- Department of Neurosurgery, University of Tennessee Health Science Center, Memphis, Tennessee, United States
Correspondence Address:
Kara A. Parikh, Department of Neurosurgery, University of Tennessee Health Science Center, Memphis, Tennessee, United States.
DOI:10.25259/SNI_1102_2024
Copyright: © 2025 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Kara A. Parikh, Mustafa Motiwala, Emal Lesha, John E. Dugan, Kaan Yagmurlu, Adam S. Arthur, Nickalus R. Khan. Microsurgical resection and endovascular embolization of a left inferior frontal and Sylvian Spetzler-Martin grade 3 arteriovenous malformation. 04-Apr-2025;16:120
How to cite this URL: Kara A. Parikh, Mustafa Motiwala, Emal Lesha, John E. Dugan, Kaan Yagmurlu, Adam S. Arthur, Nickalus R. Khan. Microsurgical resection and endovascular embolization of a left inferior frontal and Sylvian Spetzler-Martin grade 3 arteriovenous malformation. 04-Apr-2025;16:120. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=13486
Abstract
Background: Arteriovenous malformations (AVMs) carry an estimated 2–4% annual risk of rupture, with an estimated 70–75% lifetime risk. They are typically discovered during young adulthood, occurring in approximately 5/10,000 individuals. Modalities of treatment involve endovascular treatment, Gamma Knife, microsurgical resection under general anesthesia, awake craniotomy, or a combination of these modalities.
Case Description: We present the case of a 33-year-old male presenting with headaches who was found to have an incidental left inferior frontal Spetzler-Martin Grade 3 AVM adjacent to Broca’s area. Given the large size of the AVM, the patient’s young age, and the lifetime risk of rupture, the patient underwent a planned 2-stage preoperative embolization and microsurgical resection under general anesthesia with intraoperative monitoring. Complete resection of the AVM was observed on postoperative digital subtraction angiography. The patient was discharged home on postoperative day 4. The patient’s transient postoperative mixed aphasia had fully resolved by the time of discharge. A review of the benefits of preoperative embolization and the technical considerations of resection of a large AVM in eloquent regions of the brain are included. The patient consented to the procedure and the publication of his images. The Institutional Review Board approval was deemed unnecessary due to the retrospective, case-report nature of this work.
Conclusion: Large AVMs in the eloquent brain can present a challenge to the surgeon. Staged, multi-modality intervention involving staged preoperative embolization and functional MRI preoperative planning can be an effective treatment strategy for strategic, safe microsurgical resection under general anesthesia for AVMs in the eloquent brain.
Keywords: Arteriovenous malformation, Broca’s area, Embolization, Microsurgical, Sylvian fissure
Video 1
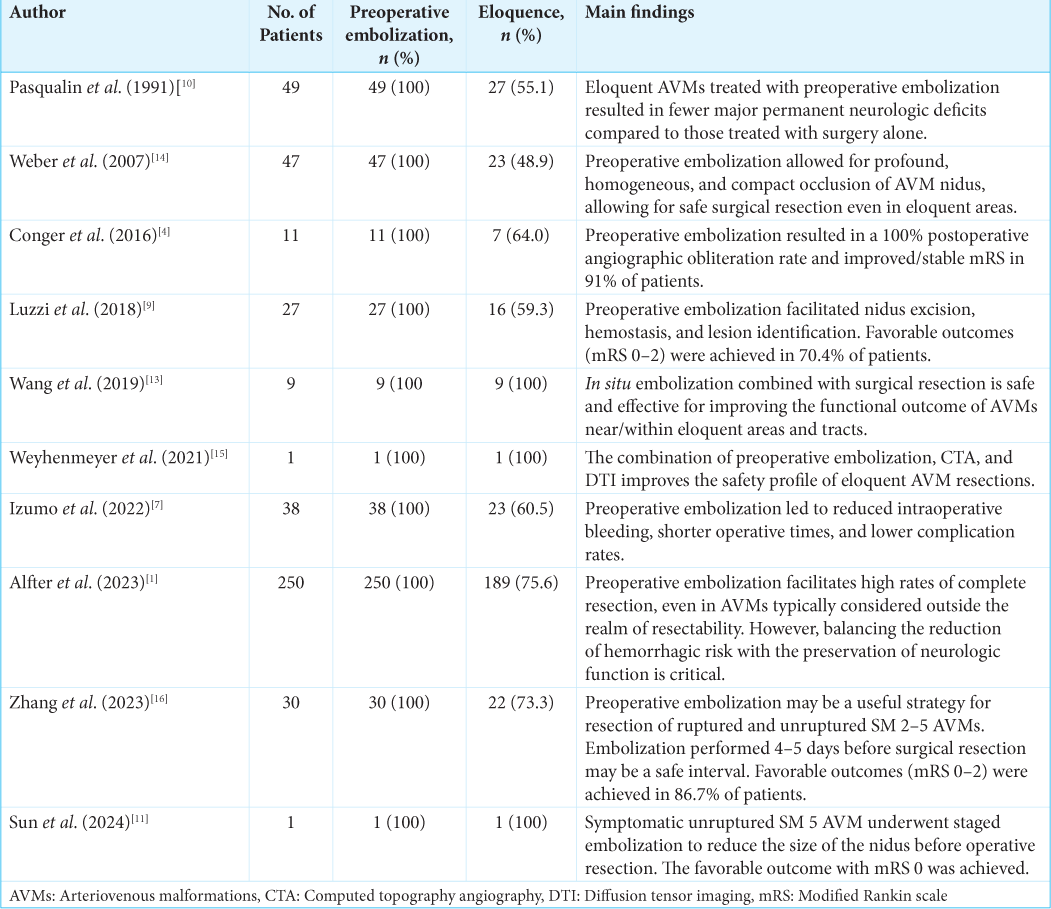
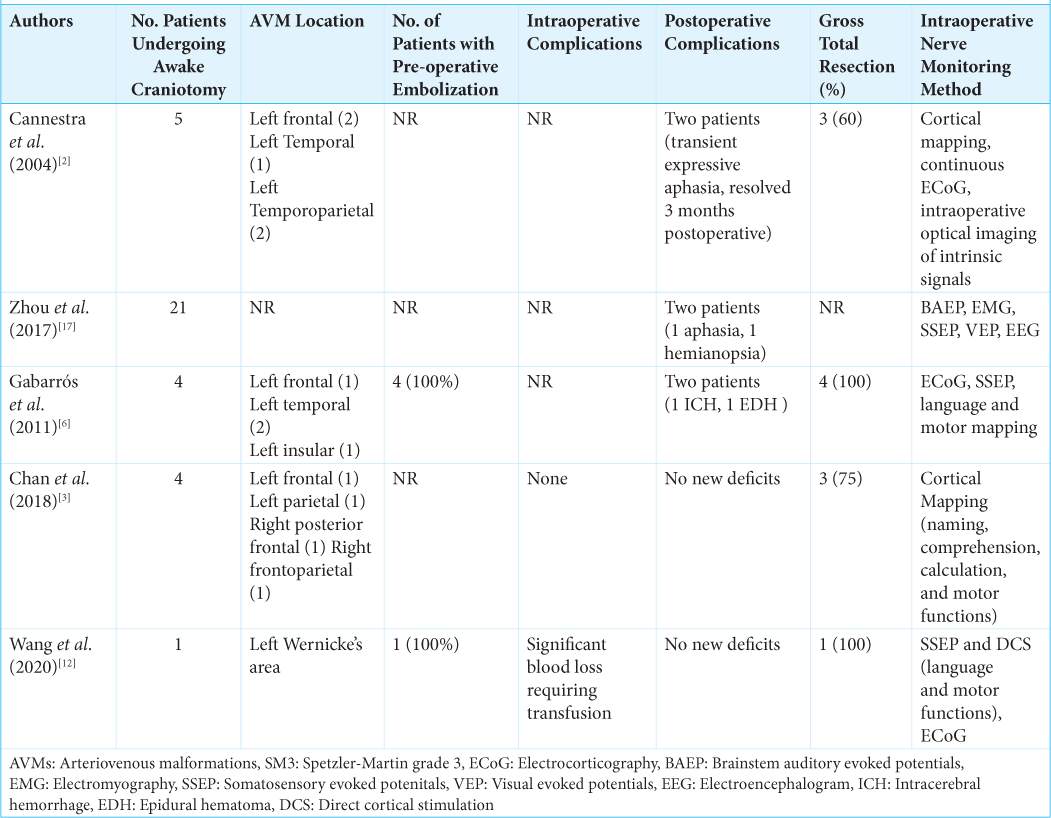
Annotations[Tables 1 and 2][1-17]
0:12 Clinical Presentation
0:28 Preoperative Imaging
1:50 Rationale for the Procedure
2:06 Risks of Procedure and Potential Benefit
2:16 Alternatives for Treatment
2:53 Description of Setup
3:50 Post-embolization Angiography
4:06 Splitting Sylvian Fissure
4:56 Indocyanine Green Angiography
5:05 Resection of AVM Nidus
6:00 Anatomical Schematic of Surgical Site
6:54 Disease Background
7:25 Technical Considerations
7:50 Literature Review
8:20 Clinical and Imaging Outcome
8:36 Postoperative Angiography
Ethical approval
The Institutional Review Board has waived the ethical approval for this study.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript, and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Alfter M, Albiña-Palmarola P, Cimpoca A, Díaz-Peregrino R, Jans P, Ganslandt O. Multi-stage treatment for spetzlermartin grades III, IV, and V arteriovenous malformations: Preoperative embolization and microsurgical resection in a consecutive series of 250 patients. J Clin Med. 2023. 12: 5990
2. Cannestra AF, Pouratian N, Forage J, Bookheimer SY, Martin NA, Toga AW. Functional magnetic resonance imaging and optical imaging for dominant-hemisphere perisylvian arteriovenous malformations. Neurosurgery. 2004. 55: 804-12 discussion 812-4
3. Chan DY, Chan DT, Zhu CX, Kan PK, Ng AY, Hsieh YP. Awake craniotomy for excision of arteriovenous malformations? A qualitative comparison study with stereotactic radiosurgery. J Clin Neurosci. 2018. 51: 52-6
4. Conger JR, Ding D, Raper DM, Starke RM, Durst CR, Liu KC. Preoperative embolization of cerebral arteriovenous malformations with silk suture and particles: Technical considerations and outcomes. J Cerebrovasc Endovasc Neurosurg. 2016. 18: 90-9
5. De Leacy R, Ansari SA, Schirmer CM, Cooke DL, Prestigiacomo CJ, Bulsara KR. Endovascular treatment in the multimodality management of brain arteriovenous malformations: Report of the society of neurointerventional surgery standards and guidelines committee. J NeuroInterv Surg. 2022. 14: 1118-24
6. Gabarrós A, Young WL, McDermott MW, Lawton MT. Language and motor mapping during resection of brain arteriovenous malformations: Indications, feasibility, and utility. Neurosurgery. 2011. 68: 744-52
7. Izumo T, Okamura K, Takahira R, Matsunaga Y, Sadakata E, Maeda H. Impact of pre-operative embolization with onyx for brain arteriovenous malformation surgery. Front Neurol. 2022. 13: 875260
8. Kondziolka D, McLaughlin MR, Kestle JR. Simple risk predictions for arteriovenous malformation hemorrhage. Neurosurgery. 1995. 37: 851-5
9. Luzzi S, Del Maestro M, Bongetta D, Zoia C, Giordano AV, Trovarelli D. Onyx embolization before the surgical treatment of grade iii spetzler-martin brain arteriovenous malformations: Single-center experience and technical nuances. World Neurosurg. 2018. 116: e340-53
10. Pasqualin A, Scienza R, Cioffi F, Barone G, Benati A, Beltramello A. Treatment of cerebral arteriovenous malformations with a combination of preoperative embolization and surgery. Neurosurgery. 1991. 29: 358-68
11. Sun H, Richard SA, Lan Z. Giant brain arteriovenous malformation managed by staged embolizations and surgical resection with satisfactory outcome. World Neurosurg. 2024. 181: 3-4
12. Wang AT, Pillai P, Guran E, Carter H, Minasian T, Lenart J. Anesthetic management of awake craniotomy for resection of the language and motor cortex vascular malformations. World Neurosurg. 2020. 143: e136-48
13. Wang M, Qiu H, Cao Y, Wang S, Zhao J. One-staged in situ embolization combined with surgical resection for eloquence protection of AVM: Technical note. Neurosurg Rev. 2019. 42: 783-90
14. Weber W, Kis B, Siekmann R, Jans P, Laumer R, Kühne D. Preoperative embolization of intracranial arteriovenous malformations with onyx. Neurosurgery. 2007. 61: 244-52 discussion 252-4
15. Weyhenmeyer J, Ordaz JD, Cohen Gadol A, Shah M. Preoperative embolization with fused CT angiography and tractography facilitates safe resection of a spetzler-martin grade IV arteriovenous malformation. Cureus. 2021. 13: e20657
16. Zhang B, Qi J, Chen P, Sun B, Ling Y, Wu Q. Deliberately staged combined endovascular embolization and subsequent microsurgery resection for the treatment of cerebral arteriovenous malformations. World Neurosurg. 2023. 178: e254-64
17. Zhou Q, Li M, Yi L, He B, Li X, Jiang Y. Intraoperative neuromonitoring during brain arteriovenous malformation microsurgeries and postoperative dysfunction: A retrospective follow-up study. Medicine (Baltimore). 2017. 96: e8054