- Department Neurological Surgery, Juntendo University Urayasu Hospital, Urayasu, Chiba, Japan.
Correspondence Address:
Satoshi Tsutsumi, Department Neurological Surgery, Juntendo University Urayasu Hospital, Urayasu, Chiba, Japan.
DOI:10.25259/SNI_1103_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Aito Watanabe, Satoshi Tsutsumi, Senshu Nonaka, Hisato Ishii. Microvascular proliferation in the clots: The key finding of acute subdural hematoma transforming into chronic subdural hematoma?. 08-Dec-2021;12:601
How to cite this URL: Aito Watanabe, Satoshi Tsutsumi, Senshu Nonaka, Hisato Ishii. Microvascular proliferation in the clots: The key finding of acute subdural hematoma transforming into chronic subdural hematoma?. 08-Dec-2021;12:601. Available from: https://surgicalneurologyint.com/surgicalint-articles/11272/
Abstract
Background: Despite extensive investigations, the exact etiology of chronic subdural hematoma (CSDH) remains elusive. Organized CSDHs are a distinct but less-understood type of CSDH.
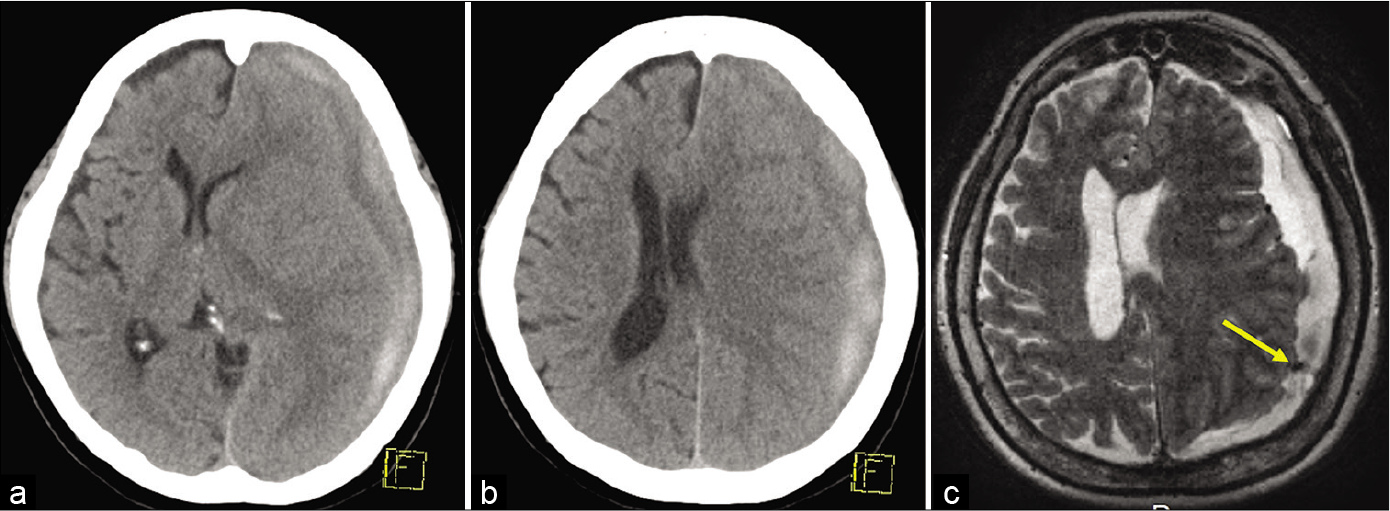
Case Description: A 50-year-old hypertensive woman experienced headache without any previous head injury. At presentation, the patient showed no focal neurological deficits. Cranial computed tomography (CT) revealed a slightly compressive subdural hematoma that spontaneously regressed and no intracranial vascular lesions. Cerebral magnetic resonance imaging identified a non-enhancing nodular lesion in the subdural hematoma. After the patient presented disorientation and aphasia on post hospitalization day 14, CT showed a considerable enlargement of the subdural hematoma. Partial removal of the bi-layered hematoma was performed through a parietal craniotomy. Histological examination revealed microvascular proliferation in both the outer membrane and the nodular lesion. On postoperative day 35, CT demonstrated a remarkable resolution of the residual hematoma.
Conclusion: Development of microvascular proliferation in the clots of an acute subdural hematoma may lead to its rapid enlargement as an organized CSDH. Organized CSDH can be managed by partial removal of the outer membrane and hematoma through a craniotomy.
Keywords: Acute subdural hematoma, Chronic subdural hematoma, Craniotomy, Microvascular proliferation, Subdural clots
INTRODUCTION
Chronic subdural hematoma (CSDH) is one of the most common neurosurgical disorders. Typically, it is managed by burr hole drainage or an evacuation through a craniotomy. Despite extensive investigations, however, its exact etiology and optimal treatment strategy remain elusive.[
In contrast with trauma-associated ASDH, spontaneous or non-traumatic ASDH is thought to occur infrequently in association with a variety of pathological processes.[
CASE PRESENTATION
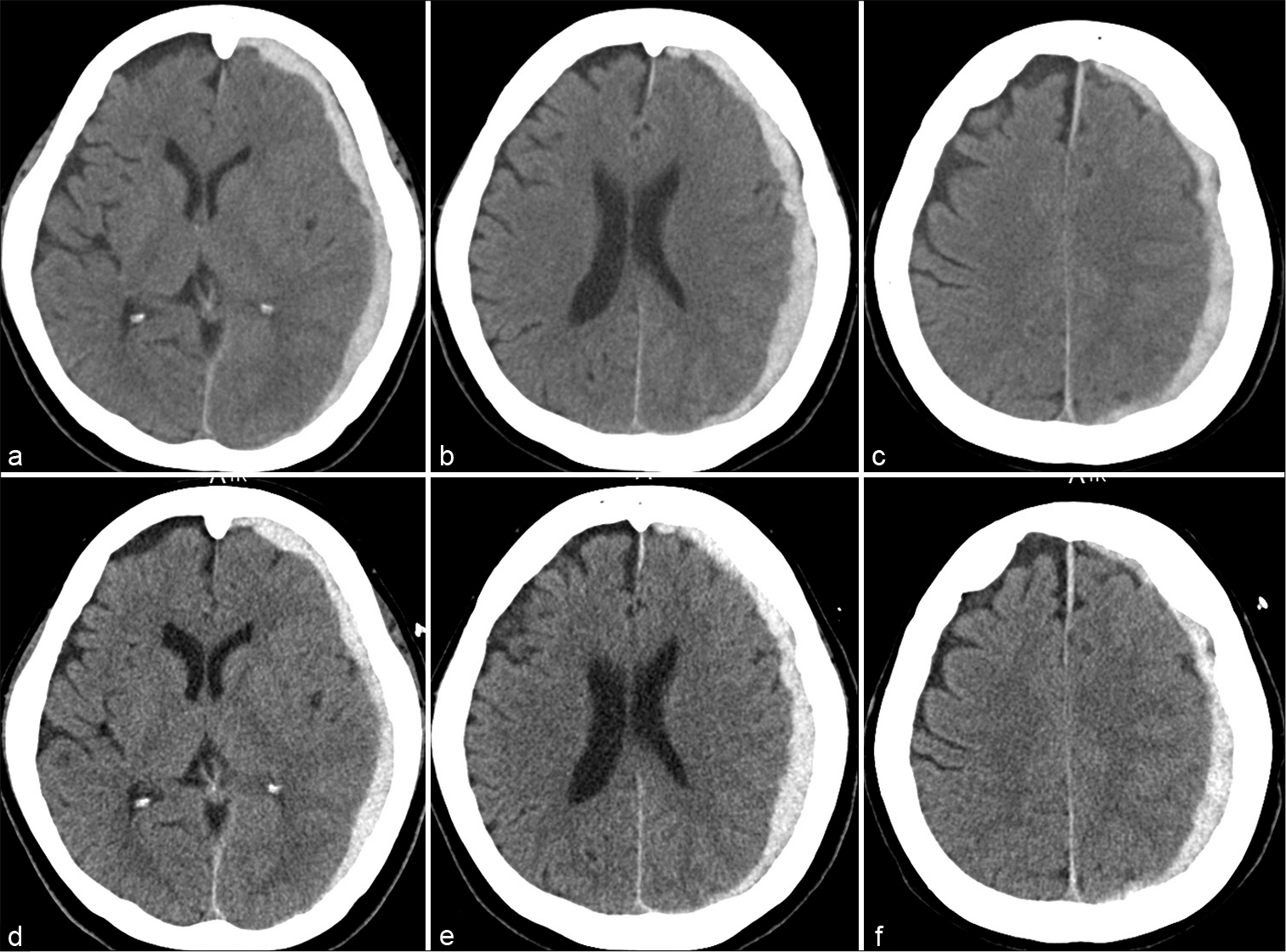
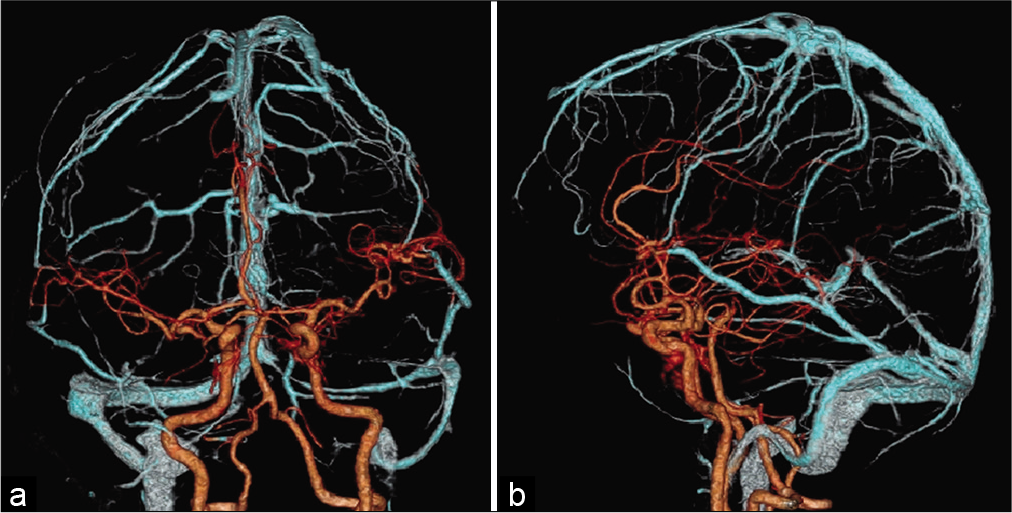
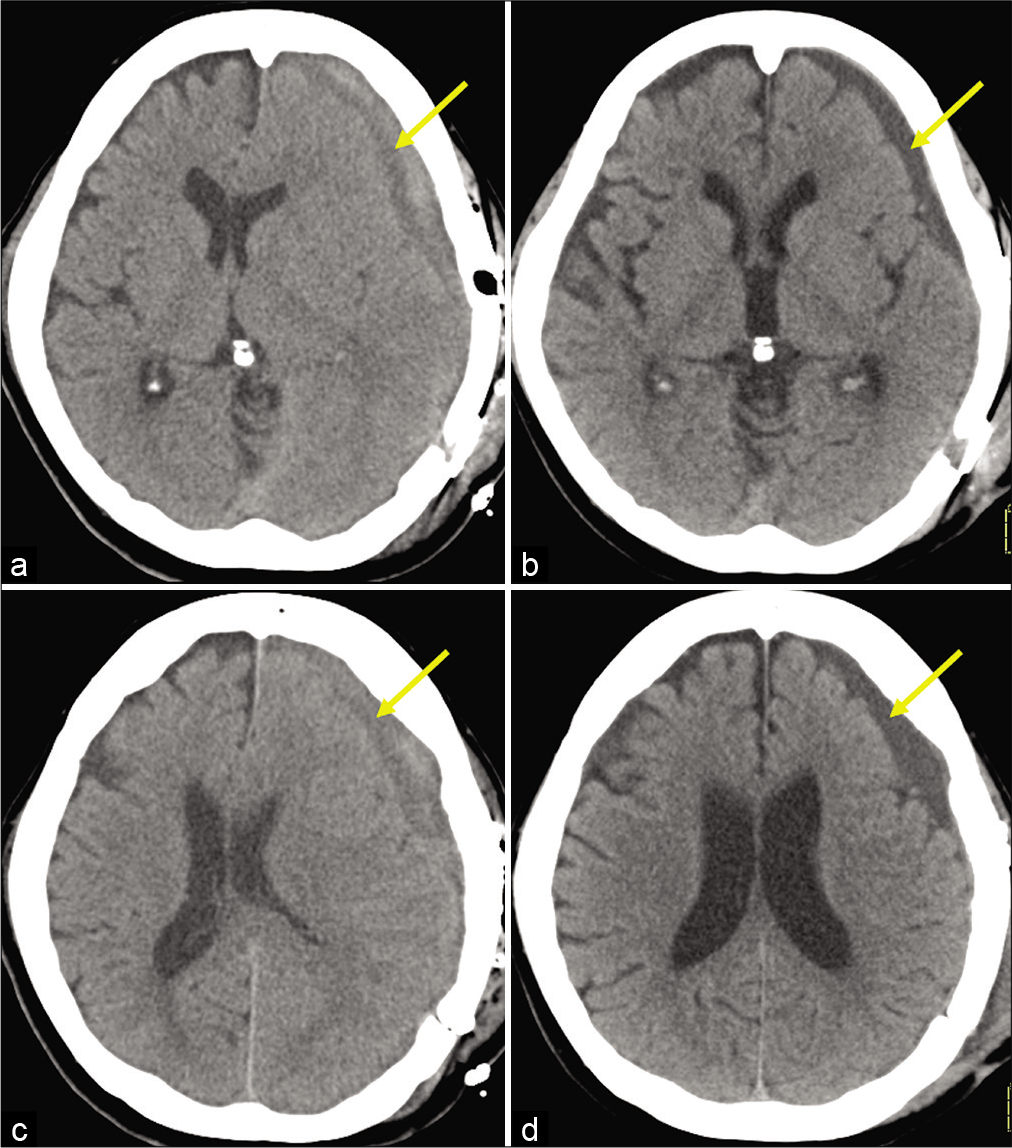
A 50-year-old hypertensive woman presented to the emergency department of our hospital presenting headache while shopping. There was no history of preceding falls or head injuries. She had not been administered steroids, anticoagulants, or antiplatelet agents. At presentation, the patient was fully awake and did not exhibit any focal neurological deficits. The blood pressure was 176/113 mmHg, and blood examination revealed normal findings. Cranial computed tomography (CT) revealed a subtly compressive, apparently ASDH in the left cerebral convexity. It was 15 mm in thickness without displacement of midline structures and showed a regression in 1 day with resolution of the headache [
Figure 3:
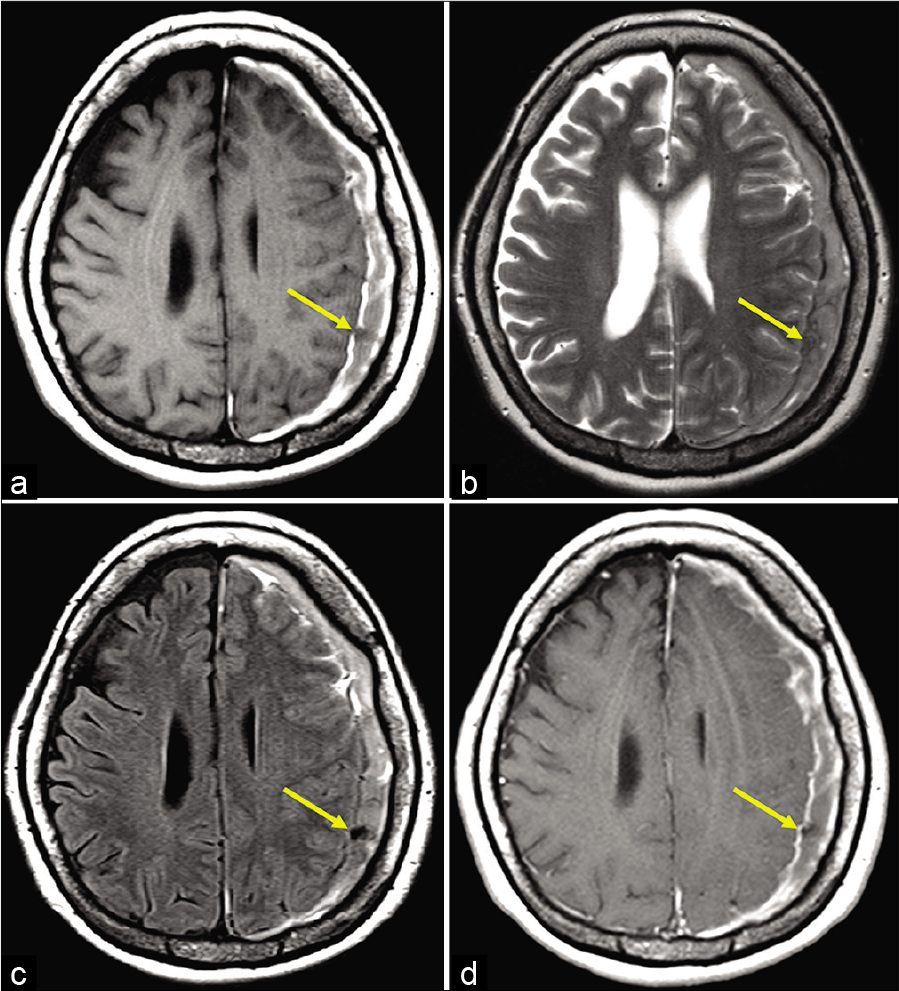
Non-contrast axial T1- (a), T2-weighted- (b), fluid attenuated inversion recovery-(c), and post-contrast axial T1-weighted magnetic resonance imaging (d), performed on post hospitalization day 6, showing a non-enhancing, nodular lesion in the subdural hematoma, adjacent to the left parietal cortex (a-d, arrow).
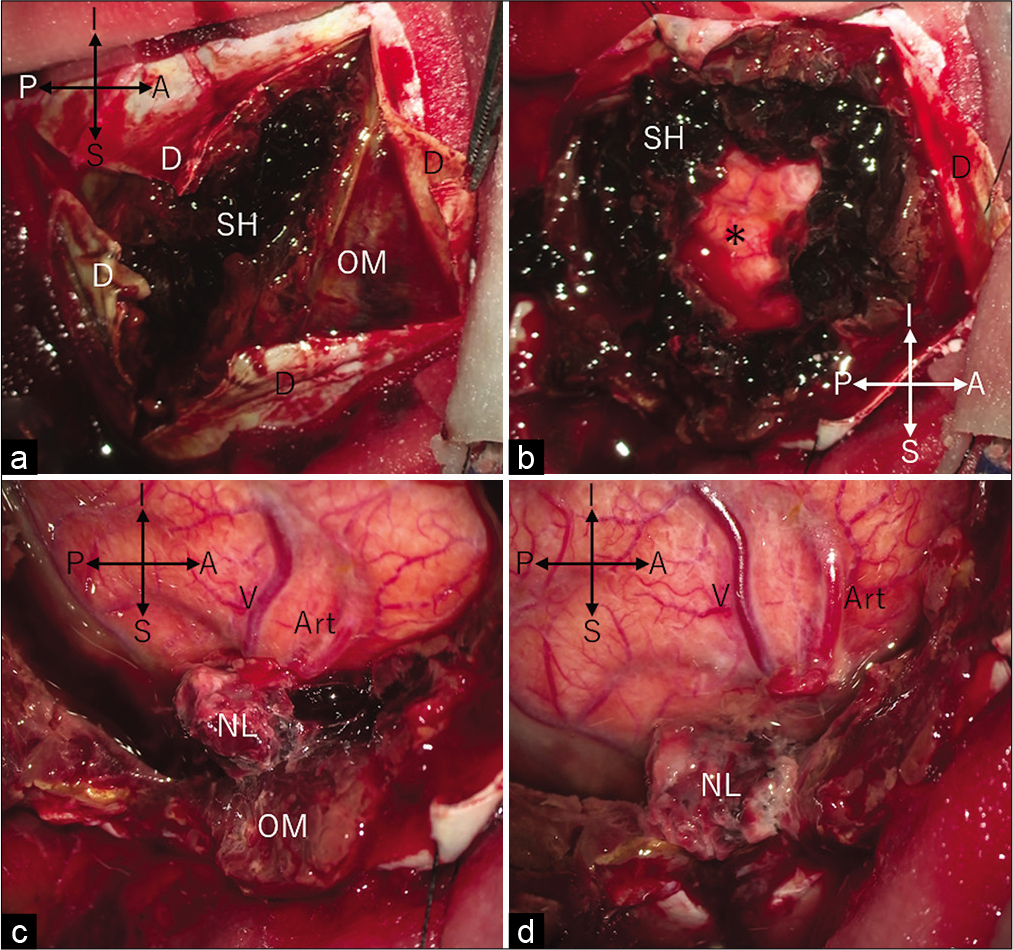
Figure 5:
Intraoperative photos showing, on reflection of the dura mater, a bi-layered subdural hematoma comprising a thick outer membrane and inner semisolid clots (a), intact cortical surface exposed after hematoma evacuation (b), nodular lesion adhering to the outer membrane of the hematoma and the arachnoids (c), and nodular lesion separate from the arachnoids with intact cortical vessels coursing underneath (d). A: anterior; Art: cortical artery; D: dura mater; I: inferior; NL: nodular lesion; OM: outer membrane of hematoma; P: posterior; S: superior; SH: semisolid hematoma; V: cortical vein; and Asterisk: cortical surface.
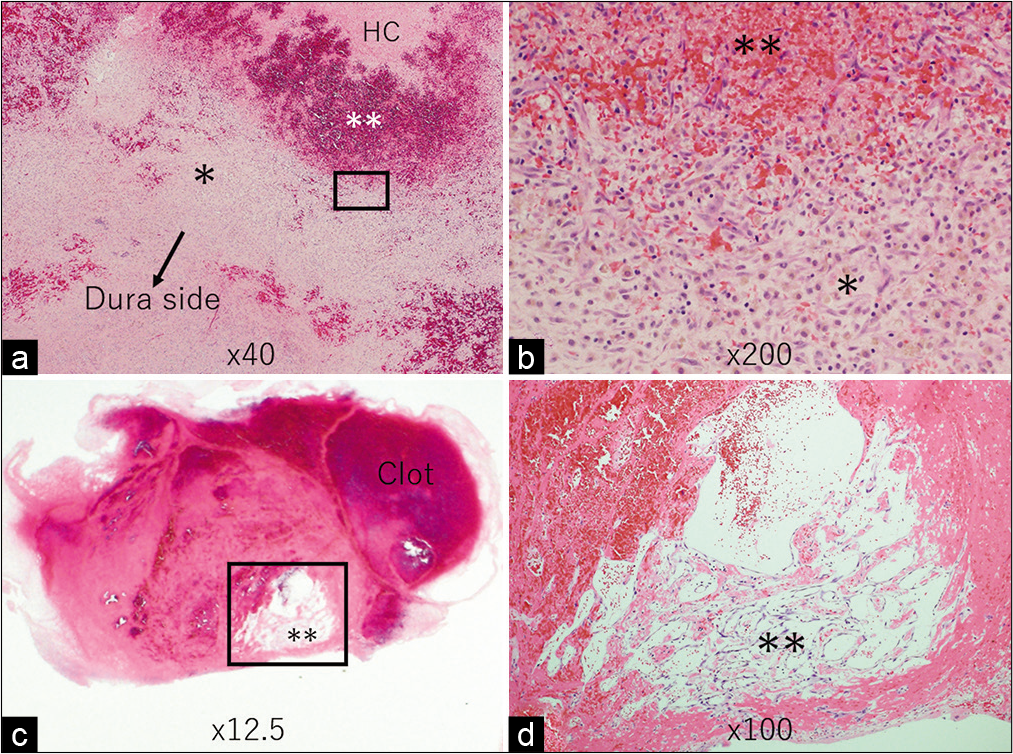
Figure 6:
Photomicrographs of the resected outer membrane (a and b) and nodular lesion (c and d) showing microvascular proliferation present in the outer membrane, adjacent to the hematoma cavity, and within the nodular lesion. (b and d) represent magnified views of the square areas in (a and c), respectively. (a-d) Hematoxylin and eosin stain. HC: Hematoma cavity; *Fibrous connective tissue; **Microvascular proliferation.
DISCUSSION
In the present case, the presumed non-traumatic ASDH initially showed spontaneous regression, but then transformed into an organized CSDH and markedly enlarged in the following 2 weeks. Despite careful observation, the exact cause of the ASDH and its original site were not identified in this case, although the existing condition of hypertension might have acted as a risk factor for the development of the hemorrhage.[
In the present case, the organized CSDH was managed by partial removal of the outer membrane and the associated subdural clots through a craniotomy. The size of the craniotomy was much smaller than the whole extension of the hematoma because we predicted that the subdural hematoma was in a fluid state and could be evacuated through the small cranial window. However, similar to a previous study, the residual hematoma resolved spontaneously following the partial removal.[
CONCLUSION
Development of microvascular proliferation in the clots of an ASDH may lead to its rapid enlargement as an organized CSDH. Organized CSDHs can be managed by partial, instead of extensive, removal of the outer membrane, and the included hematoma through a craniotomy.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Amano T, Miyamatsu Y, Otsuji R, Nakamizo A. Efficacy of endoscopic treatment for chronic subdural hematoma surgery. J Clin Neurosci. 2021. 92: 78-84
2. Chen K, Wang K, Chen D, Niu H, Yang S, Wang Y. Surgical procedure in the treatment of organized chronic subdural hematoma: A single-center experience. J Neurol Surg A Cent Eur Neurosurg. 2021. 82: 241-7
3. Coombs JB, Coombs BL, Chin EJ. Acute spontaneous subdural hematoma in a middle-aged adult: Case report and review of the literature. J Emerg Med. 2014. 47: e63-8
4. de Oliveira A, da Silva Paiva W, Teixeira MJ. Rare acute idiopathic subdural hematoma: A case report and literature review. Surg Neurol Int. 2020. 11: 9
5. Edlmann E, Whitfield PC, Kolias A, Hutchinson PJ. Pathogenesis of chronic subdural hematoma: A cohort evidencing de novo and transformational origins. J Neurotrauma. 2021. 38: 2580-9
6. Fryburg K, Nguyen HS, Cohen-Gadol AA. Spontaneous acute subdural hematoma due to fondaparinux: Report of two cases. Surg Neurol Int. 2011. 2: 44
7. Lee KS, Bae WK, Doh JW, Bae HG, Yun IG. Origin of chronic subdural haematoma and relation to traumatic subdural lesions. Brain Inj. 1998. 12: 901-10
8. Lee KS. Chronic subdural hematoma in the aged, trauma or degeneration?. J Korean Neurosurg Soc. 2016. 59: 1-5
9. Moskala M, Goscinski I, Kaluza J, Polak J, Krupa M, Adamek D. Morphological aspects of the traumatic chronic subdural hematoma capsule: SEM studies. Microsc Microanal. 2007. 13: 211-9
10. Rathore L, Sahana D, Kumar S, Sahu RK, Jain AK, Tawari M. Rapid spontaneous resolution of the acute subdural hematoma: Case series and review of literature. Asian J Neurosurg. 2021. 16: 33-43
11. Tsutsumi S, Ogino I, Miyajima M, Nonaka S, Ito M, Yasumoto Y. Role of cathepsin K in the development of chronic subdural hematoma. J Clin Neurosci. 2017. 45: 343-7
12. Yadav YR, Ratre S, Parihar V, Bajaj J, Sinha M, Kumar A. Endoscopic management of chronic subdural hematoma. J Neurol Surg A Cent Eur Neurosurg. 2020. 81: 330-41
13. Yamashima T, Yamamoto S. How do vessels proliferate in the capsule of a chronic subdural hematoma?. Neurosurgery. 1984. 15: 672-8
14. Yamashima T. The inner membrane of chronic subdural hematomas: Pathology and pathophysiology. Neurosurg Clin N Am. 2000. 11: 413-24