- Department of Neurosurgery, Kobe University Graduate School of Medicine, Kobe, Japan.
Correspondence Address:
Young Ju Kim, Department of Neurosurgery, Kobe University Graduate School of Medicine, Kobe, Japan.
DOI:10.25259/SNI_742_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Young Ju Kim, Atsushi Fujita, Masahiro Maeyama, Tatsuo Hori, Kazuhiro Tanaka, Takashi Sasayama. Late intrathecal retraction of a lumboperitoneal shunt. 08-Dec-2023;14:417
How to cite this URL: Young Ju Kim, Atsushi Fujita, Masahiro Maeyama, Tatsuo Hori, Kazuhiro Tanaka, Takashi Sasayama. Late intrathecal retraction of a lumboperitoneal shunt. 08-Dec-2023;14:417. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=12662
Abstract
Background: Lumboperitoneal (LP) shunt placement is a good option for treating elderly patients with communicating normal pressure hydrocephalus (NPH) who are also on antiplatelet therapy following endovascular treatment of unruptured bilateral internal carotid artery aneurysms. Here, in an 80-year-old male with an LP shunt, the catheter was “pinched” between adjacent spinous processes, resulting in laceration of the catheter and intrathecal catheter migration.
Case Description: An 80-year-old male was treated with a LP shunt for NPH 1 year after undergoing endovascular treatment of unruptured bilateral internal carotid artery aneurysms. The lumbar catheter was placed at the L2–3 level. Six months later, when he clinically deteriorated, the follow-up computed tomography showed recurrent ventricular enlargement. Further, studies additionally confirmed intrathecal migration of the lumbar catheter, warranting secondary ventriculoperitoneal shunt placement.
Conclusion: Patients with LP shunts may develop lumbar catheter lacerations secondary to a “pinching” effect from adjacent spinous processes, resulting in intrathecal catheter migration.
Keywords: Catheter rupture, Idiopathic normal pressure hydrocephalus, Intrathecal migration, Lumboperitoneal shunt, Ventricular shunt
INTRODUCTION
Lumboperitoneal (LP) shunts are good alternatives to ventriculoperitoneal (VP) shunts for patients requiring antiplatelet therapy. Here, one year following endovascular treatment of unruptured bilateral intracranial aneurysms, an 80-year-old patient developed idiopathic normal pressure hydrocephalus (NPH). He initially underwent placement of an LP shunt to avoid the increased hemorrhagic risks of a VP shunt. However, when the catheter became “pinched”/lacerated by the adjacent spinous processes and migrated intrathecally, he ultimately required a VP shunt.
CASE REPORT
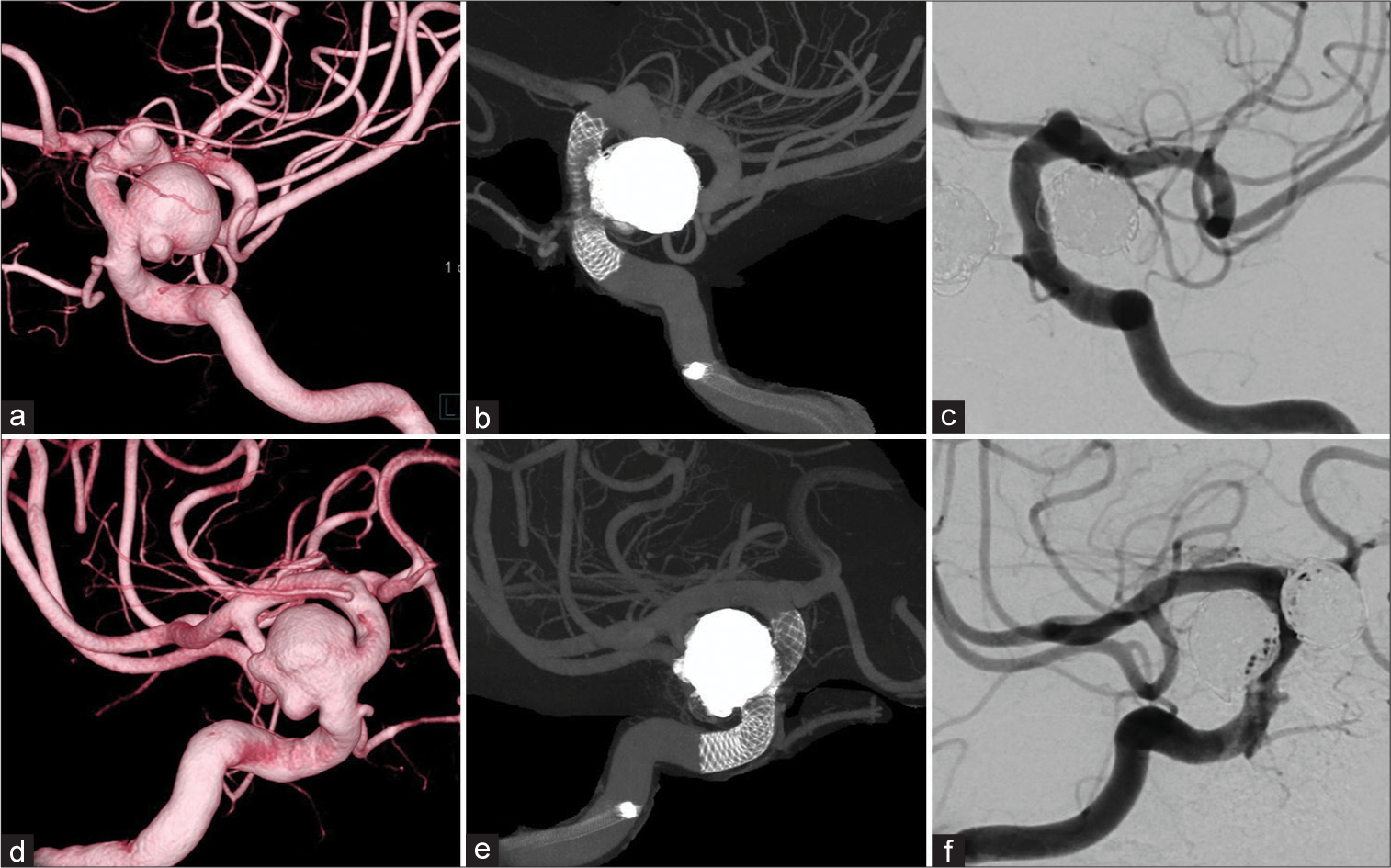
An 80-year-old male underwent coiling of bilateral carotid artery aneurysms [
Figure 1:
Angiography after flow diverter placement with coiling of bilateral carotid artery aneurysms. (ac) Left internal carotid artery. (d-f) Right internal carotid artery. (a and d) Three-dimensional rotational angiography. (b and e) Cone-beam computed tomography. (c and f) Angiography at the 6-month follow-up.
Figure 2:
Perioperative lumbar images when lumboperitoneal (LP) shunt placed. (a) computed tomography showed no scoliosis, hypertrophy of spinous processes, and/or marked calcification of interspinous ligament. (b) X-ray after LP shunt placement. (c) showed a shunt catheter inserted cephalad through the L2–L3 level.
Postoperative course
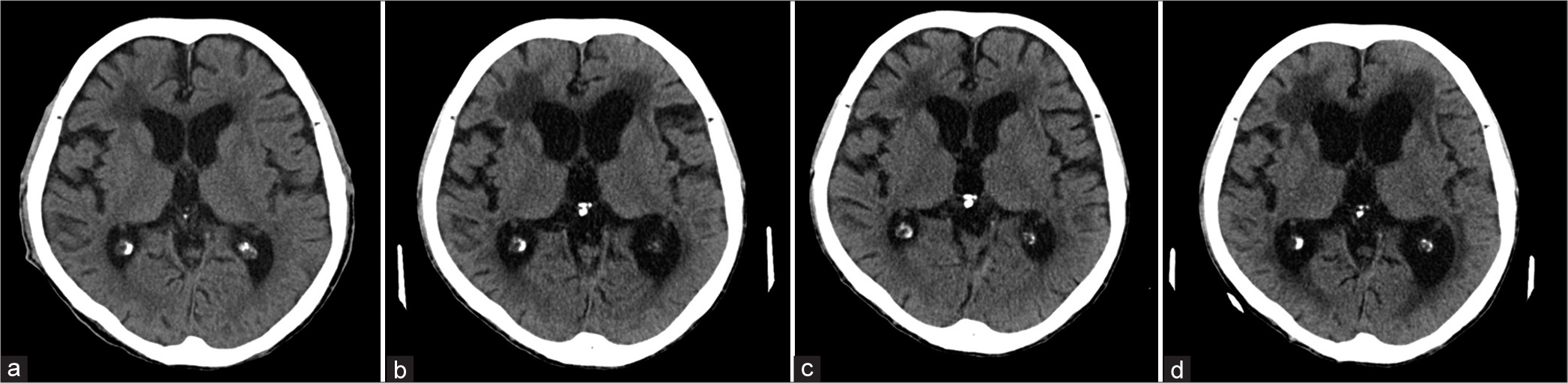
Postoperatively, his gait/cognitive function improved, and the ventricles decreased in size. However, six months later, symptoms recurred, and the CT once again showed enlarged ventricles/ periventricular lucency, plus L2 intrathecal migration of the lumbar catheter [
Figure 3:
Brain computed tomography (CT). (a) Preoperative-flow diverters. (b) CT Image after recurrent worsening of normal pressure hydrocephalus symptoms/signs following bilateral flow diverter placement; enlarged lateral ventricles/periventricular lucency-anterior horns. (c) Image when symptoms improved after lumboperitoneal shunt. (d) Six months later, the patient deteriorated.
DISCUSSION
Incidence of LP shunt intrathecal retraction/migration
An 80-year-old male developed a 6-month delayed rupture of an LP shunt catheter that was originally placed at the L2/L3 level (i.e., migrated intrathecally). Catheter rupture is described in <1% of patients following LP shunt surgery.[
Choice to initially place an LP shunt, followed secondarily by a VP shunt
We chose to place an LP shunt rather than a VP shunt as our patient was on dual antiplatelet therapy following endovascular treatment of unruptured bilateral internal carotid artery aneurysms. Hudson et al. reported that such patients are at increased risk for intracranial hemorrhages following VP shunt placement.[
CONCLUSION
Multiple factors go into choosing an LP rather than a VP shunt for treating elderly patients with NPH. Obtaining preoperative CT studies to document sufficient interspinous space/distance may avoid future lumbar proximal catheter lacerations and intrathecal retraction.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. AlBakry A, Taha MM, Al Menshawy HA. Cranial migration of lumboperitoneal shunt: A case report and review of literature. Surg Neurol Int. 2019. 10: 124
2. Hudson JS, Nagahama Y, Nakagawa D, Starke RM, Dlouhy BJ, Torner JC. Hemorrhage associated with ventriculoperitoneal shunt placement in aneurysmal subarachnoid hemorrhage patients on a regimen of dual antiplatelet therapy: A retrospective analysis. J Neurosurg. 2018. 129: 916-21
3. Jusue-Torres I, Lu J, Robison J, Hoffberger J, Wemmer J, Sanyal A. Diagnostic assessment of adult hydrocephalus log compared to standard normal pressure hydrocephalus diagnostic tools. Fluids Barriers CNS. 2015. 12: O44
4. Kazui H, Miyajima M, Mori E, Ishikawa M, SINPHONI-2 Investigators. Lumboperitoneal shunt surgery for idiopathic normal pressure hydrocephalus (SINPHONI-2): An open-label randomised trial. Lancet Neurol. 2015. 14: 585-94
5. Kikuchi A, Maegawa T, Arai N, Yamazaki K, Arai N, Chernov M. Broken lumboperitoneal shunt with intra-thecal migration of the lumbar catheter in a patient with idiopathic normal pressure hydrocephalus: Case report. Curr Pract Neurosurg. 2021. 31: e12-8
6. Tucker A, Kajimoto Y, Ohmura T, Ikeda N, Furuse M, Nonoguchi N. Fluoroscopic-guided paramedian approach for lumbar catheter placement in cerebrospinal fluid shunting: Assessment of safety and accuracy. Oper Neurosurg (Hagerstown). 2019. 16: 471-7