- Department of Neurosurgery, University of Cincinnati, Cincinnati, United States,
- Department of Neurosurgery, Neurosurgery Teaching Hospital, Al-Risafa, Baghdad, Iraq,
- Department of Neurosurgery, University of Baghdad, Al-Karkh, Baghdad, Iraq,
- Department of Otolaryngology Head and Neck Surgery, University of Cincinnati, Cincinnati, Ohio, United States
Correspondence Address:
Samer S. Hoz, Department of Neurosurgery, University of Cincinnati, Cincinnati, Ohio, United States.
DOI:10.25259/SNI_585_2024
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Samer S. Hoz1, Paolo Palmisciano1, Mustafa Ismail2, Ahmed Muthana3, Edward J. Doyle1, Mark D. Johnson1, Jonathan A. Forbes1, Charles J. Prestigiacomo1, Ravi Samy4, Mario Zuccarello1, Norberto Andaluz1. Minimally invasive presigmoid retrolabyrinthine suprameatal approach (PRSA): A cadaveric study for accessing premeatal anterior inferior cerebellar artery (AICA) aneurysms. 04-Oct-2024;15:364
How to cite this URL: Samer S. Hoz1, Paolo Palmisciano1, Mustafa Ismail2, Ahmed Muthana3, Edward J. Doyle1, Mark D. Johnson1, Jonathan A. Forbes1, Charles J. Prestigiacomo1, Ravi Samy4, Mario Zuccarello1, Norberto Andaluz1. Minimally invasive presigmoid retrolabyrinthine suprameatal approach (PRSA): A cadaveric study for accessing premeatal anterior inferior cerebellar artery (AICA) aneurysms. 04-Oct-2024;15:364. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=13128
Abstract
Background: The surgical management of aneurysms involving the proximal third of the anterior inferior cerebellar artery (AICA) usually necessitates complex and invasive approaches, thus posing major challenges. We aimed to investigate the infratentorial presigmoid retrolabyrinthine suprameatal approach (PRSA) as a surgical corridor for premeatal AICA aneurysms.
Methods: We performed 10 PRSA dissections in five cadaveric heads. Twelve morphometric parameters were measured, analyzed, and categorized into pre-procedural, intra-procedural, and additional parameters. The typical anatomic-radiological characteristics and variations were evaluated, and the related anatomical and radiological parameters were analyzed to predict surgical accessibility.
Results: Preoperative anatomic-radiological parameters provide valuable information to select patients with favorable anatomy that may offer appropriate surgical accessibility to the premeatal AICA through a PRSA corridor. The position of the basilar artery from the midline determines the degree of accessibility to the origin of AICA through the infratentorial PRSA. The PRSA for targeting proximal AICA aneurysms was also compared to other surgical approaches based on the available current literature.
Conclusion: Premeatal AICA aneurysms can be accessed and clipped through the infratentorial PRSA corridor. This would allow surgeons to avoid the sacrifice of hearing and balance as compared to other available invasive alternative approaches. The selection of the appropriate patients should be based on the individualized preoperative radiological characteristics for both the vascular and bony anatomy.
Keywords: Aneurysm, Anterior inferior cerebellar artery, Clipping, Posterior skull base, Presigmoid, Retrolabyrinthine, Sigmoid sinus
INTRODUCTION
Aneurysms involving the proximal third of the anterior inferior cerebellar artery (AICA) may arise from the basilar artery (BA)-AICA origin or from the AICA segments proximal to the internal auditory canal (IAC). The surgical management of these aneurysms is particularly challenging due to their location posterior to the middle of the clivus and the petrous apex, anterior to the cranial nerve (CN)-VII/VIII complex, and inferior to CN-V.[
In this anatomical study, we evaluated the feasibility of a minimally invasive presigmoid retrolabyrinthine suprameatal approach (PRSA) to expose the proximal AICA segments at the level of the lateral prepontine and cerebellopontine angle (CPA) cisterns.
MATERIALS AND METHODS
Five adults, formalin-fixed, triple-injected[
Surgical technique
A mastoidectomy followed by a classic retrolabyrinthine approach characterized the initial stage of the surgery. The next stage included the drilling of the posterior part of the petrous apex superior to the IAC through the presigmoid mastoidectomy, thus creating the retrolabyrinthine suprameatal corridor. This provided a multiangled exposure contemplated with effective micro-surgical maneuverability, exposing the AICA from its origin to the IAC.
Morphometric measurements
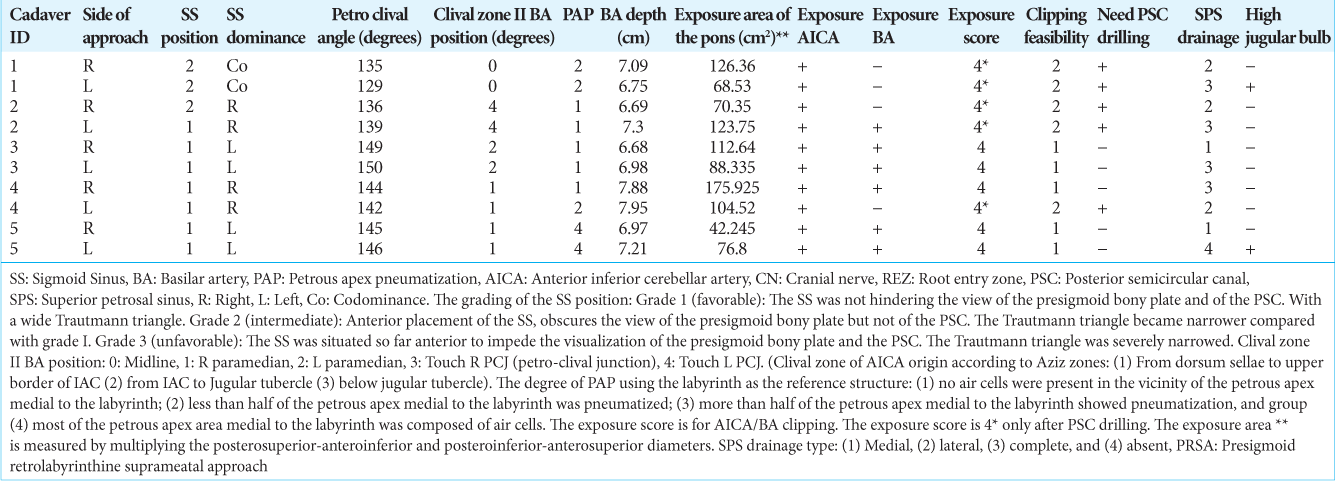
Twelve morphometric parameters were measured, analyzed, and categorized into pre-procedural, intra-procedural, and additional parameters.
The pre-procedural parameters were analyzed on pre-procedural head CT scans and used for surgical planning: (I) sigmoid sinus (SS) position,[
Figure 1:
(a) Depiction of the clival zone II with the longitudinal classification of the basilar artery (BA) position in relation to the midline. The red bar indicates the BA position within clival zone, which extends from the internal auditory canal (IAC) to the jugular tubercle into: grade-0, midline; grade-1, right paramedian; grade-2; left paramedian; grade-3, right petro-clival junction, and grade-4, left petro-clival junction. (b-d) Post-procedural cranial computed tomography scans showing the anterior inferior cerebellar artery (AICA) clipping using the presigmoid retrolabyrinthine suprameatal approach (PRSA) approach. (b) 3D reconstruction of right side PRSA craniotomy, (c) axial, and (d) sagittal sections showing the final position of the aneurysmal clip (red arrow) on the AICA origin from BA.
The intra-procedural parameters were assessed within the surgical field during the cadaveric dissection: (VI) BA depth (if the BA was not exposed, this distance was measured using the midline as a reference); (VII) arterial exposure (i.e., AICA and BA); (VIII) clipping feasibility, which classified the ease of aneurysmal clips application on the exposed BA and premeatal AICA segment into grade-1 if clipping was feasible, grade-2 if clipping was feasible with some difficulty, and grade-3 if clipping was not feasible; (IX) exposure area of the pons in cm2, measured by multiplying the longest posterosuperioranteroinferior and posteroinferior-anterosuperior diameters; and (X) exposure score,[
The additional parameters included (XI) the need for PSC drilling and (XII) the presence of a high jugular bulb.
RESULTS
The pre-procedural anatomic-radiological parameters proved to be able to provide valuable information to select patients with favorable anatomy that may offer appropriate surgical accessibility to the premeatal AICA through a PRSA corridor [
The median (IQR) BA depth was 7.04 cm (0.47 cm). The AICA was exposed on all ten sides, and the BA was exposed on eight sides. The median (IQR) of the exposure area of the pons was 94.4 cm2 (49 cm2). The exposure score was four in all specimens (three sides required PSC drilling), and clipping was feasible in all specimens (grade-2 on two sides) [
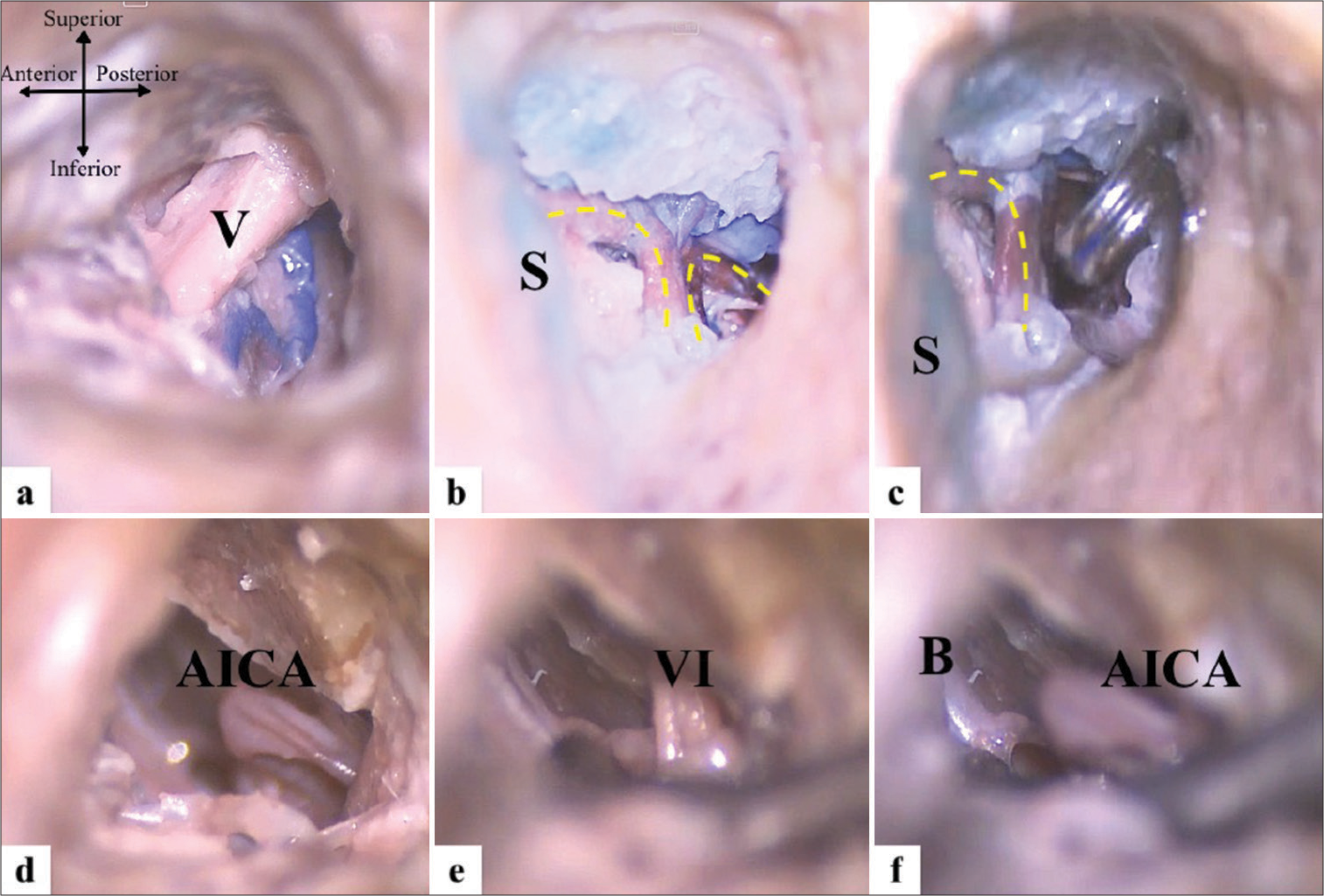
Figure 2:
Operative steps on injected cadaver head showing the extent of the minimally invasive bone cavity of left side presigmoid retrolabyrinthine suprameatal approach: (a-c) Microscopic views exposing the cranial nerve (CN)-V, and then exposing and clipping the premeatal anterior inferior cerebellar artery (AICA); (d-f) endoscopic views of the operative field for the same cadaver, using 0° and 30° scopes showing the relation of the AICA to the surrounding structures. V: Trigeminal nerve, VI: Abducent nerve, B: Basilar artery, S: Sigmoid sinus, AICA: Anterior inferior cerebellar artery.
Figure 3:
Artistic depiction of the presigmoid retrolabyrinthine suprameatal approach with the exposed anterior inferior cerebellar artery (AICA) and related operative anatomy. The dashed line indicates the drilled bone of the posterior petrous apex above the IAC. AICA: Anterior inferior cerebellar artery, C: Cerebellum, EAC: External auditory canal, P: Pons, S: Sigmoid sinus, SCC: Semicircular canals, V: Trigeminal nerve, VI: Abducent nerve, *:Facial nerve complex. Illustration prepared by Ahmed Muthana and courtesy of Samer Hoz. Asterix is defined in blue highlight. the red line is part of the illustration, and it depicts the anterior inferior cerebellar artery (AICA).
On post-procedure CT scans, an absent superior petrosal sinus (SPS) was noted on two sides and a high jugular bulb on the other two sides. The endoscope was utilized to confirm the course of the exposed BA and bilateral AICAs by following them to their origin with the parent arteries and also to inspect the surrounding critical perforators after the placement of the aneurysm clip.
DISCUSSION
The presigmoid approach per se has been extensively analyzed and recently classified in the literature.[
AICA aneurysms are classified according to the four AICA segments: anterior pontine, lateral pontine, flocculonodular, and cortical. The first 2 segments are considered the premeatal AICA segments. Endovascular strategies are preferred for aneurysms arising from the BA-AICA origin up to the IAC segment, and surgery is favored for more distal aneurysms. Operative strategies for proximal AICA aneurysms may include direct clipping, wrapping, or trapping with direct bypass.[
Anatomy and landmarks of the PRSA
While performing the PRSA, we primarily tracked the course of the premeatal AICA up to the midline in the retroclival area. We found that multiple preoperative anatomic-radiological parameters can impact patient selection. The main parameters of interest include (1) BA position at the level of the clival zone II; (2) obtuse petro-clival angle (≥144°); and (3) SS position and the volume of the mastoid cavity. Among our specimens, 5 sides (50%) showed a ≥144° angle, achieving an optimal operative trajectory that exposed the full course of the pre-meatal AICA with the feasible and straightforward dissection and clip application. In addition, more posterior SS positions provide a more feasible approach through working in a relatively wide mastoid cavity. These grades should be assessed through a CT scan in the preoperative planning phase. Other parameters with moderate planning value are the type of SPS drainage and the degree of PAP. AICA contains several sets of perforators distributed along its segments. The first segment represents the premeatal segment, containing 2–8 perforators supplying the brainstem around the entry zone of the trigeminal, facial, and vestibulocochlear nerves; middle cerebellar peduncle and the adjacent part of the pons; and the choroid plexus of the CPA, the superolateral medulla, and the glossopharyngeal and vagus nerves.[
The BA position from the midline determines the accessibility of the origin of AICA from the BA through a PRSA corridor, and it should be measured at the level of any surgical approach due to the common variations and tortuosity of the BA course. For this reason, we analyzed the BA position at the middle clival area (also called Aziz’s clival zone II[
Based on our anatomic study, we found that the full course of premeatal AICA can be exposed with the PRSA, which allows to treat of aneurysms located in the premeatal segment of AICA at the AICA origin and proximal to IAC. The exposed area comprises a trapezoid that connects the IAC, the CN-VI, the CN-V, and the BA groove. Clipping was feasible in most of the specimens with some difficulty in certain specimens. The grading of clipping feasibility was based on the expertise of our trainees and surgeons. The results should be interpreted with caution, and larger clinical trials are recommended to achieve a more standardized consensus following Delphi guidelines.[
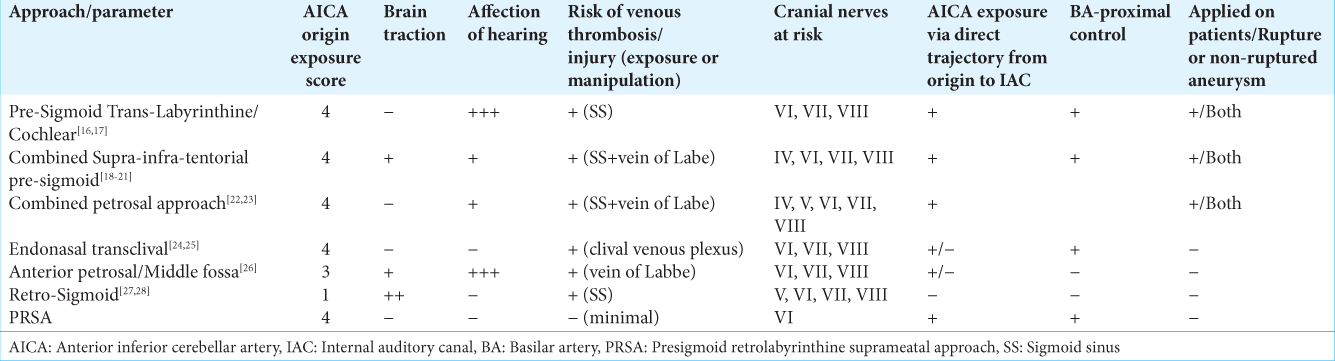
Comparison of PRSA with other approaches for BA/AICA aneurysms
When comparing different skull base approaches for AICA origin aneurysms, the variables that need to be considered include the extent of bone resection, brain retraction, and technical feasibility. For the posterolateral approaches to the petro-clival region, the retrosigmoid approach offers minimal bone resection with significant brain retraction to approach this region. However, since the retrosigmoid region is routinely used in clinical practice, most neurosurgeons are well-versed in this approach, resulting in technical expertise and minimizing morbidity. The transcochlear approach is associated with maximal bone resection and minimal brain retraction but requires neurotology expertise for the approach and results in hearing and vestibular loss. As regards the PRSA, moderate bone resection and minimal brain retraction are needed while providing reasonable surgical exposure.
When performing a comprehensive search of the literature, different approaches to the BA/AICA aneurysms have been described, each with its limitations and opportunities. To better define the possible advantages in terms of exposures and risks of our proposed PRSA, we provided a detailed description of the other approaches for accessing BA/AICA aneurysms [
The most common standard lateral skull base approaches may carry low morbidity when properly executed but are often unable to provide proper exposure of the AICA origin, thus necessitating larger exposures and increasing the chances of intraoperative complications. The presigmoid window may be offered as an addition to the subtemporal approach. However, we noted that temporal lobe exposure, retraction, and tentorial resection are often not necessary. We have consistently observed the presence of the proximal AICA in our surgical field when employing our proposed approach. These findings prompted us to explore the presigmoid window as a viable access point for these difficult lesions, which occasionally lack suitable surgical or endovascular alternatives.
There are numerous advantages of the PRSA over the classic transcochlear, presigmoid supra-infra-tentorial, and combined transpetrosal, trans-sigmoid, and endoscopic transclival approaches. The most important comprises the limited mastoid drilling, the avoidance of exposure and traction of the SS, and the preservation of the SPS, labyrinthine, cochlea, and CN-VII functions. In addition, the avoidance of the retraction of the temporal lobe and cerebellum, coupled with the preservation of the vein of Labbe, characterize critical differences in the PRSA as compared to other lateral and posterolateral approaches targeting the area of the petro-clival region between the IAC and the upper border of the jugular tubercle (clival zone II).[
Limitations
The PRSA corridor has some limitations. The proximal AICA can be exposed and manipulated through the minimally invasive PRSA. However, large lesions that require wide exposure, ruptured aneurysms with considerable hematoma, and unfavorable anatomy may pose some difficulties. Real surgical nuances and complications cannot be assessed fully through cadaveric studies. Thus further clinical implication seems to represent a mandatory step in advocating where and when to use such minimally invasive approaches. As the primary aim of this study was to propose our minimally invasive technique to tackle BA/AICA aneurysms, we did not perform cadaveric dissections to compare different approaches, but we searched the literature to identify the potential benefits and limitations of our approach in comparison to others. Future work is warranted to complete further comparative cadaveric dissections.
CONCLUSION
The premeatal AICA aneurysms can be accessed and clipped through the infratentorial PRSA corridor. This approach allows the preservation of hearing and balance as compared to other available invasive alternative approaches. The selection of the appropriate patients should be based on the individualized preoperative radiological characteristics for both the vascular and bony anatomy.
Ethical approval
The Institutional Review Board approval is not required, as it is cadaveric study.
Declaration of patient consent
Patient’s consent was not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
Acknowledgments
We acknowledge Ahmed Muthana for providing the graphical illustration [Figure 3].
References
1. Aljuboori Z, Hoz SS, Al-Sharshahi ZF, Ding D, Andaluz N. Surgical clipping of a ruptured distal anterior inferior cerebellar artery aneurysm: A technical note. Cureus. 2021. 13: e18688
2. Abdel Aziz KM, Sanan A, van Loveren HR, Tew JM, Keller JT, Pensak ML. Petroclival meningiomas: Predictive parameters for transpetrosal approaches. Neurosurgery. 2000. 47: 139-50
3. Bambakidis NC, Manjila S, Dashti S, Tarr R, Megerian CA. Management of anterior inferior cerebellar artery aneurysms: An illustrative case and review of literature. Neurosurg Focus. 2009. 26: E6
4. Bernardo A, Evins AI, Visca A, Stieg PE. The intracranial facial nerve as seen through different surgical windows: An extensive anatomosurgical study. Neurosurgery. 2013. 72: ons194-207
5. Bocanegra-Becerra JE, Acha Sánchez JL, Contreras Montenegro L, Cueva M, Bellido A, Contreras S. Exoscopic clipping of a ruptured posterior communicating artery aneurysm through a minipterional approach: 2-dimensional operative video. Oper Neurosurg. 2022. p. 10.1227
6. Chanda A, Nanda A. Partial labyrinthectomy petrous apicectomy approach to the petroclival region: An anatomic and technical study. Neurosurgery. 2002. 51: 147-60
7. Day JD, Fukushima T, Giannotta SL. Cranial base approaches to posterior circulation aneurysms. J Neurosurg. 1997. 87: 544-54
8. Dexian Tan A, Ng JH, Lim SA, Low DY, Yuen HW. Classification of temporal bone pneumatization on high-resolution computed tomography: Prevalence patterns and implications. Otolaryngol Head Neck Surg. 2018. 159: 743-9
9. Doan V, Lemos-Rodriguez AM, Sreenath SB, Unnithan A, Recinos PF, Zanation AM. Using the endoscopic endonasal transclival approach to access aneurysms arising from AICA, PICA, and vertebral artery: An anatomical study. J Neurol Surg B Skull Base. 2016. 77: 207-11
10. Drake CG, Peerless SJ, Hernesniemi JA, editors. Surgery of vertebrobasilar aneurysms: London, Ontario experience on 1767 patients. New York: Springer Science and Business Media; 2012. p.
11. Gonzalez LF, Alexander MJ, McDougall CG, Spetzler RF. Anteroinferior cerebellar artery aneurysms: Surgical approaches and outcomes--a review of 34 cases. Neurosurgery. 2004. 55: 1025-35
12. Gross BA, Tavanaiepour D, Du R, Al-Mefty O, Dunn IF. Petrosal approaches to posterior circulation aneurysms. Neurosurg Focus. 2012. 33: E9
13. Horgan MA, Delashaw JB, Schwartz MS, Kellogg JX, Spektor S, McMenomey SO. Transcrusal approach to the petroclival region with hearing preservation. Technical note and illustrative cases. J Neurosurg. 2001. 94: 660-6
14. Hou K, Xu K, Yu J. Endovascular treatment of anterior inferior cerebellar artery trunk aneurysms. Interv Neuroradiol. 2022. 28: 604-12
15. Hoz SS, Palmisciano P, Albairmani SS, Kaye J, Muthana A, Johnson MD. A proposed classification system for presigmoid approaches: A scoping review. J Neurosurg. 2023. 139: 965-71
16. Hoz SS, Palmisciano P, Ismail M, Sharma M, Muthana A, Forbes J. Anatomical study of the supratentorial extension for the retrolabyrinthine presigmoid approaches. World Neurosurg. 2024. 188: e120-7
17. Hoz SS, Sharma M, Palmisciano P, Johnson MD, Ismail M, Muthana A. Peritrigeminal safe entry zone access to anterolateral pons using the presigmoid retrolabyrinthine suprameatal approach: A Cadaveric morphometric study. Oper Neurosurg (Hagerstown). 2023. 25: e303-7
18. Humphrey-Murto S, Varpio L, Wood TJ, Gonsalves C, Ufholz LA, Mascioli K. The use of the Delphi and other consensus group methods in medical education research: A review. Acad Med. 2017. 92: 1491-8
19. Locksley HB, Sahs AL, Knowler L. Report on the cooperative study of intracranial aneurysms and subarachnoid hemorrhage. Section II. General survey of cases in the central registry and characteristics of the sample population. J Neurosurg. 1966. 24: 922-32
20. Quiñones-Hinojosa A, Chang EF, Lawton MT. The extended retrosigmoid approach: An alternative to radical cranial base approaches for posterior fossa lesions. Oper Neurosurg. 2006. 58: Ons-208-14
21. Rhoton AL. Microsurgical anatomy of the posterior fossa cranial nerves. Neurosurgery. 1979. 26: 398-462
22. Samii M, Ammirati M. The combined supra-infratentorial pre-sigmoid sinus avenue to the petro-clival region. Surgical technique and clinical applications. Acta Neurochir. 1988. 95: 6-12
23. Sanmillan JL, Lawton MT, Rincon-Torroella J, El-Sayed IH, Zhang X, Meybodi AT. Assessment of the endoscopic endonasal transclival approach for surgical clipping of anterior pontine anterior-inferior cerebellar artery aneurysms. World Neurosurg. 2016. 89: 368-75
24. Seifert V. Direct surgery of basilar trunk and vertebrobasilar junction aneurysms via the combined transpetrosal approach. Neurol Med Chir (Tokyo). 1998. 38: 86-92
25. Sekhar LN, Schessel DA, Bucur SD, Raso JL, Wright DC. Partial labyrinthectomy petrous apicectomy approach to neoplastic and vascular lesions of the petroclival area. Neurosurgery. 1999. 44: 537-50
26. Sincoff EH, McMenomey SO, Delashaw JB. Posterior transpetrosal approach: Less is more. Oper Neurosurg. 2007. 60: 53-9
27. Singh A, Irugu DV, Sikka K, Verma H, Thakar A. Study of sigmoid sinus variations in the temporal bone by micro dissection and its classification-a cadaveric study. Int Arch Otorhinolaryngol. 2019. 23: e311-6
28. Siwanuwatn R, Deshmukh P, Figueiredo EG, Crawford NR, Spetzler RF, Preul MC. Quantitative analysis of the working area and angle of attack for the retrosigmoid, combined petrosal, and transcochlear approaches to the petroclival region. J Neurosurg. 2006. 104: 137-42
29. Smith K, Ventre GJ, Palmisciano P, Hussein AE, Hoz SS, Forbes JA. Brain vasculature color-labeling using the triple-injection method in cadaveric heads: A technical note for improved teaching and research in neurovascular anatomy. Oper Neurosurg (Hagerstown). 2023. 24: 291-300
30. Spetzler RF, Daspit CP, Pappas CT. The combined supra-and infratentorial approach for lesions of the petrous and clival regions; experience with 46 cases. J Neurosurg. 1992. 76: 588-99
31. Suh SH, Kim DJ, Kim DI, Kim BM, Chung TS, Hong CK. Management of anterior inferior cerebellar artery aneurysms: Endovascular treatment and clinical outcome. AJNR Am J Neuroradiol. 2011. 32: 159-64
32. Thomas N, Maratos E, Barazi S. Combined supra-and infra-tentorial retro-labyrinthine pre-sigmoid approach. Curr Otorhinolaryngol Rep. 2019. 7: 195-9
33. Tjahjadi M, Niemelä M, Kivelev J, Serrone J, Maekawa H, Jahromi BR. Presigmoid approach to vertebrobasilar artery aneurysms: A series of 31 patients and review of the literature. World Neurosurg. 2016. 92: 313-22
34. Tomio R, Horiguchi T, Borghei-Razavi H, Tamura R, Yoshida K, Kawase T. Anterior transpetrosal approach: Experiences in 274 cases over 33 years. Technical variations, operated patients, and approach-related complications. J Neurosurg. 2022. 136: 413-21