- Department of Neurosurgery, AHEPA, University General Hospital, Aristotle University of Thessaloniki, Thessaloniki, Greece
- Lab of Medical Physics, Faculty of Medicine, School of Health Sciences, Aristotle University of Thessaloniki, Thessaloniki, Greece
Correspondence Address:
Alkinoos Athanasiou
Department of Neurosurgery, AHEPA, University General Hospital, Aristotle University of Thessaloniki, Thessaloniki, Greece
DOI:10.4103/sni.sni_299_17
Copyright: © 2017 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Alkinoos Athanasiou, Ioannis Balogiannis, Ioannis Magras. Lasting bilateral mydriasis after traumatic brain injury may not always be a lost case. 26-Sep-2017;8:229
How to cite this URL: Alkinoos Athanasiou, Ioannis Balogiannis, Ioannis Magras. Lasting bilateral mydriasis after traumatic brain injury may not always be a lost case. 26-Sep-2017;8:229. Available from: http://surgicalneurologyint.com/surgicalint-articles/lasting-bilateral-mydriasis-after-traumatic-brain-injury-may-not-always-be-a-lost-case/
Abstract
Background:Lasting bilateral mydriasis and absence of pupillary light reflex following severe traumatic brain injury (TBI) are considered signs of irreversible brainstem damage and have been strongly associated with poor outcome.
Case Description:A young female patient presented with severe TBI, contusions, and diffuse brain edema. She was initially treated medically, but developed delayed secondary refractory intracranial hypertension and bilaterally dilated, non-reactive pupils for 12 h. Wide decompressive craniectomy and dural incisions were performed. The patient presented gradual improvement in her clinical condition [Glasgow Coma Scale (GCS) 13/15]. Delayed recurring infections lead to the patient's death due to sepsis after 3 months.
Conclusion:In light of recent studies, lasting bilateral mydriasis may not always be considered a decisive factor for non-escalation of treatment, as variability among TBI patients and outcomes has been demonstrated. Wide decompressive craniectomy is viable for controlling refractory intracranial hypertension in hemodynamically stable patients.
Keywords: Brain edema, decompressive craniectomy, dilated pupils, intracranial hypertension, traumatic brain injury
INTRODUCTION
Lasting bilaterally dilated and unreactive pupils after a severe traumatic brain injury (TBI) are usually considered a sign of irreversible brainstem damage and have been strongly associated with a very poor outcome (death, vegetative state, or severe disability) in the majority of patients.[
A mark of 6 h of lasting bilateral mydriasis has been considered an almost definite prognostic factor for mortality of those patients;[
Hereby, we present a case of short-term recovery by a young patient that presented secondary intracranial hypertension following TBI and was treated with decompressive craniectomy after 12 h of fixated dilated pupils. We discuss on the possible significance of this previously unreported, to our best knowledge, outcome.
CASE HISTORY
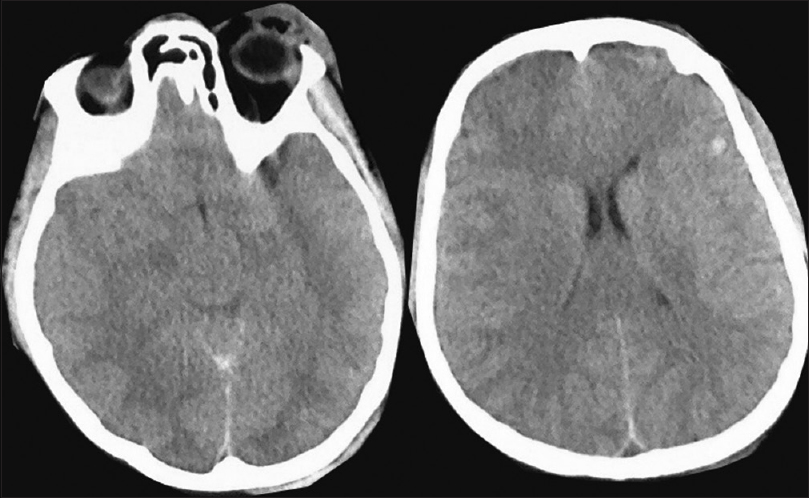
A 19-year-old woman was admitted comatose at the Emergency Department after a fall from a motorbike (reported low speed but no helmet) with severe TBI. She presented with a GCS of 5/15 (by component: Eyes 1, verbal 2, and motor 2) and 3 mm non-reactive pupils bilaterally. The computed tomography (CT) brain scan at admission showed few left frontal and temporal contusions, a small left frontal epidural hematoma and diffuse brain edema [
The patient was intubated and admitted to the intensive care unit (ICU) after placement of an intraparenchymal catheter for measuring and managing of intracranial pressure (ICP) [
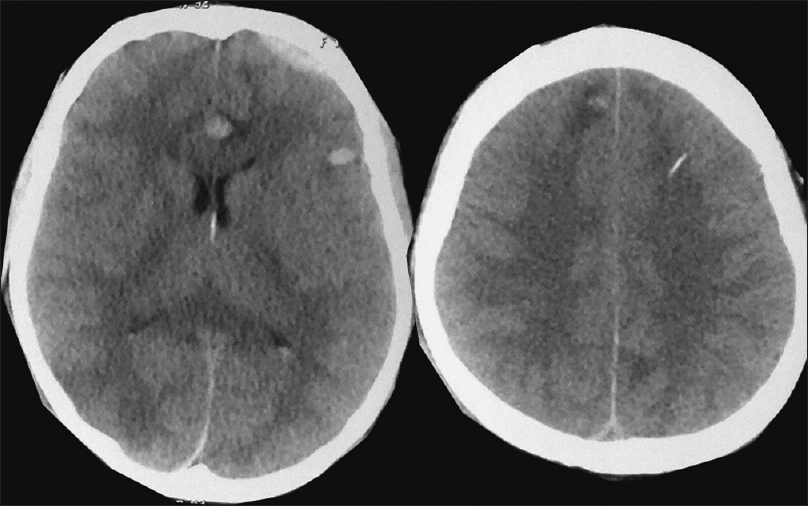
On the afternoon of the 7th post-injury day, while in ICU care, the patient presented an increase in ICP (>25 mmHg with surges of >30) and bilateral non-reactive mydriasis (7 mm). Initial decision was for conservative treatment using mannitol, hyperventilation, and barbiturate coma that controlled the ICP in a range of 17–27 mmHg, but[
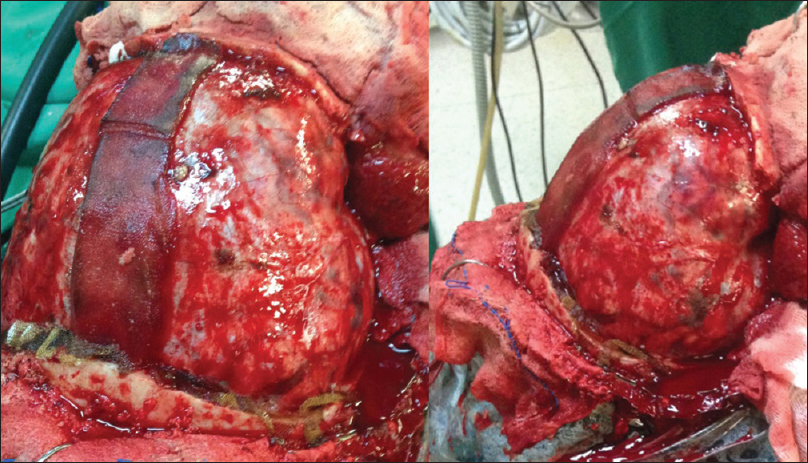
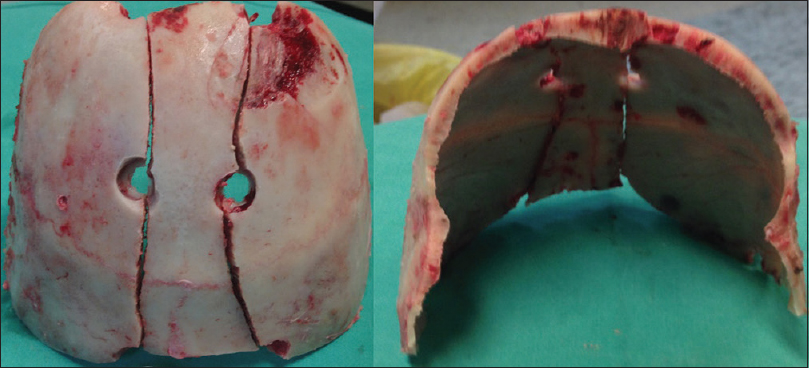
The pupils were checked immediately before the operation, but no recovery was observed. The patient was then operated using a wide decompressive craniectomy that encompassed bilaterally frontal and temporal areas, and extended as far as possible in the parietal bone. No bony bridge was left above the superior sagittal sinus in the area of the craniectomy; undercutting and smoothing was also performed at the edge of the parietal bone. Furthermore, due to excessive swelling of the underlying brain, we decided to perform dural incisions instead of flap durotomy [Figures
Figure 3
Intraoperative photo of the patient's brain (swollen) immediately after the craniectomy, before dural incision. Despite the wide craniectomy and decompression our impression was that dural opening would cause bilateral encephalocele, so the decision was to perform multiple dural incisions instead
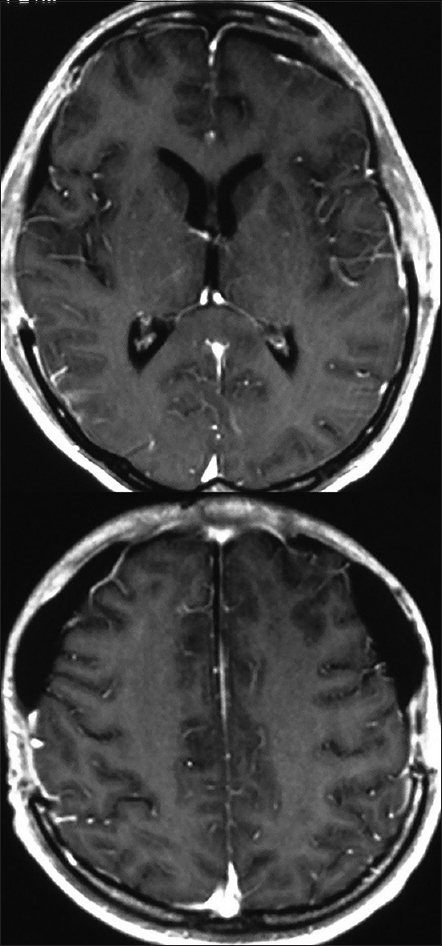
While immediately postoperatively the patient pupils did not change, the patient's condition presented gradual improvement over the period of the next 3 weeks. She was able to be decommitted from mechanical ventilation, be transported back to the neurosurgical ward and commence physiotherapy, and active kinesiotherapy. The patient's tracheostomy was removed and the patient's outcome at 1 month post-injury was at Glasgow Outcome Scale (GOS) 4 (moderate disability), reaching a GCS of 13/15 (by component: eyes 4, verbal 3, and motor 6). A 1-month post-injury magnetic resonance imaging (MRI) scan also showed significant improvement of the intracranial lesions [
The patient's significant improvement was halted by complications in the form of delayed recurring refractory infections (pulmonary and systematic sepsis) and her clinical status gradually deteriorated, leading to her death due to sepsis after 3 months (ultimately GOS 1) despite combined management with the hospital's infections team.
DISCUSSION
Lasting bilaterally fixated pupils has been proposed as a decisive factor for non-escalation of treatment.[
A known study has evaluated the effect of mydriasis duration on the outcoume of TBI patients treated with craniotomy.[
The aggressive surgical management (wide decompressive craniectomy) has been shown to benefit patients with delayed or refractory intracranial hypertension after severe TBI,[
CONCLUSION
The presence of lasting bilateral mydriasis should not always be considered a decisive factor for non-escalation of treatment.[
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Bahloul M, Ben Hamida C, Chelly H, Chaari A, Kallel H, Dammak H. Severe head injury among children: Prognostic factors and outcome. Injury. 2009. 40: 535-40
2. Chaudhuri K, Malham GM, Rosenfeld JV. Survival of trauma patients with coma and bilateral fixed dilated pupils. Injury. 2009. 40: 28-32
3. Chen JW, Vakil-Gilani K, Williamson KL, Cecil S. Infrared pupillometry, the Neurological Pupil index and unilateral pupillary dilation after traumatic brain injury: Implications for treatment paradigms. Springerplus. 2014. 3: 548-
4. Chieregato A, Venditto A, Russo E, Martino C, Bini G. Aggressive medical management of acute traumatic subdural hematomas before emergency craniotomy in patients presenting with bilateral unreactive pupils. A cohort study. Acta Neurochir (Wien). 2017. 159: 1553-9
5. Helmy A, Kirkpatrick PJ, Seeley HM, Corteen E, Menon DK, Hutchinson PJ. Fixed, dilated pupils following traumatic brain injury: Historical perspectives, causes and ophthalmological sequelae. Acta Neurochir Suppl. 2012. 114: 295-9
6. Hutchinson PJ, Corteen E, Czosnyka M, Mendelow AD, Menon DK, Mitchell P. Decompressive craniectomy in traumatic brain injury: The randomized multicenter RESCUEicp study (www.RESCUEicp.com). Acta Neurochir. 2006. 96: 17-20
7. Hutchinson PJ, Timofeev I, Kirkpatrick P. Surgery for Brain Edema. Neurosurg Focus. 2007. 22: E14-
8. Kolias AG, Adams H, Timofeev I, Czosnyka M, Corteen EA, Pickard JD. Decompressive craniectomy following traumatic brain injury: Developing the evidence base. Br J Neurosurg. 2016. 30: 246-50
9. Kontopoulos V, Foroglou N, Patsalas J, Magras J, Foroglou G, Yiannakou-Pephtoulidou M. Decompressive craniectomy for the management of patients with refractory hypertension: Should it be reconsidered?. Acta Neurochir. 2002. 144: 791-6
10. Marmarou A, Lu J, Butcher I, McHugh GS, Murray GD, Steyerberg EW. Prognostic value of the Glasgow Coma Scale and pupil reactivity in traumatic brain injury assessed pre-hospital and on enrollment: An IMPACT analysis. J Neurotrauma. 2007. 24: 270-80
11. Morgalla MH, Will BE, Roser F, Tatagiba M. Do long-term results justify decompressive craniectomy after severe traumatic brain injury?. J Neurosurg. 2008. 109: 685-90
12. Moscote-Salazar LR, Alvis-Miranda HR, Palencia C, M Rubiano A. emergent decompressive craniectomy in patients with fixed dilated pupils; a single center experience. Bull Emerg Trauma. 2013. 1: 175-8
13. Saade N, Veiga JC, Cannoni LF, Haddad L, Araújo JL. Evaluation of prognostic factors of decompressive craniectomy in the treatment of severe traumatic brain injury. Rev Col Bras Cir. 2014. 41: 256-62
14. Sahuquillo J, Arikan F. Decompressive craniectomy for the treatment of refractory high intracranial pressure in traumatic brain injury. Cochrane Database Syst Rev. 2006. 25: CD003983-
15. Sakas DE, Bullock MR, Teasdale GM. One-year outcome following craniotomy for traumatic hematoma in patients with fixed dilated pupils. J Neurosurg. 1995. 82: 961-5
16. Schneider GH, Bardt T, Lanksch WR, Unterberg A. Decompressive craniectomy following traumatic brain injury: ICP, CPP and neurological outcome. Acta Neurochir Suppl. 2002. 81: 77-9
17. Whicield PC, Patel H, Hutchinson PJ, Czosnyka M, Parry D, Menon D. Bifrontal decompressive craniectomy in the management of posttraumatic intracranial hypertension. Br J Neurosurg. 2001. 15: 500-7
18. Yatsushige H, Takasato Y, Masaoka H, Hayakawa T, Otani N, Yoshino Y. Prognosis for severe traumatic brain injury patients treated with bilateral decompressive craniectomy. Acta Neurochir Suppl. 2010. 106: 265-70