- Department of Plastic Surgery, Apollo Gleneagles Hospital, Kolkata, West Bengal, India.
Correspondence Address:
Srinjoy Saha, Department of Plastic Surgery, Apollo Gleneagles Hospital, Kolkata, West Bengal, India.
DOI:10.25259/SNI_14_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Srinjoy Saha. Minimalistic reconstruction of exposed skull in a complex craniovertebral polytrauma. 31-May-2021;12:248
How to cite this URL: Srinjoy Saha. Minimalistic reconstruction of exposed skull in a complex craniovertebral polytrauma. 31-May-2021;12:248. Available from: https://surgicalneurologyint.com/surgicalint-articles/10835/
Abstract
Background:
Case Description: A sizeable 10 × 6.5 cm forehead defect was reconstructed utilizing regenerative principles under local anesthesia and sedation in a 54-year-old woman. After adequate debridement of gangrenous soft tissues, exposed outer skull bones were trephined, forehead defect covered with a synthetic biomaterial, and the patient was discharged thereafter. Granulating neodermis regenerated within the biomaterial over the next 6 weeks. Weekly platelet-rich plasma injections along the wound margins facilitated wound regeneration. Dimensions reduced by two-thirds to 6.5 × 3.5 cm with wound regeneration and contraction, while granulating neodermis covered the remaining skull-bones. Split skin-grafting over the neodermis ensured satisfying long-term results, with similar color, texture, soft-tissue thickness, and sensation. Multiple occipitocervical, spinal, scapular, and rib fractures healed well with strict immobilization.
Conclusion: Good long-term results were achieved with significantly reduced dangers, complications, hospitalization, and costs than traditional reconstructive flap surgeries. Minimalistic reconstruction utilizing tissue engineering and regenerative medicine principles appears beneficial for patients with grave spinal injuries.
Keywords: Biodegradable temporising matrix, Craniovertebral injury, Forehead reconstruction, Minimally invasive reconstruction, Platelet-rich plasma
INTRODUCTION
Complicated anatomy of the skull base and cervical spine significantly challenge proper diagnosis and treatment of craniovertebral injuries.[
CASE PRESENTATION
Craniovertebral polytrauma
A 54-year-old woman was transferred to our neurosurgical intensive care from another hospital after surviving a high-speed automobile collision 2 days earlier. Computed tomograms revealed diffuse axonal injury of the brain along with concomitant craniovertebral fractures, including fractures over the right occipital condyle, seventh cervical vertebrae foramen transversarium anterior wall, and seventh cervical right lateral mass – lamina junction. Furthermore, fractures involving both scapulae, second to sixth ribs, and fifth dorsal vertebrae were observed in addition to bilateral pulmonary contusions and left hemothorax. Over the scalp, she had large degloving injuries with grease and road dirt sticking to the wounds. Debridement and primary closure of the degloved scalp tissues were initially performed by the treating neurosurgeon. The patient was stabilized in intensive care and closely monitored for her cranial, cervical, and pulmonary injuries. Taylor’s brace and Philadelphia collar were applied after her relatives preferred conservative management.
Minimalistic reconstruction
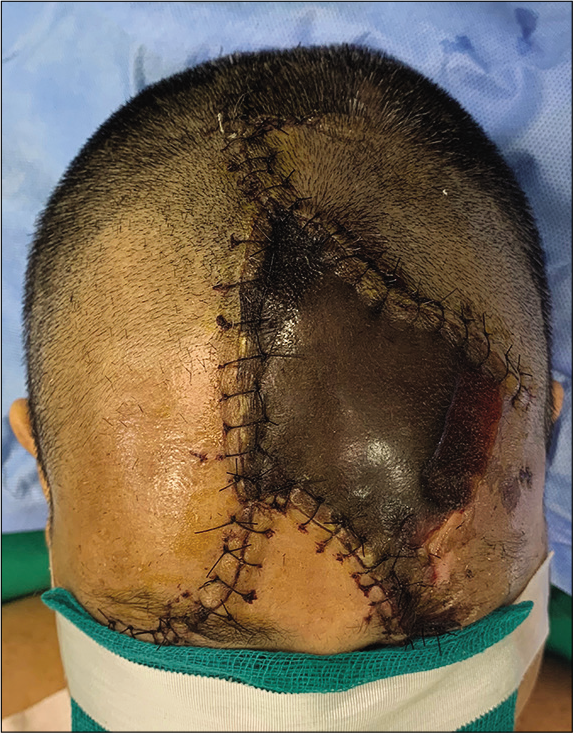
After the amelioration of life-threatening medical conditions, a plastic surgical referral was received for managing the necrosed degloved skin over her left forehead. Proper counseling of different options for forehead reconstruction followed. Finally, we decided to perform smaller surgeries under minimal anesthesia, while strictly maintaining her spinal immobilization with a collar and brace. Under sedation and local anesthesia, necrotic areas were debrided along the demarcation margins, resulting in a 10 cm × 6.5 cm forehead and scalp defect, including 9 cm × 5 cm area of barren skull bones without any periosteal cover [
RESULTS
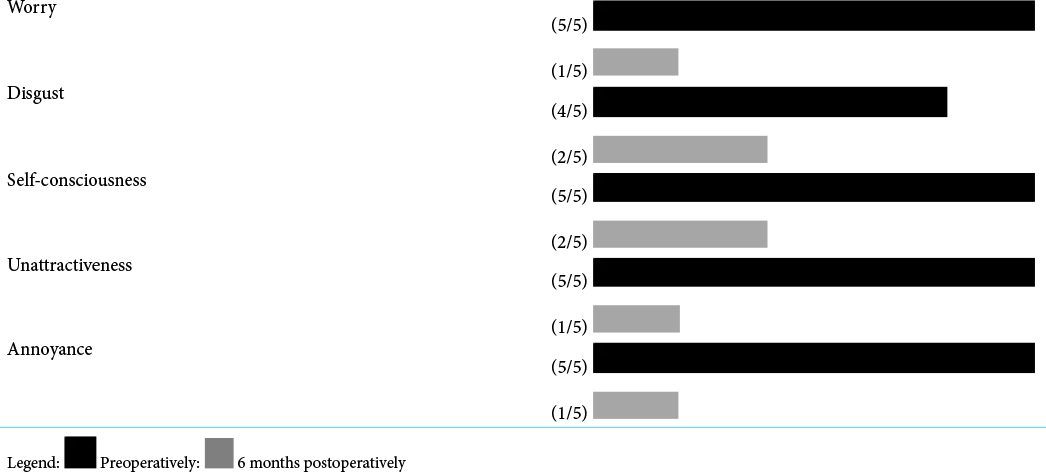
Removal of the outer semi-permeable film layer after 5 weeks showed significant wound regeneration and contraction, shortening the wound dimensions to 6.5 cm × 3.5 cm. Thus, wound areas had reduced substantially by approximately two-thirds, from 65 cm2 initially to 23 cm2 eventually, with granulating neodermis formation within the inner scaffold [
DISCUSSION
Occipital condylar fractures are potentially dangerous and require careful attention in unconscious patients.[
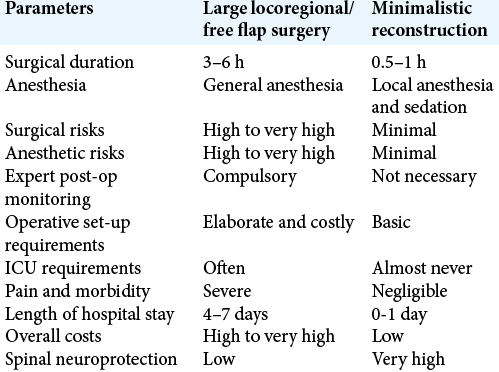
Reconstructing large (>20 cm2) forehead defects usually require sizeable loco-regional flaps or free tissue transfers. Loco-regional flaps, comprising substantial tissues from the adjacent forehead and scalp, are transposed, rotated, or advanced to cover the tissue defect. A wide flap-base with extensive dissection and undermining is necessary to preserve vascularity to the flap-edges.[
While performing loco-regional flaps and free tissue transfers, rotating and positioning the headneck junction are imperative several times to facilitate flap transfer and suturing.[
Platelets are anucleate derivatives of megakaryocytes that roam in the peripheral bloodstream for 7–10 days after migrating from the bone marrow. Activated, it releases several growth factors and cytokines for about 1 week, which possess angiogenic, mitogenic, and chemotactic properties. Autologous PRP is obtained after centrifuging the patient’s venous blood to concentrate platelets, wherein platelet counts exceed 1-million/microliter, roughly 5 times the baseline values.[
CONCLUSION
Minimalistic reconstruction achieved an equivalent functional and aesthetic result when compared to reconstructive flap- surgeries, but with significantly reduced dangers, chances of complications, and hospitalization, while lowering treatment costs. This case was performed at the height of the covid pandemic period, when regular hospital services were severely curtailed. In spite of limited available resources, it worked wonderfully and safely. It may become an apt model for reconstructing exposed skull-bones in the presence of significant craniovertebral injuries, especially in places and situations with limited medical resources.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Bao FP, Zhang HG, Zhu SM. Anesthetic considerations for patients with acute cervical spinal cord injury. Neural Regen Res. 2017. 12: 499-504
2. Conde-Montero E, de la Cueva Dobao P, Martínez González JM. Platelet-rich plasma for the treatment of chronic wounds: Evidence to date. Chronic Wound Care Manag Res. 2017. 4: 107-20
3. Costa DJ, Walen S, Varvares M, Walker R. Scalp rotation flap for reconstruction of complex soft tissue defects. J Neurol Surg B Skull Base. 2016. 77: 32-7
4. Dagtekin A, Avci E, Hamzaoglu V, Ozalp H, Karatas D, Esen K. Management of occipitocervical junction and upper cervical trauma. J Craniovertebr Junction Spine. 2018. 9: 148-55
5. Diedrich DA, Rose PS, Brown DR. Airway management in cervical spine injury. Curr Anesthesiol Rep. 2013. 3: 197-204
6. Drosou A, Trieu D, Goldberg LH. Scalpel-made holes on exposed scalp bone to promote second intention healing. J Am Acad Dermatol. 2014. 71: 387-8
7. Greenwood JE, Wagstaff MJ, Rooke M, Caplash Y. Reconstruction of extensive calvarial exposure after major burn injury in 2 stages using a biodegradable polyurethane matrix. Eplasty. 2016. 16: e17
8. Krüger A, Oberkircher L, Frangen T, Ruchholtz S, Kühne C, Junge A. Fractures of the occipital condyle clinical spectrum and course in eight patients. J Craniovertebr Junction Spine. 2013. 4: 49-55
9. Larrañaga J, Rios A, Franciosi E, Mazzaro E, Figari M. Free flap reconstruction for complex scalp and forehead defects with associated full-thickness calvarial bone resections. Craniomaxillofac Trauma Reconstr. 2012. 5: 205-12
10. Saha S. Triple-plane dissection of combined forehead and scalp flaps for large posttraumatic forehead defects. Int J Recent Surg Med Sci. 2020. 6: 24-9
11. Ueda S, Sasaki N, Fukuda M, Hoshimaru M. Surgical treatment for occipital condyle fracture, C1 dislocation, and cerebellar contusion with hemorrhage after blunt head trauma. Case Rep Orthop. 2016. 2016: 8634831
12. Volakakis E, Papadakis M, Manios A, Ioannou CV, Zoras O, de Bree E. Platelet-rich plasma improves healing of pressure ulcers as objectively assessed by digital planimetry. Wounds. 2019. 31: 252-6











Dinesh Naidoo
Posted June 6, 2021, 6:51 am
Excellent cosmetic result very comparable to what would have been achievable with a graft