- Department of Neurosurgery, Hospital Civil “Dr. Juan I. Menchaca,” Guadalajara,
- Department of Health Sciences, Medical Surgeon Career Internship Program, Autonomous University of Guadalajara, Zapopan,
- Department of Radiology, Imaging and Diagnosis Center, Guadalajara, Jalisco, Mexico.
Correspondence Address:
Sergio Valente Esparza Gutiérrez, Department of Neurosurgery, Hospital Civil “Dr. Juan I. Menchaca,” Guadalajara, Jalisco, Mexico.
DOI:10.25259/SNI_501_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Adrián Santana Ramírez1, Sergio Valente Esparza Gutiérrez1, Pedro Avila Rodríguez1, Omar Alejandro Santana Ortiz2, Jesús Nicolás Serrano Heredia3. Juvenile angiolipoma in the subtemporal region, zygomatic, and pterygomaxillary fossa treated by microwave ablation – A case study and literature review. 09-Sep-2022;13:409
How to cite this URL: Adrián Santana Ramírez1, Sergio Valente Esparza Gutiérrez1, Pedro Avila Rodríguez1, Omar Alejandro Santana Ortiz2, Jesús Nicolás Serrano Heredia3. Juvenile angiolipoma in the subtemporal region, zygomatic, and pterygomaxillary fossa treated by microwave ablation – A case study and literature review. 09-Sep-2022;13:409. Available from: https://surgicalneurologyint.com/surgicalint-articles/11857/
Abstract
Background: Angiolipomas are benign mesenchymal tumors that infrequently affect the head-and-neck region and can appear with infiltrating and non-infiltrating forms. Surgical excision is the treatment of choice; however, there are other alternatives to manage this condition whose consideration is quite useful to evaluate per each particular case.
Case Description: An 11-year-old girl was diagnosed with non-infiltrating angiolipoma in the subtemporal region, the zygomatic, and pterygomaxillary fossa; she had a history of having undergone surgery on two previous occasions with a failed resection attempt due to the high vascularization of the injury and significant transoperative bleeding. The condition was managed with minimally invasive techniques through microwave ablation, requiring two sessions, achieving very satisfactory results both esthetically and in the final size of the lesion.
Conclusion: The microwave ablation technique may turn out to be a very useful tool for the management of lesions with high vascularization such as angiolipoma. This technique offers a new possibility for initial management, both independent of and complementary to other management techniques for other lesions at the base of the skull and/or facial massif regions.
Keywords: Angiolipoma, Lipoma, Microwave ablation
INTRODUCTION
Angiolipomas are benign mesenchymal tumors that infrequently affect the head-and-neck region and can appear with infiltrating and non-infiltrating forms. Surgical excision is the treatment of choice; however, there are other alternatives to manage this condition whose consideration is quite useful to evaluate per each particular case. We describe a case of non-infiltrating angiolipoma involving the subtemporal region, the zygomatic fossa, and the pterygomaxillary region on the right side. The effect of its volume deformed bone structures and adjacent soft tissues, with noticeable facial deformity. The patient underwent treatment on two occasions, with a failed attempt at surgical resection with a maxillofacial operation due to a high degree of vascularity and intraoperative bleeding. Given the history of high vascularization, it was decided to manage the tumor ablation using ultrasound-guided microwaves. This required the patient to undergo two ablation sessions to achieve acceptable results, both esthetic and in terms of tumor volume.
CASE STUDY
An 11-year-old female patient had a progressive increase in volume in the cheek region on the right side. This condition was noticed by the mother of the patient at the age of 10 years and was accompanied by mild local pain on palpation and with chewing, as well as with limited opening of the mandible. The patient was initially seen by the department which twice performed the maxillofacial operation which involved a failed resection attempt due to high bleeding liability. Procedures involved performing a linear suprazygomatic incision, vertical on the right side, 1 cm in front of the tragus, achieving a biopsy for histopathological study and where angiolipoma was reported.
Magnetic resonance studies were evaluated where, when a considerable extension of the lesion is observed, from the zygomatic fossa to the pterygomaxillary, with displacement of the masseter muscle [
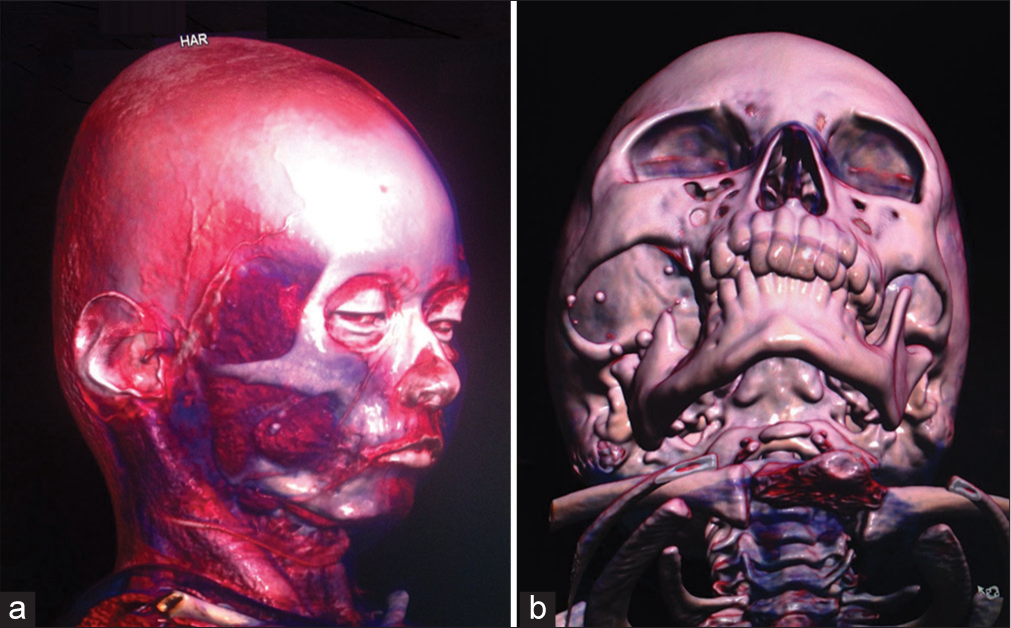
Figure 1:
3D-Volume Rendering of tomography study reconstruction. (a) Anterolateral view with image of soft tissue, a transspatial tumor is demonstrated in the right subtemporal region with extension to the zygomatic and pterygomaxillary fossae, deep in the masseter muscle. (b) Anteroinferior view with bone image: Facial asymmetry is demonstrated with increased width of the zygomatic fossa, anterior displacement, and thinning of the right zygomatic process. As with remodeling of the mandibular ramus, there is no alteration of the cortical bone.
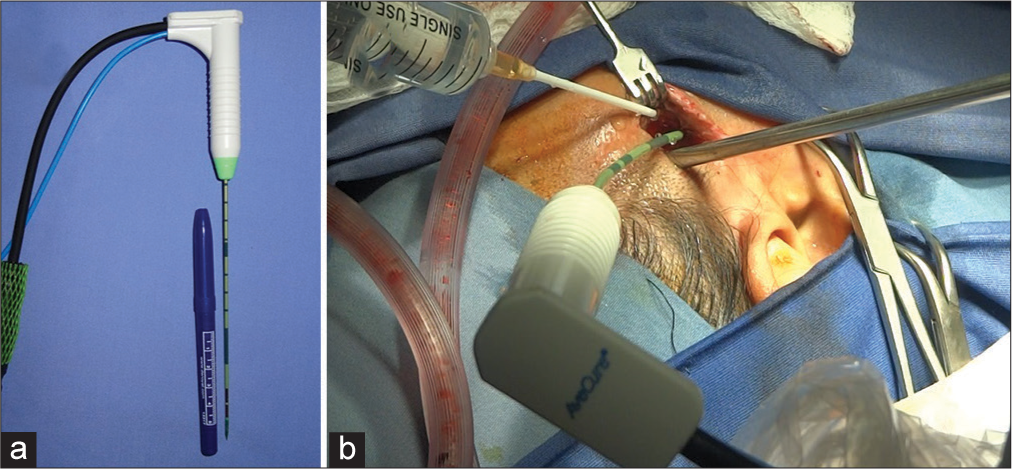
The first procedure involved a suprazygomatic incision where a biopsy was taken for histopathological study and ablation of the suprazygomatic portion of the lesion was realized [
DISCUSSION
Angiolipomas as histological variants of lipoma are benign mesenchymal tumors composed of mature lipocytes and blood vessels.[
Angiolipomas most commonly affect young male patients, accounting for approximately 6–17% of all lipomas.[
Based on the studies performed, angiolipomas can be divided into two types, infiltrating and non-infiltrating.[
The diagnosis of angiolipoma is based on both clinical and histopathological examination. Ultrasonography, magnetic resonance imaging, and fine-needle aspiration cytology can be useful in the diagnosis of angiolipoma.[
Treatment for non-infiltrating angiolipoma is enucleation, while for infiltrating angiolipoma a wide excision should be performed to include surrounding normal tissue. In cases of recurrence or inadequate resection, radiotherapy should be pursued;[
It is our judgment that the thermal effect of the microwave ablation shows two important phases: (1) The damage caused by hyperthermia, which generates an inflammatory process with a higher peak between 72 h and 7 days after ablation, with the consequent progressive decrease in edema and swelling and (2) in the medium term a second phase, characterized by a progressive reduction in the volume of the lesion (the latter, as shown by the evolution both in facial aspects and in magnetic resonance images [
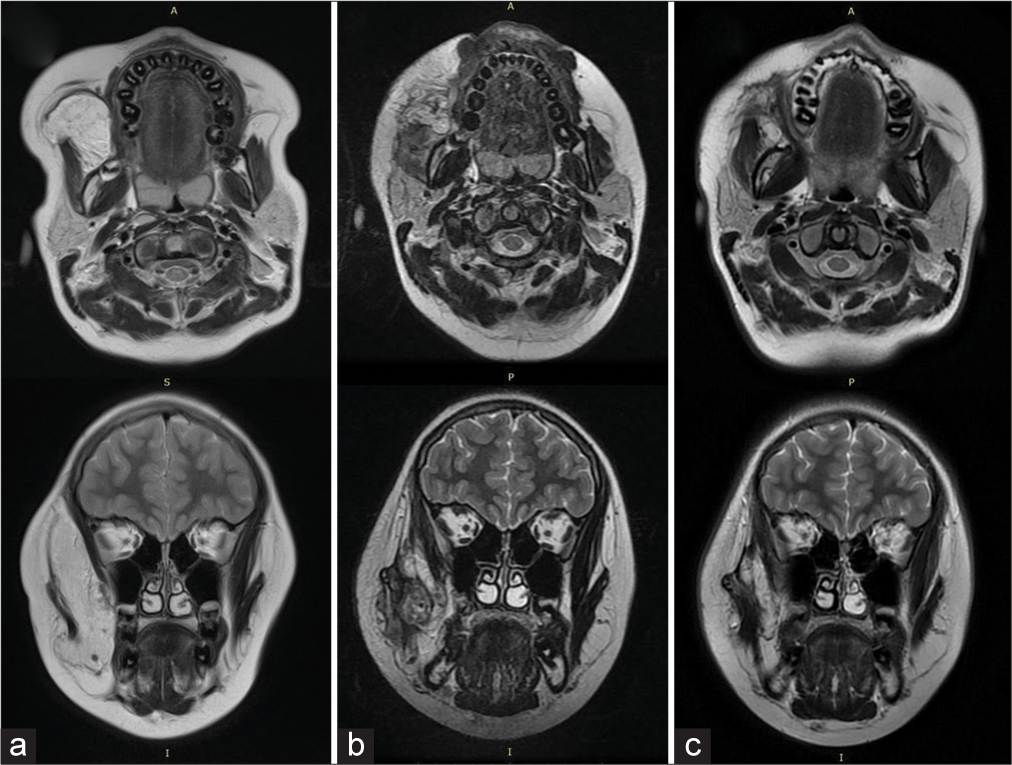
Figure 3:
T2-enhanced magnetic resonance images in the axial and coronal sections, where the changes were observed during the care of the ablation, are shown here sequentially. (a) A basal study shows a lesion with intensity similar to that of fatty tissue in the right masticatory space that displaces the masseter muscle. This lesion extends toward the zygomatic and pterygomaxillary fossa regions, involving an increase in the volume of said area prior to ablation. (b) Control study 5 months after ablation (c) Same sequences 1 year and 9 months after ablation: Note the decreased volume of the tumor and the presence of hypointense fibrous scar tissue.
In general, recurrences are very rare. The exception is for infiltrating angiolipoma, which has a recurrence rate of 35–50%.[
CONCLUSION
The subtemporal, pterygomaxillary, and facial region is an area that is also the responsibility of neurosurgery as part of skull base surgery.
Management of highly vascularized lesions that jeopardize this area with conventional techniques involve a high possibility of damage to structures, such as to the temporomandibular joints, to temporal muscle and trigeminal and facial nerves, as well as involving blood loss. Microwave ablation is a new technique in neurosurgery which is already used by the authors in the treatment of intracranial tumors and of the skull base. Patients with these types of conditions could benefit from avoiding many of the aforementioned complications, considering a minimally invasive technique which can be applied repeatedly such as in the present case.
In the case of other types of extracranial lesions, new studies are necessary to further demonstrate the effects generated by this type of ablation.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Akyüz C, Emir S, Büyükpamukçu M, Büyükpamukçu N, Cağlar M, Kale G. Successful treatment with interferon alfa in infiltrating angiolipoma: A case presenting with Kasabach-Merritt syndrome. Arch Dis Child. 2003. 88: 67-8
2. Altug HA, Sahin S, Sencimen M, Dogan N, Erdogan O. Noninfiltrating angiolipoma of the cheek: A case report and review of the literature. J Oral Sci. 2009. 51: 137-9
3. Bua AJ, Luáces R, Franco FL, García-Rozado Á, Escudero JL, Capdevila EF. Angiolipoma in head and neck: Report of two cases and review of the literature. Int J Oral Maxillofac Surg. 2010. 39: 610-5
4. Carrafiello G, Laganà D, Mangini M, Fontana F, Dionigi G, Boni L. Microwave tumors ablation: Principles, clinical applications and review of preliminary experiences. Int J Surg. 2008. 6: S65-9
5. Cassoni A, Romano A, Terenzi V, Bartoli D, Buonaccorsi S, Valentini V. Intramasseterin-infiltrating angiolipoma: A challenging diagnosis. J Craniofac Surg. 2012. 23: e290-2
6. Gonzalez-Crussi F, Enneking WF, Arean VM. Infiltrating angiolipoma. J Bone Joint Surg Am. 1966. 48: 1111-24
7. Lin JJ, Lin F. Two entities in angiolipoma. A study of 459 cases of lipoma with review of literature on infiltrating angiolipoma. Cancer. 1974. 34: 720-7
8. Louis DN, Ohgaki H, Wiestier OD, Cavenee WK, Ellison DW, Perry A.editors. WHO Classification of Tumours of the Central Nervous System. Lyon Cedex France: International Agency for Reserch on Cancer; 2016. p. 260
9. Ozaki T, Mori I, Nakamura M, Utsunomiya H, Tabuse K, Kakudo K. Microwave cell death: Immunohistochemical and enzyme histochemical evaluation. Pathol Int. 2003. 53: 686-92
10. Palaia G, Gaimari G, Giudice RL, Galanakis A, Tenore G, Romeo U. Excision of an oral angiolipoma by KTP laser: A case report. Ann Stomatol (Roma). 2011. 2: 28-31
11. Rai D, Verma S. Angiolipoma larynx: A case report. Indian J Otolaryngol Head Neck Surg. 2011. 63: 384-6
12. Ramírez AS, Rodriguez PA, Gutiérrez SV, Avila OG. Preliminary experience in the management of brain and skull-base tumors with microwave ablation; Feasibility guided by ultrasound, report from 23 cases. Surg Neurol Int. 2019. 10: 17
13. Shah VS, Harish M, Patel JR, Shah N. Infiltrating angiolipoma of the cheek. BMJ Case Rep. 2013. 2013: bcr2013200041
14. Shahi AK, Ash H, Chatterji K, Singh R. Cellular infiltrative angiolipoma of cheek in an infant. Natl J Maxillofac Surg. 2014. 5: 202-5