- Department of Neurosurgery, Neurozone 3D Research Center, Lima, Peru.
Correspondence Address:
Cristian Eugenio SalazarCampos, Department of Neurosurgery, Neurozone 3D Research Center, Lima, Peru.
DOI:10.25259/SNI_239_2024
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Christian Alexander Yataco-Wilcas, Bruno Eduardo Diaz-Llanes, Yosimar Salomon Coasaca-Tito, Luis Alberto Lengua-Vega, Cristian Eugenio Salazar-Campos. Morphometric analysis of transsphenoidal surgery in Peruvian population. 10-May-2024;15:156
How to cite this URL: Christian Alexander Yataco-Wilcas, Bruno Eduardo Diaz-Llanes, Yosimar Salomon Coasaca-Tito, Luis Alberto Lengua-Vega, Cristian Eugenio Salazar-Campos. Morphometric analysis of transsphenoidal surgery in Peruvian population. 10-May-2024;15:156. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=12890
Abstract
Background: Transsphenoidal surgery has become a key element in the approach to skull base pathologies. The objective of the study was to explore the morphometry of the sphenoidal region in the Peruvian population, with an emphasis on understanding its specific anatomical characteristics and providing quantitative data for the planning of transsphenoidal surgery.
Methods: A cross-sectional study included a random sample of 81 cases of healthy individuals who presented to the Radiology Department of a Private Hospital Center in Peru over 1 year. Skull computed tomography scans without contrast were performed, and a detailed morphometric analysis was conducted by an expert neurosurgeon, including measurements of four parameters to evaluate the anatomy of the craniofacial region.
Results: Most participants exhibited complete sellar pneumatization, followed by incomplete sellar pneumatization, while conchal pneumatization was rare. Significant differences were found between men and women in the distance from the nasal opening to the dorsum of the sella turcica. No significant gender differences were observed in other anatomical measurements or significant changes with age in anatomical measurements.
Conclusion: Morphometric analysis provides crucial data for the precise customization of surgical interventions in the Peruvian population, especially in transsphenoidal surgery. The results highlight the importance of considering individual anatomical differences and gender variability during surgical planning. Morphometry emerges as a valuable tool to enhance the quality and safety of transsphenoidal surgery by adapting surgical strategies to the specific anatomical dimensions of each patient.
Keywords: Morphometry, Sellar anatomy, Sphenoidal pneumatisation, Transsphenoidal surgery, Anatomical measurements
INTRODUCTION
Transsphenoidal surgery has become a key element in the approach to sellar pathologies, especially in the treatment of pituitary adenomas and other conditions related to the pituitary gland.[
Through the implementation of endoscopes and micro-instruments, detailed visualization is achieved for precise excision of skull base lesions, thus minimizing the risk of damage to adjacent tissues.[
At present, the philosophy of “safe surgery” has become an essential paradigm in the field of surgical interventions, emphasizing the importance of detailed planning supported by precise anatomical measurements, not only to increase patient safety but also to improve surgical outcomes.[
Preoperative morphometric analysis of the sellar region in the Peruvian population emerges as an essential tool in planning transsphenoidal surgery, adding a crucial dimension to the precision and personalization of this neurosurgical approach. By meticulously evaluating the anatomical characteristics of the sella turcica and surrounding structures through tomographic imaging techniques, neurosurgeons can obtain specific and quantitative information about each patient’s anatomical variability.[
METHODS
Study participants
We conducted a cross-sectional study involving 81 randomly selected cases. These individuals, deemed healthy, were chosen from those who visited the Radiology Department of a Private Hospital Center in Peru between January 2023 and January 2024. The research protocol underwent review and approval by the Medical Ethics Committee of the same private hospital.
Image acquisition
Every patient underwent non-contrast computed tomography (CT) scans of their skull, and only images displaying morphometric features without alterations were used. These images were acquired using the equipment and techniques available in the Radiology Department of the Private Hospital Center. To take measurements on bone window images, we utilized a lightweight, fast, and intuitive medical image viewer, such as RadiAnt DICOM Viewer (Medixant, Poznan, Poland), ensuring optimal viewing conditions.
Image analysis
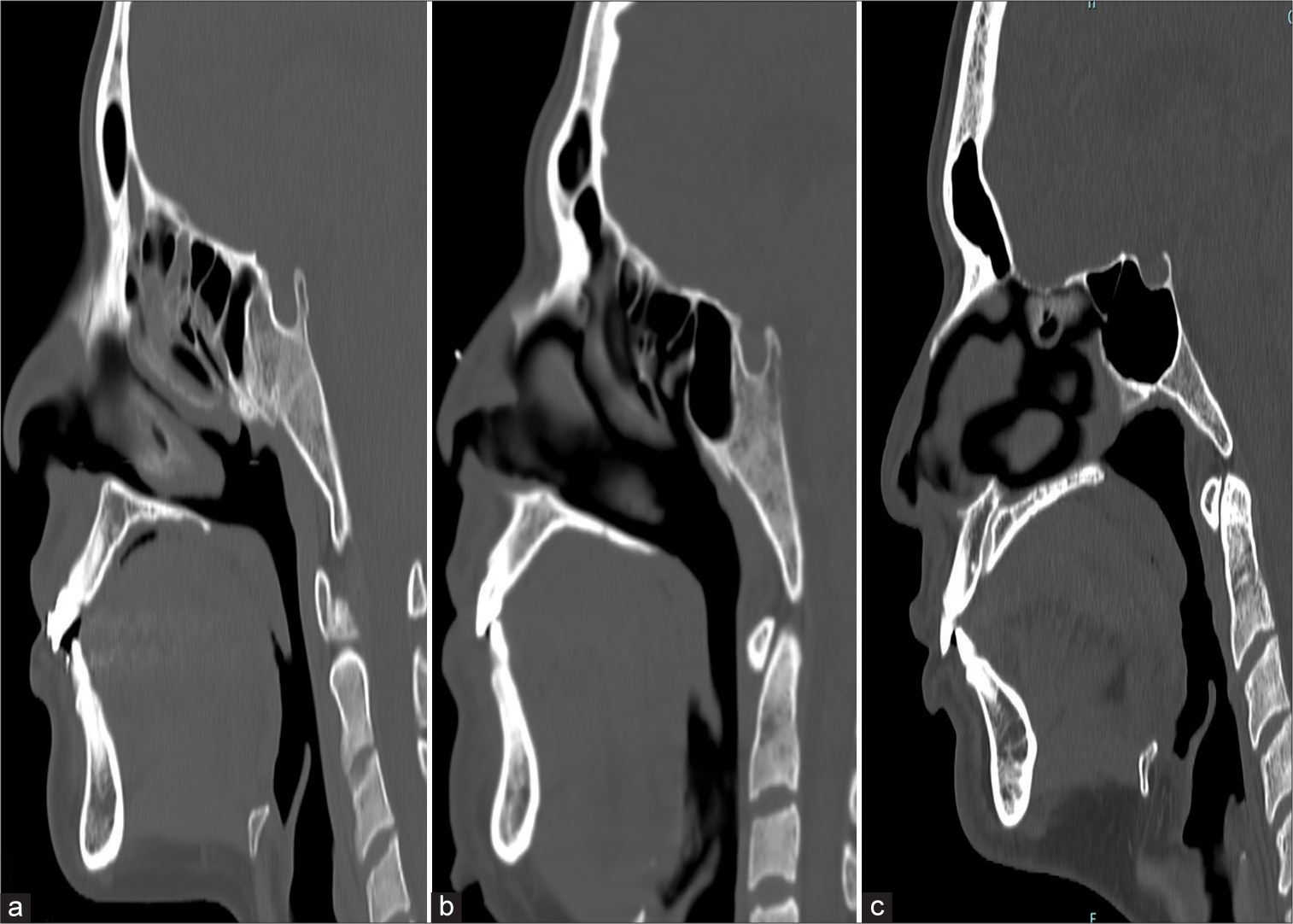
A meticulous morphometric analysis of the images was conducted, led by an experienced neurosurgeon and neuroradiologist. The main objective was to identify types of pneumatization of the sphenoid sinus, classifying them into conchal, complete sellar, and incomplete sellar [
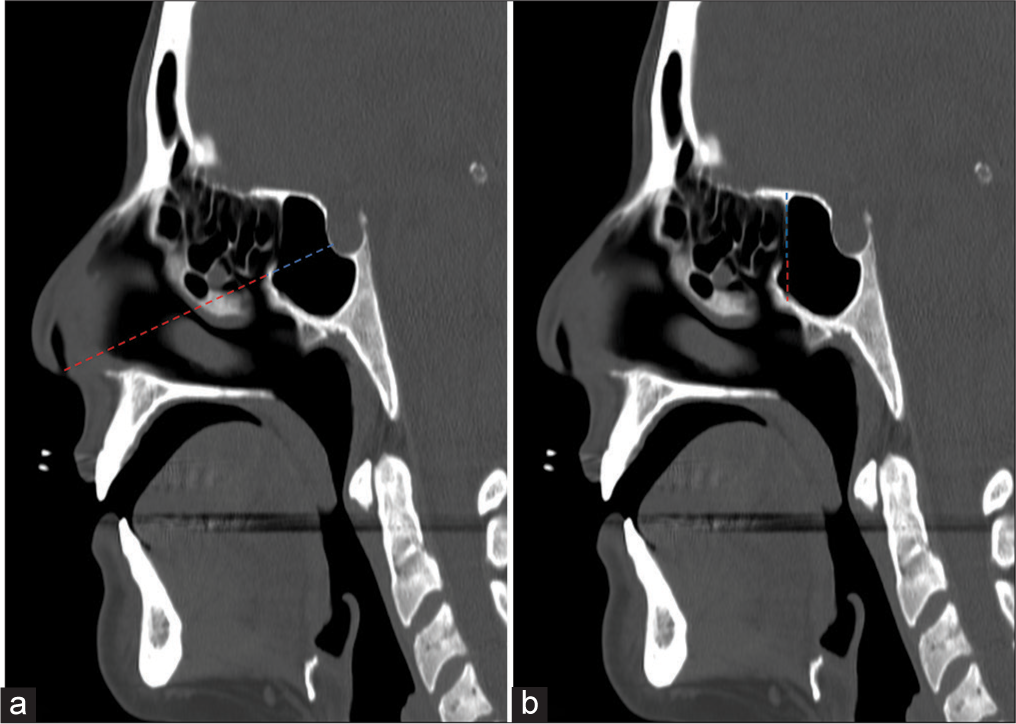
In addition, specific measurements of four key parameters to evaluate the anatomy of the craniofacial region were carried out. First, the distance from the nasal opening to the sphenoid sinus was measured. Second, the assessment of the distance between the anterior and posterior edges of the sphenoid sinus. Third, the distance from the anterior skull base to the sphenoidal ostium, the opening of the sphenoid sinus. Finally, the evaluation of the distance from the floor of the sphenoid sinus to the sphenoidal ostium [
Figure 2:
Measurements of the sphenoid sinus in the Peruvian population. (a) The dashed red line measured the distance from the nasal opening to the sphenoid sinus. The blue line measured the distance between the anterior and posterior borders of the sphenoid sinus. (b) The dashed blue line measures the distance from the anterior skull base to the sphenoid ostium, and the dashed red line measures the distance from the floor of the sphenoid sinus to the sphenoid ostium.
It is relevant to note that, in cases of conchal pneumatization, measurements from the skull base to the sphenoidal ostium and from the floor of the sphenoid sinus to the sphenoidal ostium were omitted, based on the fact that the conchal type does not have a sphenoidal ostium.
Statistical analysis
The collected information was transferred to a database and subjected to analysis using STATA software version 15. Initially, the frequency distribution of the selected variables in the sample was conducted. Subsequently, measurements of quantitative variables were represented in a normal distribution curve and tabulated, including the mean and standard deviation. To assess the statistical significance of the results, parametric statistical tests were applied. Independent samples t-test and analysis of variance test were used to compare means between two or more groups, respectively. In addition, the Kruskal–Wallis test was included to evaluate the significance of variables with non-normal distribution. A level of statistical significance was established at P ≤ 0.05, considering results meeting this criterion as significant.
RESULTS
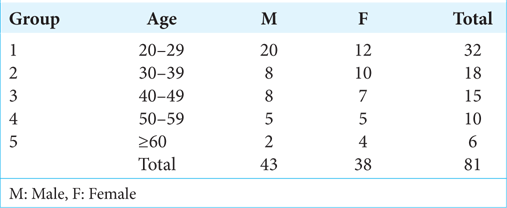
The results reveal that the majority of participants were in the age groups of 20–29 years and 30–39 years, with 32 and 18 participants, respectively. Gender distribution was balanced, with 43 male and 38 female participants totaling 81 participants [
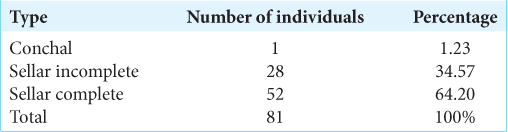
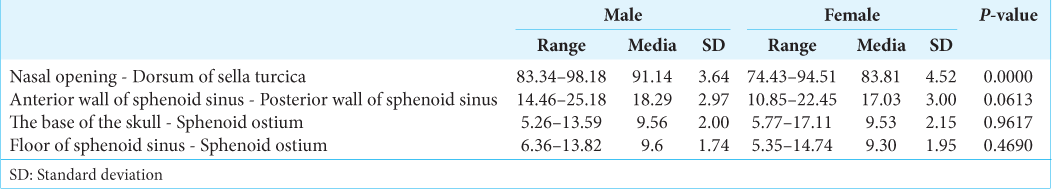
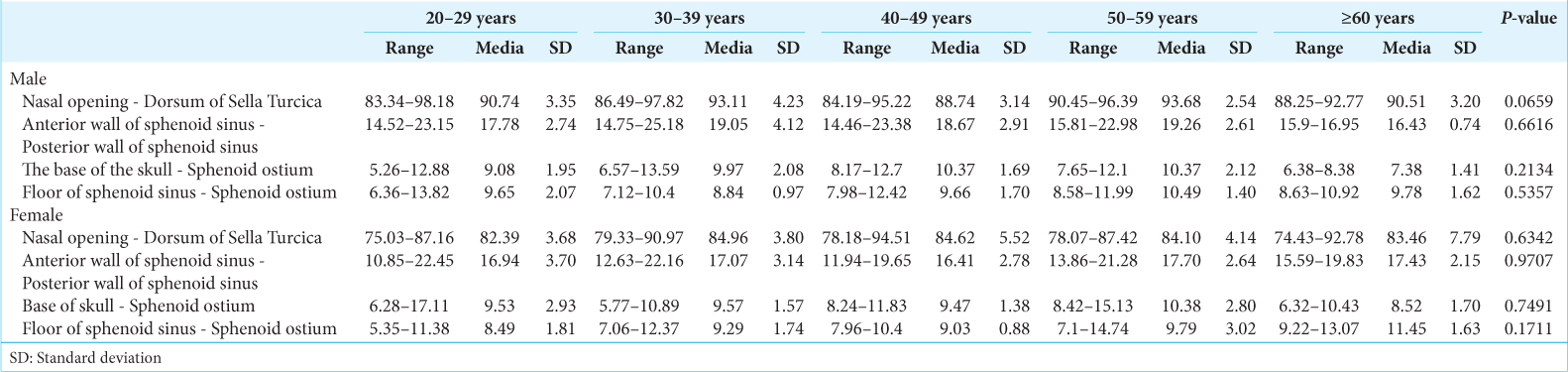
The results in
Regarding the distance between the anterior and posterior walls of the sphenoid sinus, no significant differences were observed between men (mean: 18.29 mm, SD: 2.97) and women (mean: 17.03 mm, SD: 3.00) (P = 0.0613). In addition, no significant differences were found in measurements from the base of the skull to the sphenoidal ostium and from the floor of the sphenoid sinus to the sphenoidal ostium between genders.
DISCUSSION
Morphometry plays an essential role in providing detailed quantitative information about the anatomy of a specific population. Previous Peruvian studies have been published on the morphometry of the foramen magnum [
Surgical planning not only customizes the intervention according to individual characteristics but also reduces risks and improves surgical outcomes by anticipating potential challenges in the operating room.[
The frequency of the open sphenoid ostium in Peruvian anatomy raises significant questions about the suitability of the transsphenoidal approach in surgeries for pituitary tumors. This anatomical finding suggests that the transsphenoidal approach could be a viable option due to the high accessibility of the sphenoid ostium in most Peruvians, facilitating access to the sellar region without the need for additional sinus opening procedures.[
Considering the distance and choosing the right instruments for a transsphenoidal approach is crucial for surgical planning.[
The frequent pneumatization of the sphenoid sinus in the Peruvian population is a crucial factor in surgical planning for transsphenoidal procedures. Sphenoid sinus pneumatization, characterized by air cavities, directly influences surgical strategies.[
The fact that most Peruvians have a fully pneumatized sphenoid sinus emphasizes that the transsphenoidal approach could be a feasible option for treating sellar region conditions. With this prevalent pneumatization pattern, this surgical method, known for being minimally invasive, appears effective and suitable for Peruvian patients.[
CONCLUSION
The morphometric analysis highlights that complete sellar pneumatization is the most common in the Peruvian population. This study holds significant relevance for transsphenoidal surgery in Peru as it provides detailed quantitative insights into the individual anatomy of the sella turcica and surrounding structures. Moreover, the variation in the distance from the nasal opening to the dorsum of the sella turcica between males and females underscores the role of morphometry in tailoring surgical approaches precisely, thereby mitigating risks and complications by adjusting strategies according to each patient’s unique anatomical characteristics.
Morphometry, akin to an artist’s precise brush strokes, enables surgeons to delineate interventions meticulously, considering individual anatomical nuances and guiding instrument selection with precision. This artistry not only enhances the customization of surgical procedures but also enhances overall procedural safety by anticipating anatomical variations that influence the efficacy of transsphenoidal surgery. Thus, the fusion of morphometric analysis with surgical expertise results in a tailored and personalized approach that enhances the quality and safety of transsphenoidal surgery, specifically within the Peruvian population.
Ethical approval
The research protocol underwent review and approval by the Medical Ethics Committee of Private Hospital Center. The approval number 05-012024-115 Date 17/01/2024.
Declaration of patient consent
Patient’s consent was not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Al-Dwairy S, Al-Mousa A, Fataftah J, Tarifi AA, Al-Ani SO, Badran KH. Morphometric analysis of the sella turcica and sphenoid sinus: A retrospective cross-sectional study. Int J Morphol. 2023. 41: 858-62
2. Azab WA, Abdelnabi EA, Mostafa KH, Burhamah TA, Alhaj AK, Khalil AM. Effect of sphenoid sinus pneumatization on the surgical windows for extended endoscopic endonasal transsphenoidal surgery. World Neurosurg. 2020. 133: e695-701
3. Buchfelder M, Schlaffer SM, Zhao Y. The optimal surgical techniques for pituitary tumors. Best Pract Res Clin Endocrinol Metab. 2019. 33: 101299
4. Cappabianca P, Cavallo LM, Esposito F, de Divitiis E. Endoscopic endonasal transsphenoidal surgery: Procedure, endoscopic equipment and instrumentation. Childs Nerv Syst. 2004. 20: 796-801
5. Chumnanvej S, Pillai BM, Chalongwongse S, Suthakorn J. Endonasal endoscopic transsphenoidal approach robot prototype: A cadaveric trial. Asian J Surg. 2021. 44: 345-51
6. Dogan ME, Kotanlı S, Yavuz Y, Wahjuningrum DA, Pawar AM. Computed tomography-based assessment of sphenoid sinus and sella turcica pneumatization analysis: A retrospective study. PeerJ. 2023. 11: e16623
7. ELKammash TH, Enaba MM, Awadalla AM. Variability in sphenoid sinus pneumatization and its impact upon reduction of complications following sellar region surgeries. Egypt J Radiol Nucl Med. 2014. 45: 705-14
8. Enkaoua A, Islam M, Ramalhinho J, Dowrick T, Booker J, Khan DZ. Image-guidance in endoscopic pituitary surgery: An in-silico study of errors involved in tracker-based techniques. Front Surg. 2023. 10: 1222859
9. Famurewa OC, Ibitoye BO, Ameye SA, Asaleye CM, Ayoola OO, Onigbinde OS. Sphenoid sinus pneumatization, septation, and the internal carotid artery: A computed tomography study. Niger Med J. 2018. 59: 7-13
10. Gandhi CD, Christiano LD, Eloy JA, Prestigiacomo CJ, Post KD. The historical evolution of transsphenoidal surgery: Facilitation by technological advances. Neurosurg Focus. 2009. 27: E8
11. García-Garrigós E, Arenas-Jiménez JJ, Monjas-Cánovas I, Abarca-Olivas J, Cortés-Vela JJ, De La Hoz-Rosa J. Transsphenoidal approach in endoscopic endonasal surgery for skull base lesions: What radiologists and surgeons need to know. RadioGraphics. 2015. 35: 1170-85
12. Hanson M, Li H, Geer E, Karimi S, Tabar V, Cohen MA. Perioperative management of endoscopic transsphenoidal pituitary surgery. World J Otorhinolaryngol Head Neck Surg. 2020. 6: 84-93
13. Iskra T, Stachera B, Możdżeń K, Murawska A, Ostrowski P, Bonczar M. Morphology of the sella turcica: A meta-analysis based on the results of 18,364 patients. Brain Sci. 2023. 13: 1208
14. Khan DZ, Hanrahan JG, Baldeweg SE, Dorward NL, Stoyanov D, Marcus HJ. Current and future advances in surgical therapy for pituitary adenoma. Endocr Rev. 2023. 44: 947-59
15. Van Lindert EJ, Ingels K, Mylanus E, Grotenhuis JA. Variations of endonasal anatomy: Relevance for the endoscopic endonasal transsphenoidal approach. Acta Neurochir (Wien). 2010. 152: 1015-20
16. Liu JK, Das K, Weiss MH, Laws ER, Couldwell WT. The history and evolution of transsphenoidal surgery. J Neurosurg. 2001. 95: 1083-96
17. Lobatto DJ, de Vries F, Zamanipoor Najafabadi AH, Pereira AM, Peul WC, Vliet Vlieland TP. Preoperative risk factors for postoperative complications in endoscopic pituitary surgery: A systematic review. Pituitary. 2018. 21: 84-97
18. Louis RG, Eisenberg A, Barkhoudarian G, Griffiths C, Kelly DF. Evolution of minimally invasive approaches to the sella and parasellar region. Int Arch Otorhinolaryngol. 2014. 18: S136-48
19. Luzzi S, Giotta Lucifero A, Rabski J, Kadri PA, Al-Mefty O. The party wall: Redefining the indications of transcranial approaches for giant pituitary adenomas in endoscopic era. Cancers. 2023. 15: 2235
20. Elhadi AM, Hardesty DA, Zaidi HA, Kalani MY, Nakaji P, White W. Evaluation of surgical freedom for microscopic and endoscopic transsphenoidal approaches to the sella. Neurosurgery. 2015. 11: 69-78 discussion 78-9
21. Maia R, Miranda A, Geraldo AF, Sampaio L, Ramaglia A, Tortora D. Neuroimaging of pediatric tumors of the sellar region-A review in light of the 2021 WHO classification of tumors of the central nervous system. Front Pediatr. 2023. 11: 1162654
22. Orringer DA, Golby A, Jolesz F. Neuronavigation in the surgical management of brain tumors: Current and future trends. Expert Rev Med Devices. 2012. 9: 491-500
23. Raappana A, Koivukangas J, Pirilä T. 3D modeling-based surgical planning in transsphenoidal pituitary surgery-preliminary results. Acta Otolaryngol (Stockh). 2008. 128: 1011-8
24. Raseman J, Guryildirim M, Beer-Furlan A, Jhaveri M, Tajudeen BA, Byrne RW. Preoperative computed tomography imaging of the sphenoid sinus: Striving towards safe transsphenoidal surgery. J Neurol Surg Part B Skull Base. 2020. 81: 251-62
25. Sari S, Sari E, Akgun V, Ozcan E, Ince S, Saldir M. Measures of pituitary gland and stalk: From neonate to adolescence. J Pediatr Endocrinol Metab. 2014. 27: 1071-6
26. Sevinc O, Is M, Barut C, Erdogan A. Anatomic variations of sphenoid sinus pneumatization in a sample of Turkish population: MRI study. Int J Morphol. 2014. 32: 1140-3
27. Shin JH, Kang SG, Hong YK, Jeun SS, Kim SW, Kim SW. Role of the superior turbinate when performing endoscopic endonasal transsphenoidal approach. Folia Morphol. 2014. 73: 73-8
28. Shinomiya A, Shindo A, Kawanishi M, Miyake K, Nakamura T, Matsubara S. Usefulness of the 3D virtual visualization surgical planning simulation and 3D model for endoscopic endonasal transsphenoidal surgery of pituitary adenoma: Technical report and review of literature. Interdiscip Neurosurg. 2018. 13: 13-9
29. Şimşek S, İşlek A. Pneumatization of the sphenoid sinus is the major factor determining the variations of adjacent vital structures. Egypt J Otolaryngol. 2024. 40: 2
30. Štoković N, Trkulja V, Dumić-Čule I, Čuković-Bagić I, Lauc T, Vukičević S. Sphenoid sinus types, dimensions and relationship with surrounding structures. Ann Anat. 2016. 203: 69-76
31. Venneri F, Brown LB, Cammelli F, Haut ER, Donaldson L, Ricciardi W, Sheridan S, Tartaglia R, editors. Safe surgery saves lives. Textbook of patient safety and clinical risk management. Cham: Springer International Publishing; 2021. p. 177-88
32. Wei LF, Zhang J, Chen HJ, Wang R. Value of anatomical landmarks in single-nostril endonasal transnasal-sphenoidal surgery. Exp Ther Med. 2013. 5: 1057-62
33. Yan JL, Chang CN, Chen PY. Endoscopic transsphenoidal surgery for resection of pituitary macroadenoma: A retrospective study. PLoS One. 2021. 16: e0255599
34. Yataco-Wilcas CA, Salazar-Ascurra A, Diaz-Llanes BE, Coasaca-Tito YS, Lengua-Vega LA, Salazar-Campos CE. Morphometric analysis of the foramen magnum in the Peruvian population. Surg Neurol Int. 2024. 15: 9
35. Zada G, Agarwalla PK, Mukundan S, Dunn I, Golby AJ, Laws E. The neurosurgical anatomy of the sphenoid sinus and sellar floor in endoscopic transsphenoidal surgery. J Neurosurg. 2011. 114: 1319-30
36. Zada G, Woodmansee WW, Iuliano S, Laws ER. Perioperative management of patients undergoing transsphenoidal pituitary surgery. Asian J Neurosurg. 2010. 5: 1-6
37. Zhan G, Guo S, Hu H, Liao J, Dang R, Yang Y. Expanded endoscopic endonasal transsphenoidal approach to determine morphological characteristics and clinical considerations of the cavernous sinus venous spaces. Sci Rep. 2022. 12: 16794