- Department of Neurosurgery, Arrazi Hospital, Mohammed VI University Hospital Center of Marrakesh, Cadi Ayyad University, Faculty of Medicine, Marrakesh, Morocco
Correspondence Address:
Malak El Marrakchi, Department of Neurosurgery, Arrazi Hospital, Mohammed VI University Hospital Center of Marrakesh, Cadi Ayyad University, Faculty of Medicine, Marrakesh, Morocco.
DOI:10.25259/SNI_670_2024
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Malak El Marrakchi, Nahla Zian, Meryem Ait Benali, Farouk Hajhouji, Said Ait Benali. Jael’s syndrome: Removal of a retained intracranial kitchen knife blade – A case report. 22-Nov-2024;15:427
How to cite this URL: Malak El Marrakchi, Nahla Zian, Meryem Ait Benali, Farouk Hajhouji, Said Ait Benali. Jael’s syndrome: Removal of a retained intracranial kitchen knife blade – A case report. 22-Nov-2024;15:427. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=13246
Abstract
Background: Jael’s syndrome is defined as an intentional injury caused by a knife in the skull or the face. It is a rare yet challenging situation in clinical practice. Initial triage is the key to optimal management.
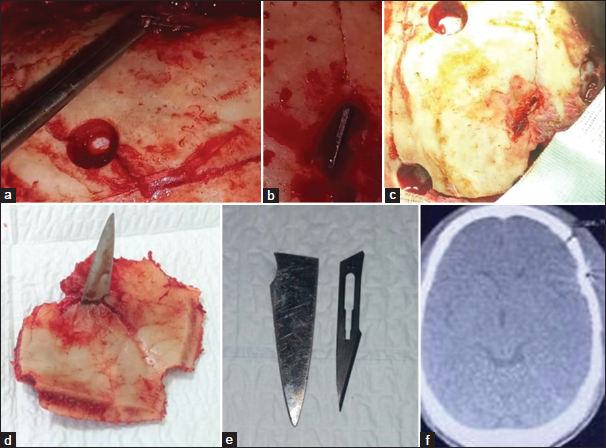
Case Description: We describe the case of a right-handed 30-year-old man presenting to the emergency for headaches 15 days after a stabbing attack into the skull using a kitchen knife. He was conscious with no neurological deficit or history of seizures. The wound had already healed. A cerebral computed tomography (CT) scan showed a retained kitchen knife blade. The stab wound extended through the temporal lobe and ended a few centimeters before the brainstem. The blade was removed under general anesthesia. Postoperative follow-up was satisfying without any neurological worsening. The control CT scan showed a remaining knife edge in the bone flap. It was decided to monitor the patient regularly, and he was discharged 3 days later.
Conclusion: This case highlights the medicolegal importance of physical examination and radiological exploration in penetrating head injury.
Keywords: Case report, Head, Jael’s syndrome, Knife blade, Penetrating trauma, Stab injury
INTRODUCTION
Penetrating brain injury (PBI) is a rare clinical entity. It carries high morbidity and mortality and often happens in adult male patients after a stabbing assault or a suicide attempt.[
Jefferson defined penetrating injury using a knife into the skull or the face as Jael’s syndrome in 1968.[
CASE REPORT
We describe the case of a right-handed 30-year-old patient with no medical history presenting to the emergency department for headaches 15 days after a penetrating head injury following a stabbing attack by a kitchen knife. The handle had broken at point-blank range. The patient was apyretic and conscious with no neurological deficit or history of seizures and the wound had already healed [
DISCUSSION
PBI is a life-threatening situation. It is mostly due to firearms.[
Initial assessment is crucial to triage. It depends mainly on clinical status. In some cases, surgery is performed immediately. Otherwise, patients need to undergo radiological exploration to assess the severity of the injury and overall prognosis. Magnetic resonance imaging is contraindicated in patients with metallic FBs. Head X-ray and CT scan remain available and rapidly performed. Objectifying vascular injury in the acute phase is essential using CT angiography.[
Complications following PBI could happen immediately after the trauma or later. They include hemorrhage, contusion, edema, infection, FB migration, cerebrospinal fluid leak, hydrocephalous, seizures, and vascular injuries like aneurysm, pseudoaneurysm, thrombus, dissection,[
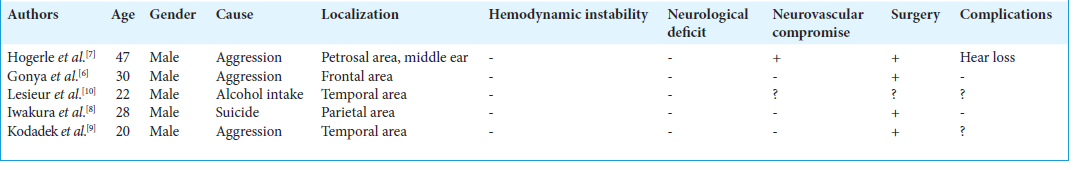
In fact, patients with retained intracranial knife blades have a higher risk of perioperative infection and vascular complications. Taylor et al. observed an increased incidence of vascular and infectious complications as well as mortality within the group of patients with retained transcranial knife blades. In addition to that, the handle break adds complexity to the problem since the blade constitutes evidence. Hence, this category of patients requires special attention and caution since the situation carries particular medicolegal implications.[
PBI is a vital emergency. The goal of treatment is resuscitation. Bleeding and high intracranial pressure should be controlled. Although triage is based mainly on clinical status, an indication for surgery is controversial. In fact, a Glasgow Coma Scale lower than 6 with fixed pupils is a factor of poor prognosis. In addition to that, radiological findings such as brainstem injury or deep localization should reconsider surgery since exploration or fragment retrieval could be harmful. It is highly recommended to perform surgery as soon as possible, preferably before 12 hours after trauma to reduce the risk of infection. Surgical practice depends on radiological patterns. In minor penetrating injuries, the goal is to extract the FB and perform debridement and removal of necrotic tissue, hematoma evacuation, hemostasis, and dura-mater plasty. Significant brain swelling is an indication of decompressive craniectomy.[
In Jael’s syndrome, “inline” removal is preferable. It depends mostly on how fixed the blade is. One of the used maneuvers is the application of vise grips to the protruding blade and using a mallet to pull the FB out in the direction of its insertion. Other surgeons perform a craniectomy or a craniotomy around the knife blade. For retained blades, Van Dellen and Lipschitz described a D-shaped craniectomy with the straight side against the blade to free it from the bone. However, it’s not clear witch technique (craniectomy or craniotomy) is best to achieve the optimal results and reduce the risk of operative complications.[
CONCLUSION
PBI is associated with high morbidity and mortality. Radiological exploration should be performed rapidly, when possible, without delaying resuscitation. Nevertheless, surgery is not always indicated. In Jael’s syndrome, “inline” removal is preferable.
Authors’ contributions
Dr. Malak El Marrakchi: Literature search, manuscript preparation, editing, and review. Dr. Nahla Zian: Literature search. Dr. Meryem Ait Benali: literature search. Pr. Farouk Hajhouji: manuscript review. Pr. Said Ait Benali: a manuscript review.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Abraham ZS, Lomnyack WP, Kimario OM, Kahinga AA. Jael’s syndrome: Case report and literature review. Int J Surg Case Rep. 2021. 88: 106484
2. Bhootra BL. Retained intra cranial blade-medicolegal perspectives. J Forensic Leg Med. 2007. 14: 31-4
3. De Lanerolle NC, Kim JH, Bandak FA. Neuropathology of traumatic brain injury: Comparison of penetrating, nonpenetrating direct impact and explosive blast etiologies. Semin Neurol. 2015. 35: 12-9
4. Deb S, Acosta J, Bridgeman A, Wang D, Kennedy S, Rhee P. Stab wounds to the head with intracranial penetration. J Trauma. 2000. 48: 1159-62
5. Fahde Y, Laghmari M, Skoumi M. Penetrating head trauma: 03 rare cases and literature review. Pan Afr Med J. 2017. 28: 305
6. Gonya S, Mbatha A, Moyeni N, Enicker B. (2016) Retained garden fork following cranial stab injury. J Surg Case Rep. 2016. p. rjv175
7. Högerle C, Nörenberg D, Biczok A, Kunz M, Baumeister P, Uhl B. (2022) Stab Injury of the Petrosal Bone: Case Report and Literature Review. Ear Nose Throat J. 101: NP431-NP435
8. Iwakura M, Kawaguchi T, Hosoda K, Shibata Y, Komatsu H, Yanagisawa A, Kohmura E. (2005) Knife blade penetrating stab wound to the brain--case report--. Neurol Med Chir (Tokyo). 45: 172-175
9. Kodadek LM, Leeper WR, Caplan JM, Molina C, Stevens KA, Colby GP. (2015) Retained transcranial knife blade with transection of the internal carotid artery treated by staged endovascular and surgical therapy: technical case report. Neurosurgery. 11: E372-375 discussion E375
10. Lesieur O, Verrier V, Lequeux B, Lempereur M, Picquenot E. Retained knife blade: An unusual cause for headache following massive alcohol intake. Emerg Med J. 2006. 23: e13
11. Loggini A, Vasenina VI, Mansour A, Das P, Horowitz PM, Goldenberg FD. Management of civilians with penetrating brain injury: A systematic review. J Crit Care. 2020. 56: 159-66
12. Mansour A, Loggini A, El Ammar F, Ginat D, Awad IA, Lazaridis C. Cerebrovascular complications in early survivors of civilian penetrating brain injury. Neurocrit Care. 2021. 34: 918-26
13. McKechnie J. A severe craniofacial impalement injury (Jael’s syndrome). Br J Oral Maxillofac Surg. 1986. 24: 258-64
14. Skarupa DJ, Khan M, Hsu A, Madbak FG, Ebler DJ, Yorkgitis B. Trends in civilian penetrating brain injury: A review of 26,871 patients. Am J Surg. 2019. 218: 255-60
15. Taylor AG, Peter JC. Patients with retained transcranial knife blades: A high-risk group. J Neurosurg. 1997. 87: 512-5
16. Vakil MT, Singh AK. A review of penetrating brain trauma: Epidemiology, pathophysiology, imaging assessment, complications, and treatment. Emerg Radiol. 2017. 24: 301-9