- Department of Neurosurgery, Saitama Medical Center, Saitama Medical University, Kawagoe, Japan.
- Department of Orthopaedic Surgery, Saitama Medical Center, Saitama Medical University, Kawagoe, Japan.
Correspondence Address:
Satoshi Ogihara, Department of Orthopaedic Surgery, Saitama Medical Center, Saitama Medical University, Kawagoe, Japan.
DOI:10.25259/SNI_859_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Shinsuke Yoshida1, Shunpei Iida2, Rei Akagawa2, Soichi Oya1, Kazuo Saita2, Satoshi Ogihara2. Metastatic renal cell carcinoma of the lumbar spine with long posterior instrumented fusion and repetitive dislodgement of the set screws of the S2 alar-iliac screw. 22-Dec-2023;14:439
How to cite this URL: Shinsuke Yoshida1, Shunpei Iida2, Rei Akagawa2, Soichi Oya1, Kazuo Saita2, Satoshi Ogihara2. Metastatic renal cell carcinoma of the lumbar spine with long posterior instrumented fusion and repetitive dislodgement of the set screws of the S2 alar-iliac screw. 22-Dec-2023;14:439. Available from: https://surgicalneurologyint.com/surgicalint-articles/12682/
Abstract
Background: S2 alar-iliac screws (S2AIS) are widely used to anchor the pelvis to a lumbar fusion. Here, we report a patient who experienced repetitive dislodgement of the set screws of the S2AIS following a posterior instrumented fusion.
Case Description: A 68-year-old male presented with an L3 metastasis and L2–L3 subluxation attributed to renal cell cancer. Following an L2–L5 posterior decompression and T9-pelvic fusion utilizing bilateral S2AIS fixation, the set screws of the S2AIS repeatedly dislodged, requiring two additional operations. The final surgery required multiple anchors to the ilium and provided adequate fixation until the patient’s expiration.
Conclusion: The set screw fixing force was weaker than the fixing force of the S2AIS; multiple iliac anchors effectively salvaged this condition.
Keywords: Dislodgement, Multiple anchors, S2 alar-iliac screw, Set screw
INTRODUCTION
Fixation at the lumbosacral spine junction remains a challenge for spinal surgeons.[
CASE DESCRIPTION
History and examination
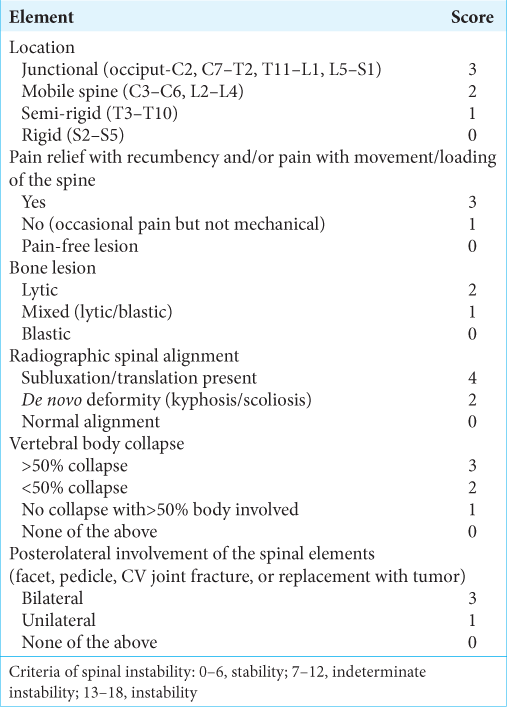
A 68-year-old male presented with 4/5 right iliopsoas and quadricep weakness accompanied by hypoesthesia of both anterolateral thighs and bladder dysfunction. The lumbar magnetic resonance imaging revealed an extradural compressive enhancing mass at the L2–3 level and invasions of the bilateral L2/3 and left L3/4 facets [
Figure 1:
(a) Sagittal gadolinium-enhanced T1-weighted magnetic resonance imaging (MRI) showing an extradural enhancing metastatic tumor at L2–3. (b) Axial MRI at L2–3 revealed severe spinal stenosis and tumor invasion of both L2/3 facet joints. (c) Axial MRI revealing tumor invasion of the left L3/4 facet.
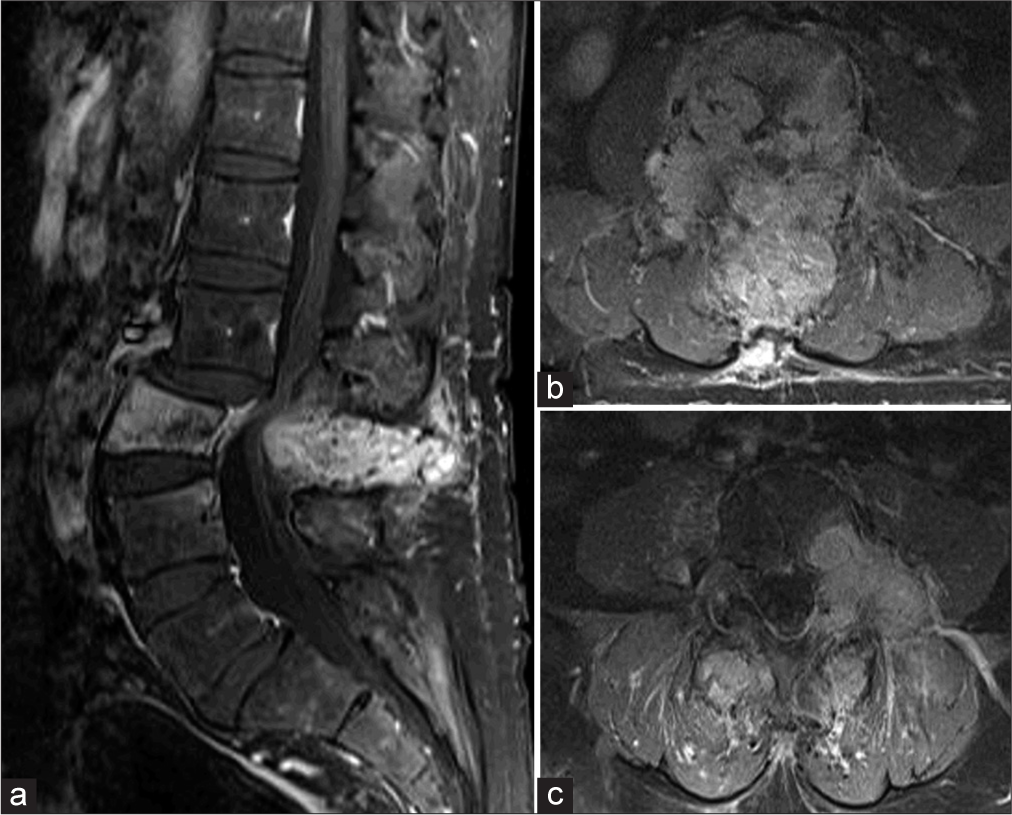
Figure 2:
(a) Axial computed tomography (CT) of L2–3 demonstrating osteolytic changes involving bilateral pedicles and part of the L2/3 facets. (b) Axial CT showing the destruction of the left L3/4 facet. (c) Sagittal L2–L3 CT image showing subluxation (arrow). (d) Sagittal CT image identifying further progression of subluxation one month later than (c) (arrow).
Surgery
An L2–5 posterior decompression was performed; the pathology was diagnostic for spinal metastasis from renal cell cancer. This decompression was followed by a posterolateral thoraco–lumbo–pelvic fusion. Pedicle screws were placed bilaterally at T10–L2 and L5–S1; bilateral transverse process hooks at T9 accompanied these. In addition, S2AISs were placed bilaterally, and a third rod was placed parallel to the center of the left and right rods to avoid rod breakage.
Postoperative course
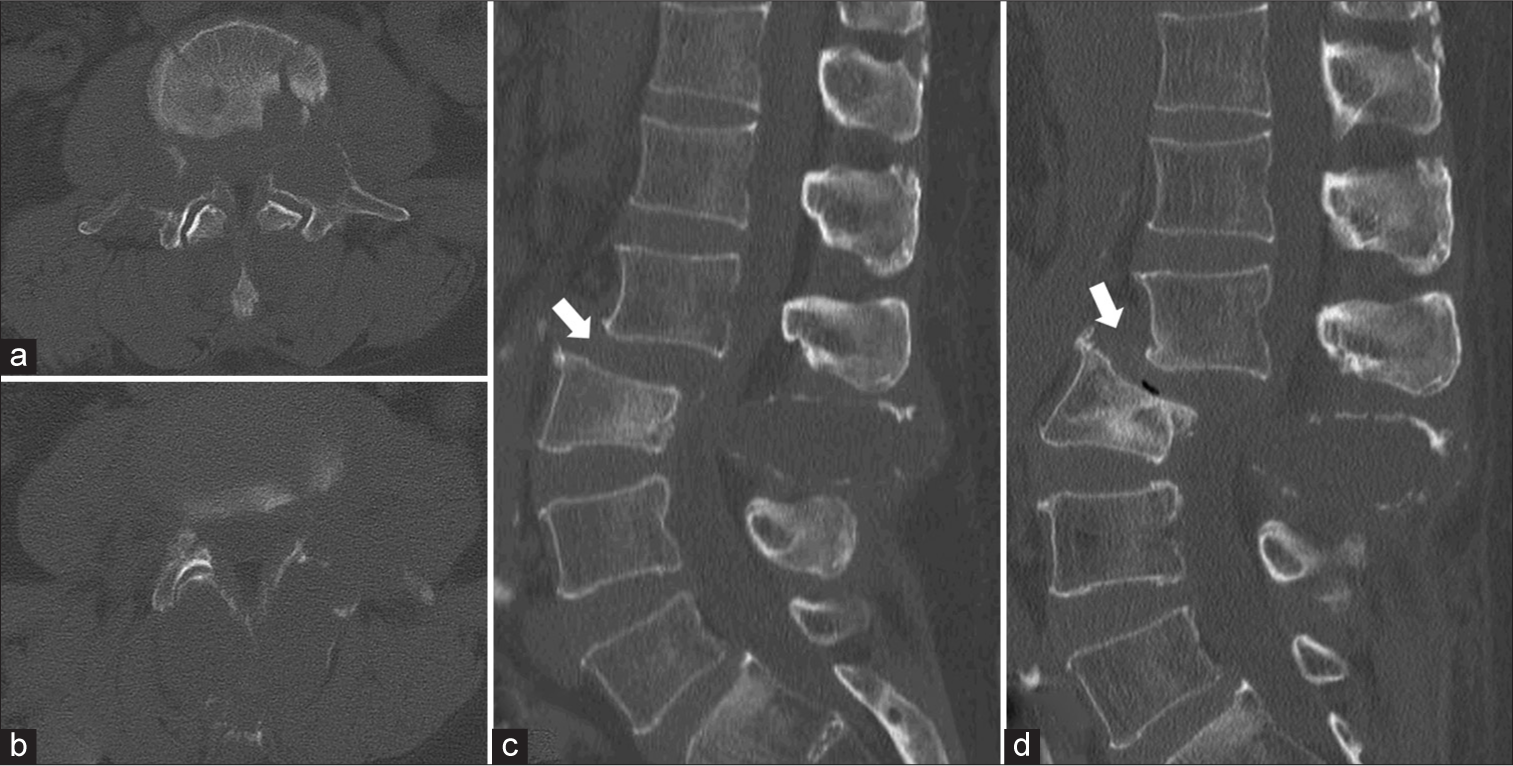
The patient’s postoperative recovery was uneventful. He received local radiotherapy at a total dose of 30 Gy for residual tumors. Although asymptomatic, radiographic assessment five months postoperatively revealed dislodgement of the bilateral set screws of the S2AIS [
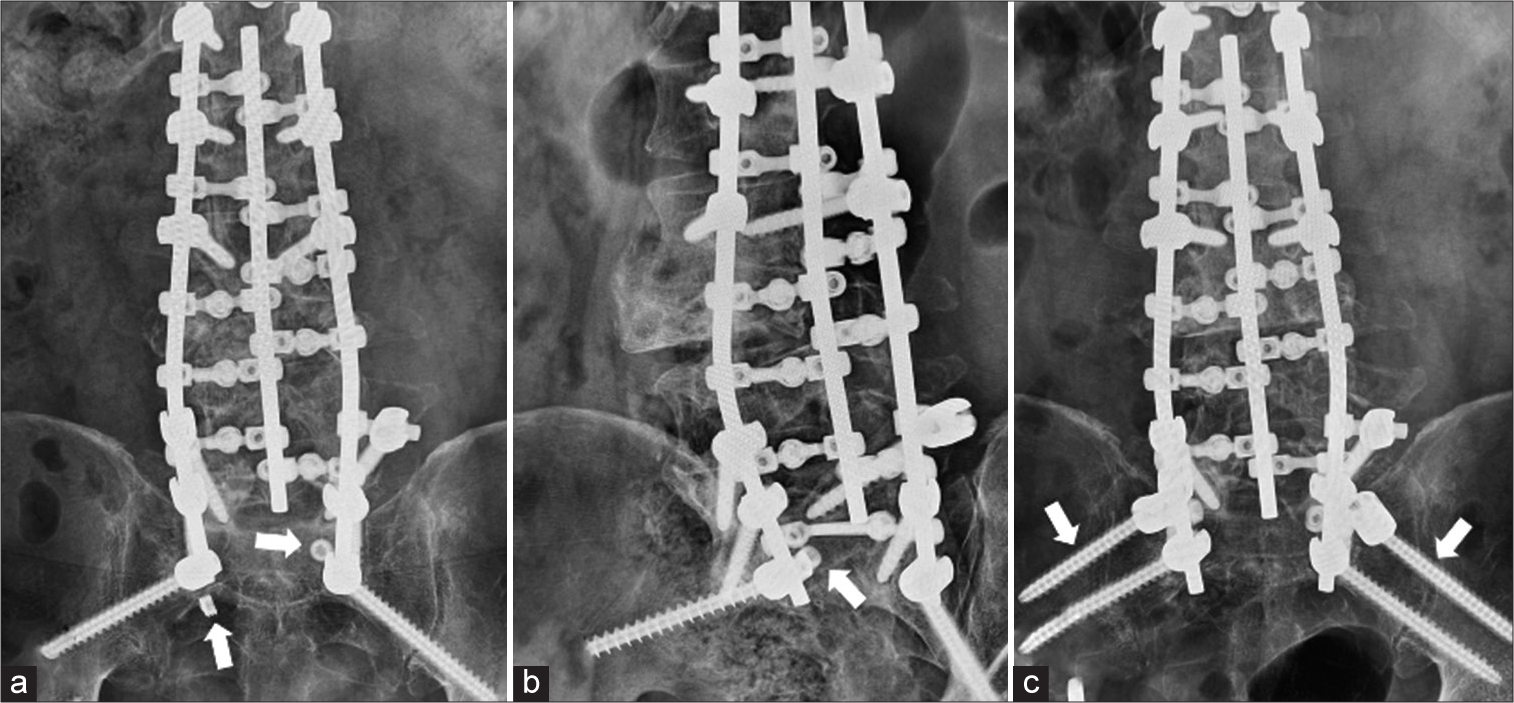
Figure 3:
(a) AP X-ray at five months post-surgery revealing dislodgement of the bilateral set screws of the S2 alar-iliac screw (S2AIS) (arrow). (b) Oblique X-ray 12 months after the second surgery showing the repeated dislodgement of the right set screw of the S2AIS (arrow). (c) AP X-ray at the final follow-up showed the stability of the fusion with the S2AIS and iliac screws (arrow).
DISCUSSION
Efficacy and mechanical failure of S2AIS for thoraciclumbar-sacral fusions
The mechanical demand at and around the lumbosacral junction following long-segment thoracolumbar–sacral fusion results in a 12–57% incidence of mechanical failure.[
Drawbacks of using S2AISs to stabilize thoracic-lumbarsacral fusions
The S2AIS achieves highly rigid fixation by crossing three cortical surfaces through the sacroiliac joint;[
CONCLUSION
The S2AIS has a strong fixing force; however, the set screw fixing force may be relatively weak. Multiple iliac anchors should be considered for extensive thoraco–lumbo–sacral fusions to prevent construct failure at the sacral level.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript, and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Chang TL, Sponseller PD, Kebaish KM, Fishman EK. Low profile pelvic fixation: Anatomic parameters for sacral alar-iliac fixation versus traditional iliac fixation. Spine (Phila Pa 1976). 2009. 34: 436-40
2. Cho W, Mason JR, Smith JS, Shimer AL, Wilson AS, Shaffrey CI. Failure of lumbopelvic fixation after long construct fusions in patients with adult spinal deformity: Clinical and radiographic risk factors: Clinical article. J Neurosurg Spine. 2013. 19: 445-53
3. Elder BD, Ishida W, Lo SF, Holmes C, Goodwin CR, Kosztowski TA. Use of S2-alar-iliac screws associated with less complications than iliac screws in adult lumbosacropelvic fixation. Spine (Phila Pa 1976). 2017. 42: E142-9
4. Fisher CG, DiPaola CP, Ryken TC, Bilsky MH, Shaffrey CI, Berven SH. A novel classification system for spinal instability in neoplastic disease: An evidence-based approach and expert consensus from the Spine Oncology Study Group. Spine (Phila Pa 1976). 2010. 35: E1221-9
5. Guler UO, Cetin E, Yaman O, Pellise F, Casademut AV, Sabat MD. Sacropelvic fixation in adult spinal deformity (ASD); a very high rate of mechanical failure. Eur Spine J. 2015. 24: 1085-91
6. Hyun SJ, Jung JM, Kim KJ, Jahng TA. Durability and failure types of S2-alar-iliac screws: An analysis of 312 consecutive screws. Oper Neurosurg (Hagerstown). 2020. 20: 91-7
7. Kebaish KM. Sacropelvic fixation: Techniques and complications. Spine (Phila Pa 1976). 2010. 35: 2245-51
8. Kim YJ, Bridwell KH, Lenke LG, Rhim S, Cheh G. Pseudarthrosis in long adult spinal deformity instrumentation and fusion to the sacrum: Prevalence and risk factor analysis of 144 cases. Spine (Phila Pa 1976). 2006. 31: 2329-36
9. Park SJ, Park JS, Nam Y, Yum TH, Choi YT, Lee CS. Failure types and related factors of spinopelvic fixation after long construct fusion for adult spinal deformity. Neurosurgery. 2021. 88: 603-11
10. Tokuhashi Y, Matsuzaki H, Oda H, Oshima M, Ryu J. A revised scoring system for preoperative evaluation of metastatic spine tumor prognosis. Spine (Phila Pa 1976). 2005. 30: 2186-91