- Neurosciences Research Centre, Molecular and Clinical Sciences Research Institute, London, United Kingdom,
- Neurosciences Research Centre, Molecular and Clinical Sciences Research Institute, Atkinson Morley Neurosurgery Centre, St George’s, University of London, Tooting, London, United Kingdom,
- Department of General and Special Surgery, Faculty of Medicine, The Hashemite University, Zarqa, Jordan.
Correspondence Address:
Salem Al-Dwairy
Neurosciences Research Centre, Molecular and Clinical Sciences Research Institute, Atkinson Morley Neurosurgery Centre, St George’s, University of London, Tooting, London, United Kingdom,
DOI:10.25259/SNI_838_2020
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Saad Moughal1, Micaela Uberti2, Alaa Al-Mousa3, Salem Al-Dwairy3, Anan Shtaya2, Erlick Pereira2. Malignant middle cerebral artery infarction following subacute subdural hematoma: A case report and literature review. 17-Mar-2021;12:105
How to cite this URL: Saad Moughal1, Micaela Uberti2, Alaa Al-Mousa3, Salem Al-Dwairy3, Anan Shtaya2, Erlick Pereira2. Malignant middle cerebral artery infarction following subacute subdural hematoma: A case report and literature review. 17-Mar-2021;12:105. Available from: https://surgicalneurologyint.com/surgicalint-articles/10646/
Abstract
Background: Subacute subdural hematomas (ASDH) are only treated surgically when they cause mass effect significant enough to give symptoms. Rarely, sub-ASDH may cause enough pressure to result in a malignant middle cerebral artery (MCA) territory infarction. Decompressive craniectomy (DC) is the last resort to reduce intracranial pressure following malignant MCA infarction. Herein, we review the literature and describe a case of MCA/posterior cerebral artery (PCA) territories infarction following drainage of a sub-ASDH that was treated with DC with good outcome.
Case Description: We report a case of malignant right-sided MCA/PCA infarction in a 62-year-old man who presented with progressive headache following a cycling incident leading to a head injury. Initial CT head demonstrated a small right ASDH. He had no neurological deficit, headache settled on analgesia, and there was no expansion of the SDH on the repeat CT; therefore, he was managed conservatively. He was admitted 6-days later with worsening headaches and hyponatremia. Repeat CT revealed an increase in size of the hematoma and mass effect leading to a mini-craniotomy and evacuation of hematoma. He developed left-sided hemiplegia, slurred speech and hyponatremia, and CT head demonstrated a right-sided MCA/PCA infarction with significant mass effect. He underwent emergent DC and subsequent cranioplasty and ultimately recovered to mRS of 2.
Conclusion: SDH are frequent neurosurgical entities. Malignant MCA/PCA strokes following mini-craniotomies are rare but need to be considered especially during the consent process.
Keywords: Subdural hematoma, Malignant middle cerebral artery infarction, Decompressive craniectomy
INTRODUCTION
Subdural hematomas (SDH) are a well-known entity that can result from a head injury. The natural history of subdural bleeds has been described elsewhere.[
CASE REPORT
A 62-year-old male previously fit and well presented with a 1-day history of severe headache following a cycling accident that caused a head injury. There was no altered consciousness and he was neurologically intact on arrival to ED. Computer tomography (CT) of the head showed a right hemispheric acute subdural hematoma (ASDH) with no significant mass effect [
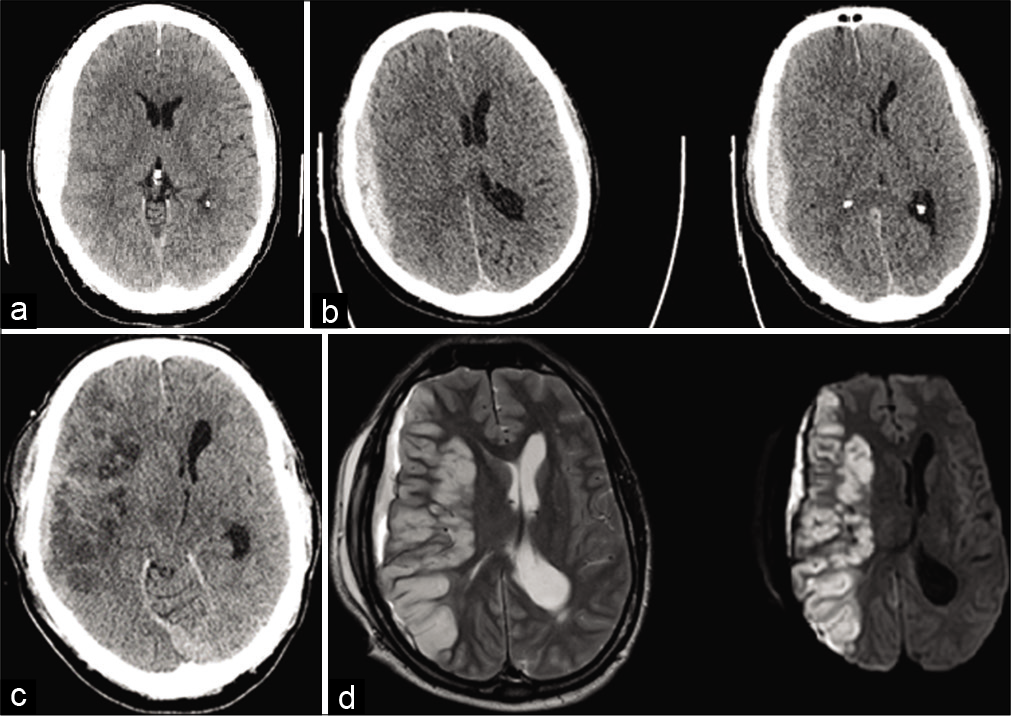
Figure 1:
Initial computed tomography (CT) demonstrated a small right acute subdural hematoma with minimal shift (a). CT performed at re-presentation demonstrated enlarged ASDH with mass effect (b). Right malignant middle cerebral artery/posterior cerebral artery territory infarction on CT (c) and MRI (T2, d).
DISCUSSION
Raised ICP can occur after an acute SDH; hence, maintenance of cerebral perfusion pressure is central to the treatment paradigm.[
In severe head injuries, vasospasm may be aggravated by hemoglobin blood products, due to SDH or subarachnoid hemorrhage, or mechanical force through endothelin-mediated hypercontractility.[
Hyponatremia is associated with an increased risk of mortality in hospitalized patients,[
DC a life-saving procedure for treatment of refractory raised ICP, in cases of large hemispheric infarction or significant head injury.[
CONCLUSION
Malignant supratentorial infarction following SDH is rarely reported. Expanding cerebral edema, hyponatremia, and reduced cerebral blood flow contribute to malignant infarction. Postoperative brain imaging in the context of progressive neurological deficit for subacute SDH is prudent to identify this rare complication. Surgical decompression was performed quickly to prevent tentorial herniation and death and produced a good functional outcome.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Adrogué HJ. Consequences of inadequate management of hyponatremia. Am J Nephrol. 2005. 25: 240-9
2. Alford PW, Dabiri BE, Goss JA, Hemphill MA, Brigham MD, Parker KK. Blast-induced phenotypic switching in cerebral vasospasm. Proc Natl Acad Sci USA. 2011. 108: 12705-10
3. Alves JL, Santiago JG, Costa G, Pinto AM. A standardized classification for subdural hematomas-I. Am J Forensic Med Pathol. 2016. 37: 174-8
4. Back L, Nagaraja V, Kapur A, Eslick GD. Role of decompressive hemicraniectomy in extensive middle cerebral artery strokes: A meta-analysis of randomised trials. Intern Med J. 2015. 45: 711-7
5. Bae DH, Choi KS, Yi HJ, Chun HJ, Ko Y, Bak KH. Cerebral infarction after traumatic brain injury: Incidence and risk factors. Korean J Neurotrauma. 2014. 10: 35-40
6. Bor-Seng-Shu E, Figueiredo EG, Amorim RL, Teixeira MJ, Valbuza JS, de Oliveira MM. Decompressive craniectomy: A meta-analysis of influences on intracranial pressure and cerebral perfusion pressure in the treatment of traumatic brain injury. J Neurosurg. 2012. 117: 589-96
7. Chen J, Li M, Chen L, Chen W, Zhang C, Feng Y. The effect of controlled decompression for severe traumatic brain injury: A randomized, controlled trial. Front Neurol. 2020. 11: 107
8. Cole CD, Gottfried ON, Liu JK, Couldwell WT. Hyponatremia in the neurosurgical patient: Diagnosis and management. Neurosurg Focus. 2004. 16: E9
9. Eberle BM, Schnüriger B, Inaba K, Gruen JP, Demetriades D, Belzberg H. Decompressive craniectomy: Surgical control of traumatic intracranial hypertension may improve outcome. Injury. 2010. 41: 894-8
10. Fujisawa H, Maxwell WL, Graham DI, Reasdale GM, Bullock R. Focal microvascular occlusion after acute subdural haematoma in the rat: A mechanism for ischaemic damage and brain swelling?. Acta Neurochir Suppl (Wien). 1994. 60: 193-6
11. Heiss WD. Malignant MCA infarction: Pathophysiology and imaging for early diagnosis and management decisions. Cerebrovasc Dis. 2016. 41: 1-7
12. Huang YH, Lee TC, Lee TH, Yang KY, Liao CC. Remote epidural hemorrhage after unilateral decompressive hemicraniectomy in brain-injured patients. J Neurotrauma. 2012. 30: 96-101
13. Kalita J, Singh RK, Misra UK. Cerebral salt wasting is the most common cause of hyponatremia in stroke. J Stroke Cerebrovasc Dis. 2017. 26: 1026-32
14. Karibe H, Hayashi T, Hirano T, Kameyama M, Nakagawa A, Tominaga T. Surgical management of traumatic acute subdural hematoma in adults: A review. Neurol Med Chir (Tokyo). 2014. 54: 887-94
15. Mirvis SE, Wolf AL, Numaguchi Y, Corradino G, Joslyn JN. Posttraumatic cerebral infarction diagnosed by CT: Prevalence, origin, and outcome. AJR Am J Roentgenol. 1990. 154: 1293-8
16. Rabinstein AA, Chung SY, Rudzinski LA, Lanzino G. Seizures after evacuation of subdural hematomas: Incidence, risk factors, and functional impact. J Neurosurg. 2010. 112: 455-60
17. Vahedi K, Hofmeijer J, Juettler E, Vicaut E, George B, Algra A. Early decompressive surgery in malignant infarction of the middle cerebral artery: A pooled analysis of three randomised controlled trials. Lancet Neurol. 2007. 6: 215-22
18. Vega RA, Valadka AB. Natural history of acute subdural hematoma. Neurosurg Clin N Am. 2017. 28: 247-55
19. Waikar SS, Mount DB, Curhan GC. Mortality after hospitalization with mild, moderate, and severe hyponatremia. Am J Med. 2009. 122: 857-65