- Department of Neurosurgery, South Miyagi Medical Center, Shibata-gun, Miyagi, Japan
- Division of Neurosurgery, Tohoku Medical and Pharmaceutical University, Sendai, Miyagi, Japan
- Department of Neurology, South Miyagi Medical Center, Shibata-gun, Miyagi, Japan
- Department of Neurosurgery, Tohoku University Graduate School of Medicine, Sendai, Miyagi, Japan.
Correspondence Address:
Satoru Ohtomo, Department of Neurosurgery, South Miyagi Medical Center, Shibata-gun, Miyagi, Japan.
DOI:10.25259/SNI_56_2024
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Youhei Takeuchi1, Hiroaki Arai1, Toshiki Endo2, Satoshi Shibuya3, Satoru Ohtomo1, Hidenori Endo4. Microvascular decompression is effective for oculomotor nerve palsy caused by posterior cerebral artery compression: A case report. 24-May-2024;15:174
How to cite this URL: Youhei Takeuchi1, Hiroaki Arai1, Toshiki Endo2, Satoshi Shibuya3, Satoru Ohtomo1, Hidenori Endo4. Microvascular decompression is effective for oculomotor nerve palsy caused by posterior cerebral artery compression: A case report. 24-May-2024;15:174. Available from: https://surgicalneurologyint.com/surgicalint-articles/12904/
Abstract
Background: Oculomotor nerve palsy is often associated with diabetes mellitus or caused by compression by a cerebral aneurysm. Here, we report a rare case of oculomotor nerve palsy caused by compression by the posterior cerebral artery (PCA).
Case Description: A 66-year-old woman suddenly developed diplopia and right blepharoptosis. Her symptoms suggested incomplete right oculomotor nerve palsy. Magnetic resonance imaging showed that a sharp curve in the right PCA had compressed the right oculomotor nerve. Microvascular decompression surgery was performed. Intraoperative findings showed that the P2 portion of the PCA had caused an indentation in the oculomotor nerve in the prepontine cistern. The transposition of the PCA with a prosthesis released the pressure. After the operation, her right blepharoptosis gradually improved. She had fully recovered by 48 days after the operation.
Conclusion: Neurovascular compression (NVC) is recognized as the cause of hemifacial spasms, trigeminal neuralgia, and glossopharyngeal neuralgia. This case report demonstrated that NVC can also cause oculomotor nerve palsy. A high index of clinical suspicion can detect vascular compression of the oculomotor nerve. Prompt diagnosis and appropriate surgical management can achieve clinical improvement.
Keywords: Microvascular decompression, Oculomotor nerve palsy, Posterior cerebral artery
INTRODUCTION
Compression caused by cerebral aneurysms and diabetes mellitus are well-known causes of oculomotor nerve palsy.[
CASE REPORT
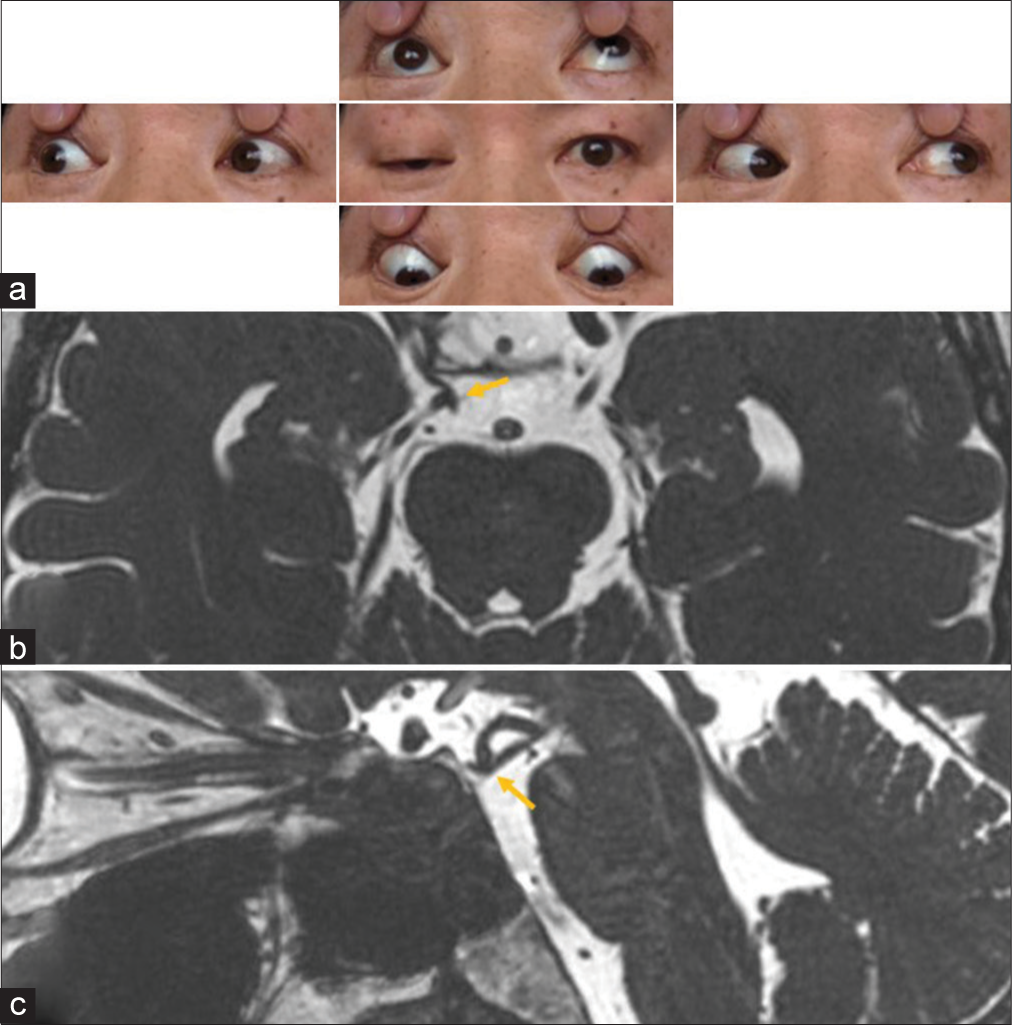
A 66-year-old woman suddenly developed diplopia and right blepharoptosis. Neurological examination revealed impaired supraduction of the right eyeball, slightly mydriatic pupil with sluggish indirect light reflex, and right blepharoptosis, indicating incomplete right oculomotor palsy [
Figure 1:
Preoperative findings. (a) Photographs of the patient’s eyes showing right blepharoptosis and moderate supraduction. Adduction and infraduction are not clearly observed. Her right pupil is not dilated. (b and c) Preoperative axial (b) and sagittal (c) heavily T2-weighted magnetic resonance images demonstrating the right posterior cerebral artery bent caudally and apparently conflicting with the right oculomotor nerve.
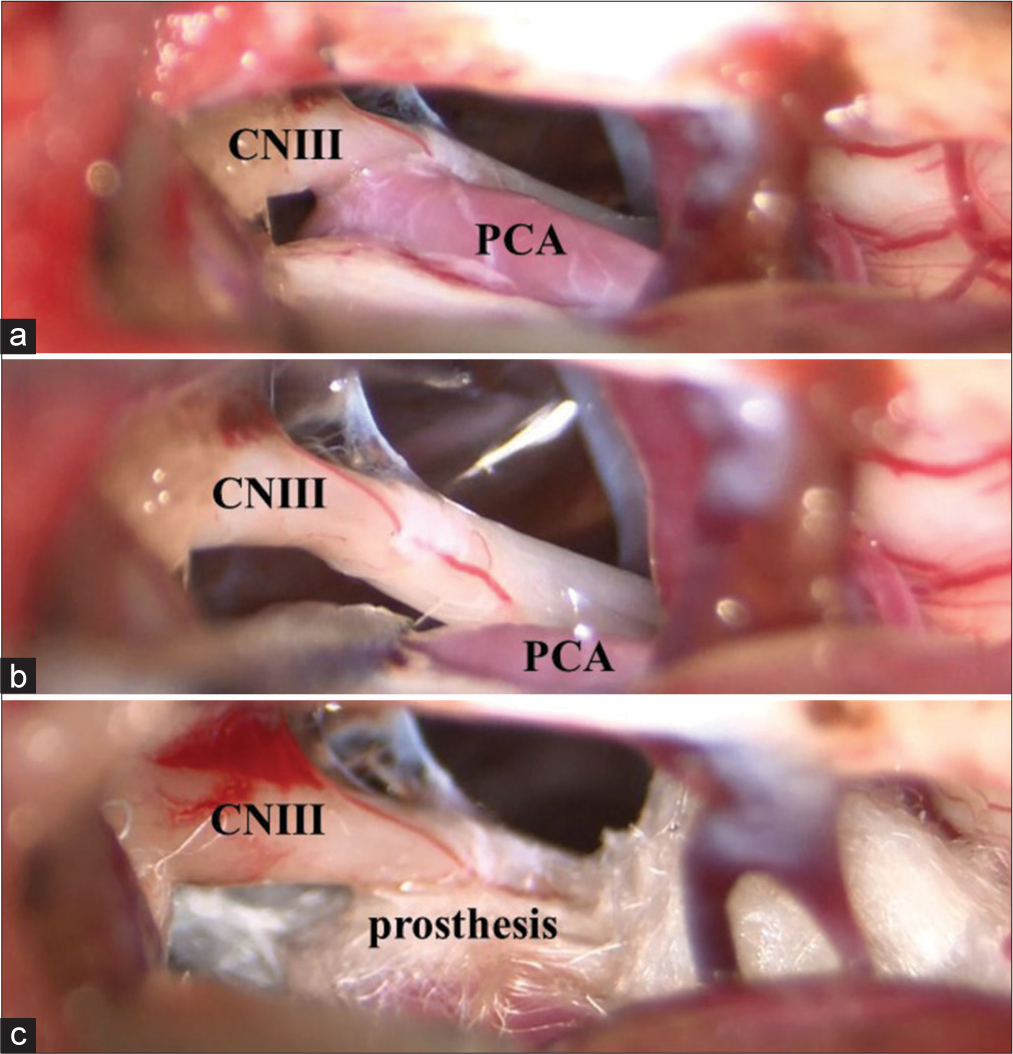
The patient underwent MVD of the right oculomotor nerve through the subtemporal approach. Surgical findings indicated a caudal bend in the P2 segment of the right PCA, which had compressed the oculomotor nerve, resulting in an indentation in the nerve [
DISCUSSION
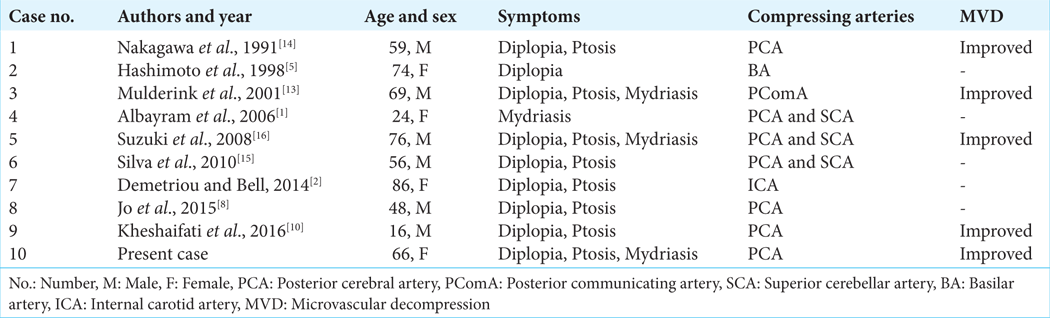
NVC syndrome presenting with oculomotor nerve palsy is a rare condition that has not yet gained widespread recognition. Therefore, in previous patients with oculomotor nerve palsy without a definite cause, the true cause may have been overlooked. Of the past 10 cases of oculomotor nerve palsy thought to be caused by NVC, improvement in symptoms was confirmed in all five cases in which MVD was performed [
NVC syndrome can be classified into hyperactive dysfunction and hypoactive dysfunction.[
Interestingly, few case reports on hyperactive dysfunction of the oculomotor nerve and ocular neuromyotonia caused by vascular compression have been published.[
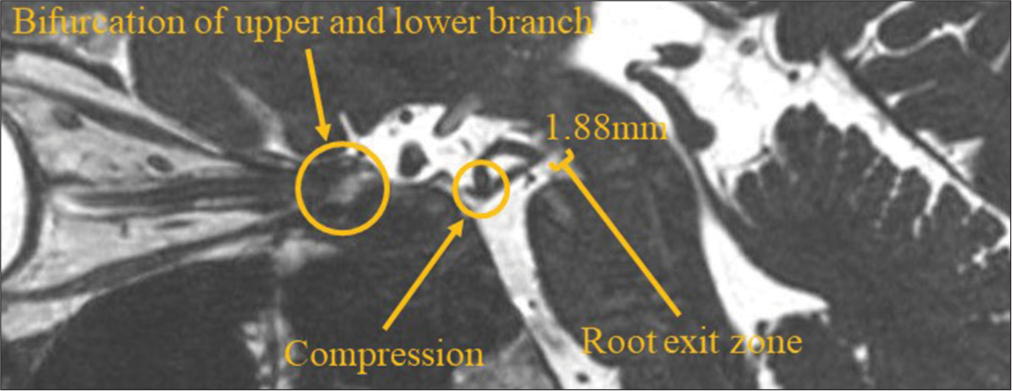
We treated a patient with oculomotor nerve palsy caused by compression by the PCA. MVD surgery led to the complete remission of symptoms. Our patient had incomplete oculomotor nerve palsy, manifesting as moderately impaired supraduction but intact adduction and infraduction. The clinical course of this patient not only shows that NVC can cause oculomotor nerve palsy but also provides anatomical suggestions about the oculomotor nerve fibers. The oculomotor nerve divides into the upper and lower branches in the fissure segment.[
CONCLUSION
Vascular compression of the peripheral oculomotor nerve can cause oculomotor nerve palsy. A high index of clinical suspicion can detect vascular compression of the oculomotor nerve. Prompt diagnosis and appropriate surgical management can achieve clinical improvement.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Albayram S, Ozer H, Sarici A, Murphy K, Miller N. Unilateral mydriasis without ophthalmoplegia--a sign of neurovascular compression? Case report. Neurosurgery. 2006. 58: E582-3
2. Demetriou GA, Bell D. Isolated third cranial nerve palsy from non-aneurysmal internal carotid artery compression. QJM. 2014. 107: 855-6
3. Frohman EM, Zee DS. Ocular neuromyotonia: Clinical features, physiological mechanisms, and response to therapy. Ann Neurol. 1995. 37: 620-6
4. Good EF. Ptosis as the sole manifestation of compression of the oculomotor nerve by an aneurysm of the posterior communicating artery. J Clin Neuroophthalmol. 1990. 10: 59-61
5. Hashimoto M, Ohtsuka K, Akiba H, Harada K. Vascular compression of the oculomotor nerve disclosed by thin-slice magnetic resonance imaging. Am J Ophthalmol. 1998. 125: 881-2
6. Iaconetta G, de Notaris M, Cavallo LM, Benet A, Ensenat J, Samii M. The oculomotor nerve: Microanatomical and endoscopic study. Neurosurgery. 2010. 66: 593-601
7. Jannetta PJ. Observations on the etiology of trigeminal neuralgia, hemifacial spasm, acoustic nerve dysfunction and glossopharyngeal neuralgia. Definitive microsurgical treatment and results in 117 patients. Neurochirurgia (Stuttg). 1997. 20: 145-54
8. Jo YS, Kim SK, Kim DH, Kim JH, Na SJ. Complete oculomotor nerve palsy caused by direct compression of the posterior cerebral artery. J Stroke Cerebrovasc Dis. 2015. 24: e189-90
9. Kasner SE, Liu GT, Galetta SL. Neuro-ophthalmologic aspects of aneurysms. Neuroimaging Clin N Am. 1997. 7: 679-92
10. Kheshaifati H, Al-Otaibi F, Alhejji M. Microvascular decompression for oculomotor nerve palsy: A case report and literature review. World Neurosurg. 2016. 88: 695.e1-3
11. Kumar MP, Vivekanand U, Umakanth S, Yashodhara BM. A study of etiology and prognosis of oculomotor nerve paralysis. Edorium J Neurol. 2014. 1: 1-8
12. Lang J, editors. Clinical anatomy of the posterior cranial fossa and its foramina. New York: Thieme Medical; 1991. p.
13. Mulderink TA, Bendok BR, Yapor WY, Batjer HH. Third nerve paresis caused by vascular compression by the posterior communicating artery. J Stroke Cerebrovasc Dis. 2001. 10: 139-41
14. Nakagawa H, Nakajima S, Nakajima Y, Furuta Y, Nishi O, Nishi K. Bilateral oculomotor nerve palsies due to posterior cerebral arterial compression relieved by microvascular decompression--case report. Neurol Med Chir (Tokyo). 1991. 31: 45-8
15. Silva EB, Ramina R, Meneses MS, Kowacs PA, Silva EB. Bilateral oculomotor nerve palsies due to vascular conflict. Arq Neuropsiquiatr. 2010. 68: 819-21
16. Suzuki K, Muroi A, Kujiraoka Y, Takano S, Matsumura A. Oculomotor palsy treated by microvascular decompression. Surg Neurol. 2008. 70: 210-2
17. Tilikete C, Vial C, Niederlaender M, Bonnier PL, Vighetto A. Idiopathic ocular neuromyotonia: A neurovascular compression syndrome?. J Neurol Neurosurg Psychiatry. 2000. 69: 642-4
18. Tsuji M, Shima A, Suzuki F, Tsuji M, Shima A, Suzuki F. Ocular neuromyotonia treated by microvascular decompression: Usefulness of preoperative 3D imaging: Case report. J Neurosurg. 2012. 117: 1166-9