- Department of Neurosurgery, Krankenhaus Barmherzige Brüder, Regensburg, Germany
- Department for Trauma, Orthopaedics and Sports Medicine, Krankenhaus Barmherzige Brüder, Regensburg, Germany
- Department of Vascular Surgery, Krankenhaus Barmherzige Brüder, Regensburg, Germany
- Pathological-Anatomical Institute, Regensburg, Germany
Correspondence Address:
Stephan Lackermair, Department of Neurosurgery, Krankenhaus Barmherzige Brüder, Regensburg, Germany.
DOI:10.25259/SNI_132_2024
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Stephan Lackermair1, Hannes Egermann1, Franz Müller2, Ingolf Töpel3, Jozef Zustin4, Adolf Mülle1. Local compression of the sciatic nerve by a vascular malformation as a rare cause of sciatica: A case report and review of literature. 19-Apr-2024;15:139
How to cite this URL: Stephan Lackermair1, Hannes Egermann1, Franz Müller2, Ingolf Töpel3, Jozef Zustin4, Adolf Mülle1. Local compression of the sciatic nerve by a vascular malformation as a rare cause of sciatica: A case report and review of literature. 19-Apr-2024;15:139. Available from: https://surgicalneurologyint.com/surgicalint-articles/12861/
Abstract
Background: Sciatica is typically caused by disc herniations or spinal stenosis. Extraspinal compression of the sciatic nerve is less frequent.
Case Description: We report a rare case of sciatica with compression of the sciatic nerve by a low-flow vascular malformation in a 24-year-old female patient. The special feature of this case was sciatica along the S1 dermatome, which only occurred in the sitting position and inclination because of compression of the sciatic nerve between the vascular malformation and the lesser trochanter. Spinal imaging showed no abnormal findings. Surgery was performed interdisciplinary and included neurosurgery, vascular surgery, and trauma surgery. After surgery, the patient became symptom-free.
Conclusion: Rare and extraspinal causes of local compression of the sciatic nerve should be considered, especially in cases of lacking spinal imaging correlation and untypical clinical presentation. Interdisciplinary surgical cooperation is of special value in cases of rare entities and uncommon locations.
Keywords: Compression sciatic nerve, Sciatica, Vascular malformation
INTRODUCTION
Sciatica is pain that radiates from the buttock downward along the course of the sciatic nerve.[
CASE DESCRIPTION
History and examination
A 24-year-old female patient presented with a 3-month history of intermittent paraesthesia and paresis in the left leg. The symptoms were mostly exacerbated by exercise. Especially while walking, the patient reported lumbago and pain in the left groin, left ventral proximal thigh, and partially lower abdomen. The special feature of this case was sciatica along the S1 dermatome, which only occurred in the sitting position and inclination. The pain was described as lasting for several minutes.
In clinical neurological examination, hip flexion on the left side scored 4/5 on the Medical Research Council (MRC) power scale, most likely due to pain-related poor innervation. Extension of the left foot was reduced to MRC 4+/5. During the examination of superficial sensory function, the patient complained about hypesthesia along the left S1-dermatome. Further, the patient presented with a slightly limping gate.
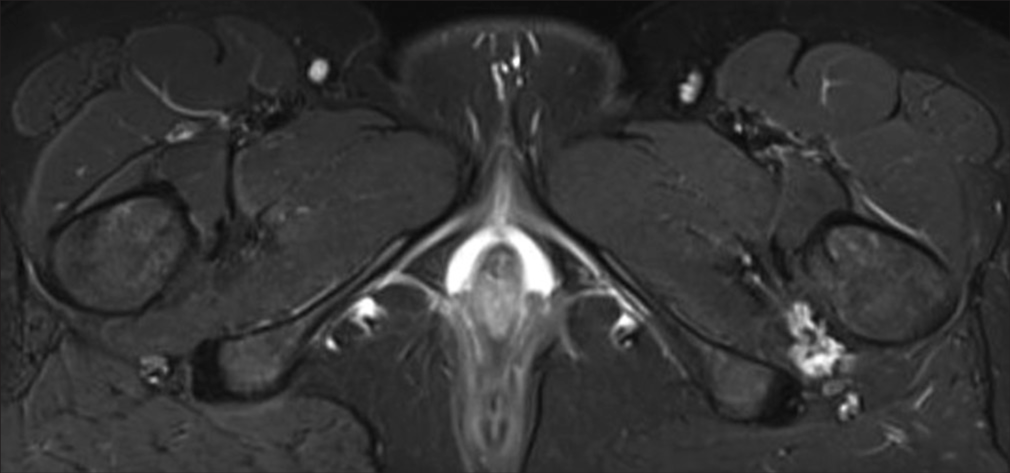
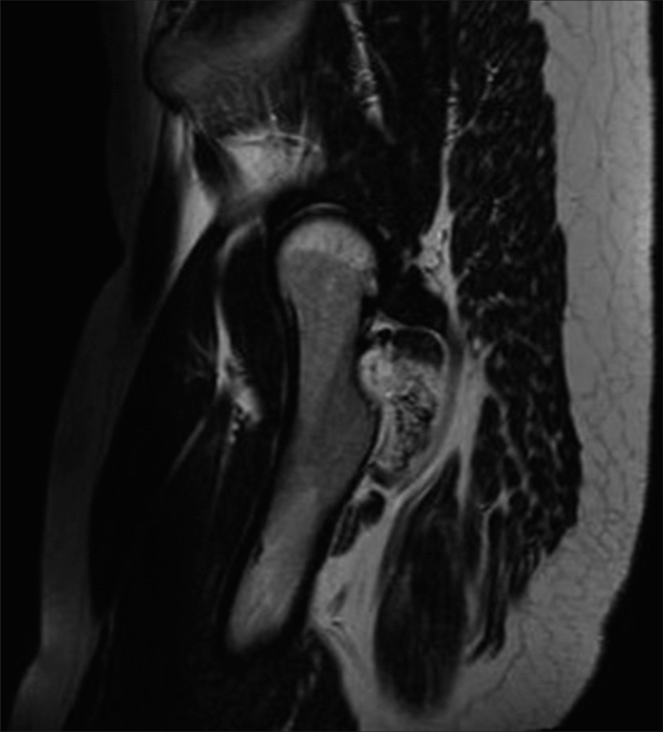
Primarily, a gynecological examination was performed, which could not reveal any reason for the symptomatology. Further, magnetic resonance imaging (MRI) of the lumbar spine was initiated but could not detect any abnormal findings [
Conservative treatment with pain medication and physiotherapy did not lead to significant improvement. Consequently, surgery was indicated.
Surgery and postoperative course
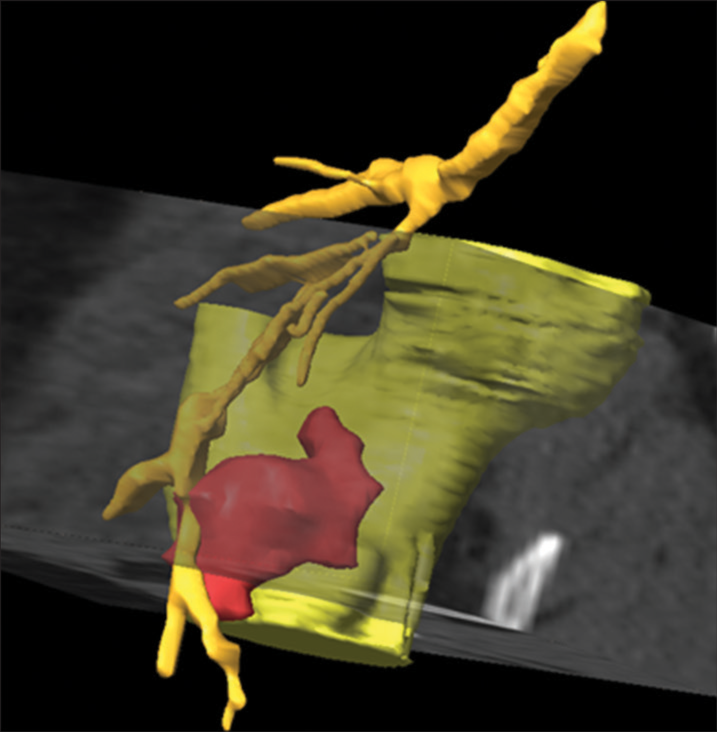
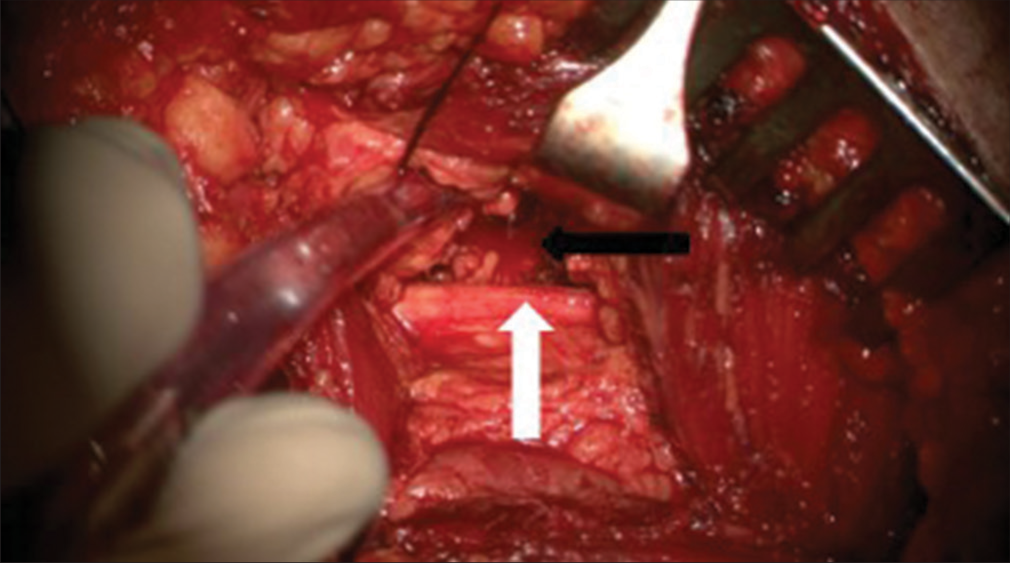
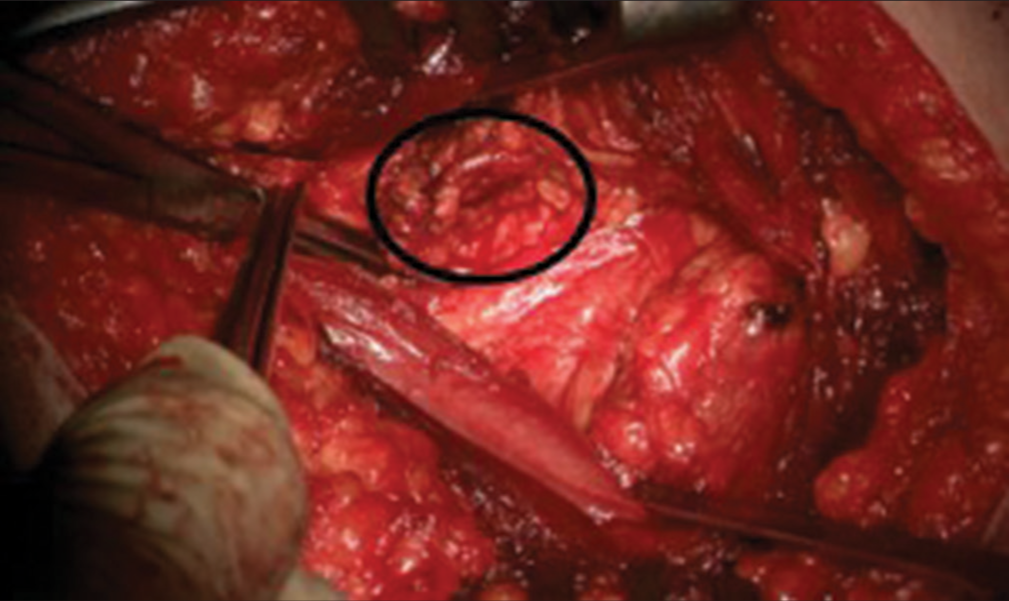
Because this uncommon entity crossed the borders of different medical fields, the operation was performed interdisciplinary and included neurosurgery, vascular surgery, and trauma surgery. Intraoperative neurophysiological monitoring (IONM) was administered, including free-running and triggered EMG (ISIS, Inomed GmbH, Emmendingen, Germany). The patient was put in a right-sided position. A Kocher–Langenbeck approach was conducted, which allows direct visualization of structures located on the posterior side of the trochanter. The sciatic nerve and pathology were visualized [
Postoperative, the patient became completely symptom-free.
Histopathological findings
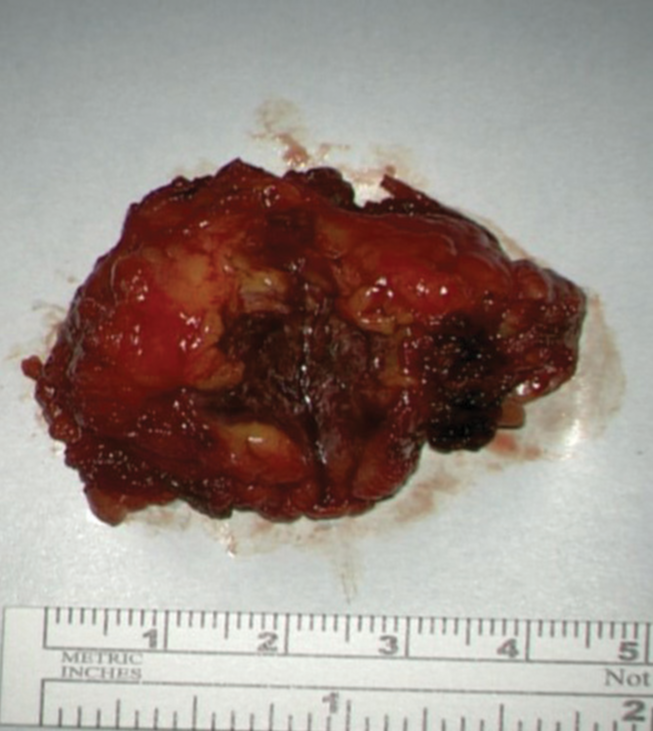
4.5 × 4.5 × 2.5 cm specimen, including slightly dilated vessels and locally calcified portions [
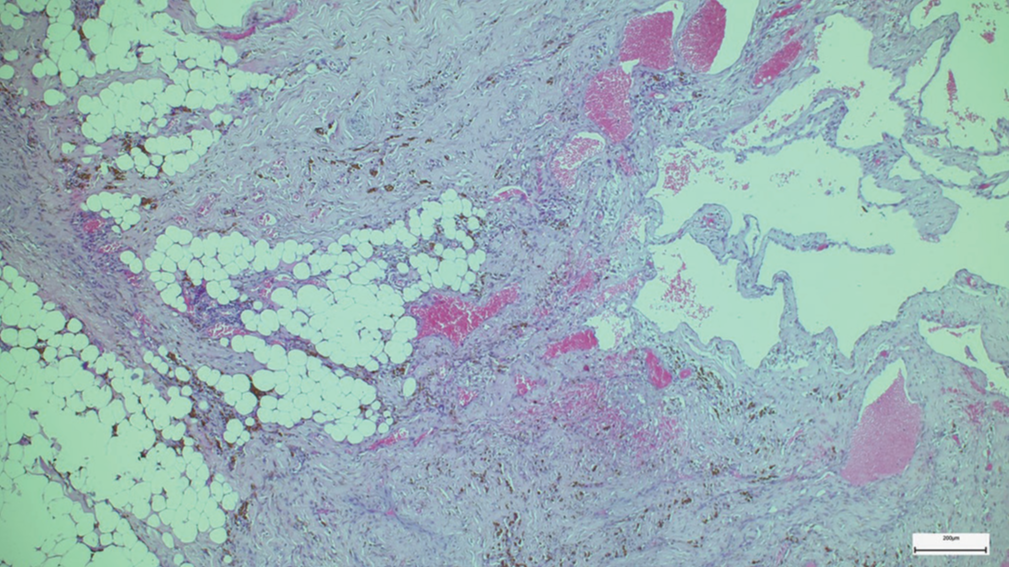
Microscopic analysis revealed an irregular non-capsulated vascular lesion infiltrating both the lipodystrophy skeletal muscle and fibro-lipomatous soft tissues. Focal intraluminal thrombi and accumulation of hemosiderophages were present throughout the lesion. No cellular atypia was observed [
DISCUSSION
Sciatica is a very frequent symptom in clinical practice and is reported to be associated with disc herniations in 87% of cases.[
Vascular malformations are categorized into low-flow and high-flow lesions.[
Clinically, venous malformations are soft, blue lesions that are compressible and can enlarge with dependent positioning or following physical exercise like in this case.[
The exact mechanism of peripheral neuropathy caused by vascular lesions is unknown. Pain is noticeably exaggerated by exercise and may be an effect of direct compression, ischemia caused by diversion of blood flow from the nerve, or venous hypertension.[
CONCLUSION
In cases where spinal imaging cannot reveal spinal morphological correlation for the treatment of refractory radicular pain, a more peripheral-located nerve compression should be considered.
Rare causes of local compression of the sciatic nerve should be considered, especially in cases of lacking spinal imaging correlation and untypical clinical presentation.
Interdisciplinary cooperation is of paramount value in treatment when the patient’s condition crosses the borders of classic medical fields.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Carqueja IM, Sousa J, Mansilha A. Vascular malformations: Classification, diagnosis and treatment. Int Angiol. 2018. 37: 127-42
2. Choudur HN, Joshi R, Munk PL. Inferior gluteal vein varicosities: A rare cause of sciatica. J Clin Rheumatol. 2009. 15: 387-8
3. Dubois J, Soulez G, Oliva VL, Berthiaume MJ, Lapierre C, Therasse E. Soft-tissue venous malformations in adult patients: Imaging and therapeutic issues. Radiographics. 2001. 21: 1519-31
4. Guedes F, Brown RS, Lourenco Torrao-Junior FJ, Siquara-de-Sousa AC, Pires Amorim RM. Nondiscogenic sciatica: What clinical examination and imaging can tell us?. World Neurosurg. 2020. 134: e1053-61
5. Hicks BL, Lam JC, Varacallo M, editors. Piriformis syndrome. StatPearls. Treasure Island, FL: StatPearls; 2023. p.
6. Hu MH, Wu KW, Jian YM, Wang CT, Wu IH, Yang SH. Vascular compression syndrome of sciatic nerve caused by gluteal varicosities. Ann Vasc Surg. 2010. 24: 1134.e1-4
7. Pacult MA, Henderson FC, Wooster MD, Varma AK. Sciatica caused by venous varix compression of the sciatic nerve. World Neurosurg. 2018. 117: 242-5
8. Porchet F, Wietlisbach V, Burnand B, Daeppen K, Villemure JG, Vader JP. Relationship between severity of lumbar disc disease and disability scores in sciatica patients. Neurosurgery. 2002. 50: 1253-9 discussion 1259-60
9. Ropper AH, Zafonte RD. Sciatica. N Engl J Med. 2015. 372: 1240-8
10. Van Gompel JJ, Griessenauer CJ, Scheithauer BW, Amrami KK, Spinner RJ. Vascular malformations, rare causes of sciatic neuropathy: A case series. Neurosurgery. 2010. 67: 1133-42 discussion 1142
11. Wirth GA, Sundine MJ. Slow-flow vascular malformations. Clin Pediatr (Phila). 2007. 46: 109-20







Cavalcante, José Ediosn da Silva
Posted May 2, 2024, 1:28 pm
very nice case and treatment -I had a patient with a venous vascular compression lateral segment spina dorsal