunts. Nerv Syst Child. 1987. 12: 147-50
14. Palmieri A, Pasquini U, Menichelli F, Salvolini U. Cerebral damage following ventricular shunt for infantile hydrocephalus evaluated by computed tomography. Neuroradiology. 1981. 21: 33-5
15. Park HJ, Lee SH, Park HJ, Shin SH. A porencephalic cyst formation in a 6-year-old female with a functioning ventriculoperitoneal shunt: A case-based review. Childs Nerv Syst. 2018. 34: 611-6
16. Rim HR, Hwang SK, Kwon SH, Kim HM. Intraparenchymal pericatheter cyst as a complication of a ventriculo-peritoneal shunt in a premature infant. J Korean Neurosurg Soc. 2011. 50: 143-6
17. Sakai N, Arai Y, Hirayama H. Malfuctioning ventricle-peritoneal shunt, associated with porencephaly. Nerv Syst Child. 1985. 10: 427-32
18. Sakai N, Yamanouchi Y, Numa Y, Matsumura H. Reversible porencephaly associated with shunt malfunction. Nerv Syst Child. 1989. 14: 365-8
19. Sakamoto H, Fujitani K, Kitano S, Murata K, Hakuba A. Cerebrospinal fluid edema associated with shunt obstruction. J Neurosurg. 1994. 81: 179-83
20. Santín-Amo JM, Rico-Cotelo M, Serramito-García R, Gelabert-González M, Allut AG. Cavidad porencefálica reversible secundaria a disfunción valvular [Reversible porencephalic cyst related to shunt dysfunction]. Rev Neurol. 2014. 58: 255-8
21. Shekawat JS, Sundar IV, Poonia N, Sinha VD. Intraparenchymal pericatheter cyst following ventriculoperitoneal shunt. Neurol India. 2012. 60: 341-2
22. Sinha AK, Lall R, Benson R, O’Brien DF, Buxton N. Intraparenchymal pericatheter cyst following ventriculoperitoneal shunt insertion: does it always merit shunt revision?. Zentralbl Neurochir. 2008. 69: 152-4
23. Sugimoto K, Enomoto T, Nose T. Reversible porencephaly. Alteration of the cerebrospinal fluid flow after shunt malfunction. Childs Nerv Syst. 1991. 7: 394-8
24. Vajramani GV, Fugleholm K. Reversible CSF cyst related to a functioning ventriculo-peritoneal shunt. Acta Neurochir (Wien). 2005. 147: 1199-202
25. Wallace DJ, Grandhi R. Intraparenchymal pericatheter cyst in ventriculoperitoneal shunt failure. BMJ Case Rep. 2017. 2017: bcr2017220468
26. Watkins JD, Lee J, Van Engen MJ, Tibbs ML, Ellegala DB, Nicholas JS. Isolated left homonymous hemianopia secondary to a pericatheter cyst-a rare presentation of a ventriculoperitoneal shunt failure. J Neuroophthalmol. 2015. 35: 60-4