- Department of Neurological Surgery, University of California, Sacramento, California, United States (Retired).
Correspondence Address:
Harry Sawyer Goldsmith, Department of Neurological Surgery, University of California, Sacramento, California, United States.
DOI:10.25259/SNI_1080_2022
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Goldsmith HS. Introduction of chemotherapy by omentum for a glioblastoma WHO-IV. Surg Neurol Int 17-Feb-2023;14:59
How to cite this URL: Goldsmith HS. Introduction of chemotherapy by omentum for a glioblastoma WHO-IV. Surg Neurol Int 17-Feb-2023;14:59. Available from: https://surgicalneurologyint.com/surgicalint-articles/12156/
THE PROBLEM
It is well acknowledged that glioblasts remain a major neurological problem that has existed for decades. When experiments with the omentum were begun in animals[
There are billions of capillaries throughout the body, but the only capillaries that have BBBs are those in the brain. Capillaries outside the brain are fenestrated (open) with endothelial cells that line the wall of these vessels. Throughout this wall of endothelial cells are open gaps that allow biological materials such as water, oxygen, and glucose to enter and exit throughout the body tissues. When these gaps are tight or blocked by specific BBB and BBTB capillaries, chemotherapy is prevented from entering the brain. If there is to be a successful chemotherapeutic treatment for glioblasts, BBB and BBTB capillaries must be bypassed or eliminated.
This paper proposes an operation that will allow the introduction of chemotherapeutic drugs into the brain of patients suffering from a glioblast. The operation requires the placement of the vascularized omentum into a prepared cavity in the brain, in which omental arteries can develop and subsequently penetrate directly and deeply into brain tissue. These omental arteries that enter the brain follow the progression of all arteries, namely, they branch into smaller vascular structures called arterioles which subsequently branch into smaller capillaries that connect the arterial-arterioles system in the body into smaller capillaries which advance blood flow from the heart into the general venous system. It is these specific capillaries in the brain that contain BBBs that prevent chemotherapy from entering the brain.
It had been hoped in the past that the administration of chemotherapeutic drugs offered to patients suffering from a glioblast would be clinically effective. Unfortunately, this did not occur. The BBBs within the brain prevent chemotherapeutic drugs from entering the brain. The operation proposed in this paper bypasses these BBBs.
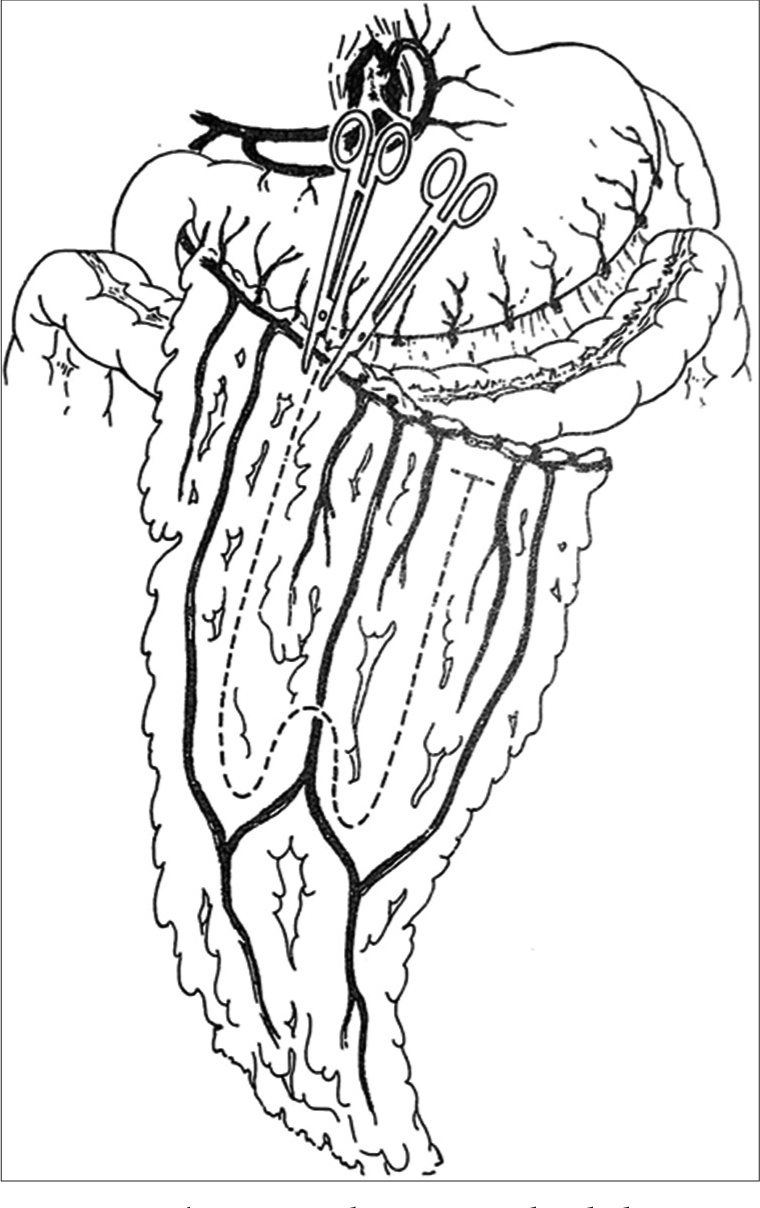
The first step in the operation is to become familiar with the intra-abdominal presence of the omentum. This is accomplished by making a 4–5-inch upper midline abdominal incision, which makes it easy to observe the placement of the omentum within the abdominal cavity. The technique to elongate the omentum up to the brain begins as follows: The omentum is completely separated from the transverse colon. This step is avascular and simple. This is followed by separating the omentum from its proximal and central attachments to the greater curvature of the stomach, leaving the gastroepiploic artery and vein intact within the omental apron. The left gastroepiploic vessels are then divided to increase omental length.
To gain length to reach the brain, the omentum is surgically tailored with care being taken to preserve intact at least one major artery and vein within the omental apron [
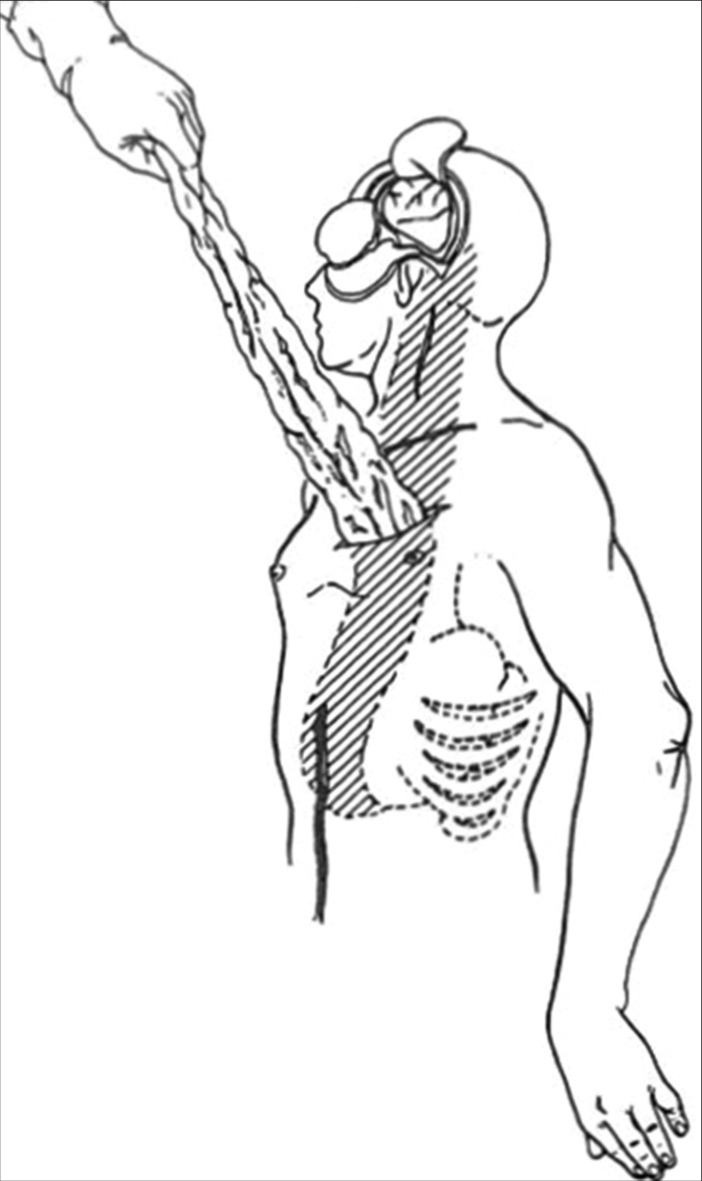
Once the omentum has been sufficiently lengthened to reach the brain without any tension, several small transverse incisions are made along the chest wall which is connected by a long longitudinal subcutaneous tunnel [
In the operation being proposed, the intact omentum is placed in a recently created brain cavity caused by the surgical excision of the glioblast. The omentum is key since it is the most angiogenic structure in the body, due to extensive amounts of vascular endothelial growth factor (VEGF) which is the most angiogenic substance in the body and its greatest concentration is found within the omentum itself.[
Before the surgery being proposed, the patient ingests aminovolumic acid (5-ALA) 3 h before the operative procedure.[
It is believed that this operation can improve the survival statistics of a glioblast, but the eventual success of the operation may depend on the strength of the chemotherapy that would be flowing into the brain through the omental arteries.
CONCLUSION
In the past, it was hoped that chemotherapy, when administered to patients with a glioblastoma, would be clinically improved by the use of these drugs. However, this did not occur as a result of BBB and BBTB capillaries that are specifically located only in the brain. It is now known that placement of the omental arteries in the brain of patients suffering from a glioblast, could allow chemotherapy to perfuse throughout the brain. Most important will be the strength of the chemotherapy that will be present in the omental capillaries that are devoid of BBB and BBTB vessels. Due to the lethality of glioblasts, it is hoped that clinical investigation of the effect of the placement of the omentum on the brain of glioblast patients will result in an experimental and clinical sense of urgency. For a patient with a glioblast, time is critical.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Goldsmith HS, Duckett S, Chen WF. Prevention of cerebral infarction in the dog by intact omentum. Am J Surg. 1975. 130: 317-20
2. Goldsmith HS, Duckett S, Chen WF. Prevention of cerebral infarction in the monkey by omental transposition to the brain. Stroke. 1978. 9: 224-9
3. Goldsmith HS, Saunder RL, Allen CD, Reeves AG, Milne J. Omental transposition to brain of stroke patients. Stroke. 1979. 10: 471-2
4. Goldsmith HS. Benefit of omental flow in Alzheimer’s disease: Effect of deteriorating neurons. J Alzheimer Dis. 2014. 42: S277-80
5. Goldsmith HS. Alzheimer disease can be treated: Why the delay?. Surg Neurol Int. 2017. 8: 133
6. Goldsmith HS. Blood brain barrier effect eliminated by omentum for the treatment of glioblastoma multiforme (WHO-IV). EC Neurol. 2018. 10: 928-32
7. Goldsmith HS. Potential improvement of survival statistics for a glioblastoma multiforme WHO-IV). Surg Neurol Int. 2019. 10: 123
8. Goldsmith HS. Alzheimer’s disease: A decreased cerebral blood flow to critical intraneuronal elements in the cause. J Alzheimer Dis. 2022. 85: 1419-22
9. Hockberg FH. Assumption in the radiotherapy of glioblastoma. Neurology. 1980. 30: 907-11
10. Koneiczny MJ, Song R, Georgia JR. Omental approach to functional recovery after cerebrovascular disease. World Neurosurg. 2015. 87: 406-16
11. Shankle WR, Hara J, Bjorsen I, Gade JF, Leport PC, Ali MB. Omental therapy for primary progressive aphasia with TAU negative histopathology: 3-years study. Neurol Res. 2009. 31: 766-9
12. Stummer W, Rodrigues F, Schucht P, Preuss M, Wiewrodt D, Nestler U. Predicting the usefulness of 5-ALA-derived tumor fluorescence for fluorescence-guided resections in pediatric brain tumors: A European survey. Acta Neurochir (Wien). 2014. 156: 2315-24
13. Zhang QK, Magovern MD, Mack CA, Budenbender KT, Ko W, Rosengart TK. Vascular endothelial growth factor is the major angiogenic factor in omentum: Mechanism of the omentum-mediated angiogenesis. J Surg Res. 1997. 67: 147-54