- Department of Neurosurgery Kyoto University Graduate School of Medicine, Kyoto, Japan
- Department of Otolaryngology-Head and Neck Surgery, Kyoto University Graduate School of Medicine, Kyoto, Japan
- Department of Diagnostic Pathology, Kyoto University Hospital, Kyoto, Japan
Correspondence Address:
Masahiro Tanji, Department of Neurosurgery, Kyoto University Graduate School of Medicine, Kyoto, Japan.
DOI:10.25259/SNI_246_2024
Copyright: © 2025 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Masahiro Tanji1, Noritaka Sano1, Jun Hashimoto1, Masahiro Kikuchi2, Mami Matsunaga2, Yuji Kitada2, Maki Yamamoba2, Yasuhide Takeuchi3, Yasuhide Makino2, Etsuko Yamamoto Hattori1, Yukinori Terada1, Yohei Mineharu1, Yoshiki Arakawa2. Multiport combined endoscopic endonasal and transorbital approach to orbital schwannoma. 21-Mar-2025;16:98
How to cite this URL: Masahiro Tanji1, Noritaka Sano1, Jun Hashimoto1, Masahiro Kikuchi2, Mami Matsunaga2, Yuji Kitada2, Maki Yamamoba2, Yasuhide Takeuchi3, Yasuhide Makino2, Etsuko Yamamoto Hattori1, Yukinori Terada1, Yohei Mineharu1, Yoshiki Arakawa2. Multiport combined endoscopic endonasal and transorbital approach to orbital schwannoma. 21-Mar-2025;16:98. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=13445
Abstract
BackgroundWe present a case report describing the use of combined endoscopic endonasal and transorbital approach (EETOA) for intraorbital schwannoma that grew rapidly during pregnancy.
Case DescriptionA 27-year-old woman who presented with headache was incidentally diagnosed with a tumor mass 1 cm in diameter near the right superior orbital fissure. Treatment of the tumor was deferred to follow-up. One month later, the patient became pregnant, and in the last trimester, she developed right abducens palsy and mildly dilated pupil. Magnetic resonance imaging (MRI) showed that the tumor mass had grown rapidly with a maximal diameter of 5 cm and had extended into the orbit through the superior orbital fissure. After spontaneous vaginal delivery, EETOA was planned to remove both the intraorbital region and cavernous sinus compartment to avoid craniotomy. Surgical resection began with an endoscopic endonasal approach. Orbital decompression was performed by removing the lamina papyracea, and the tumor was resected in the lateral cavernous sinus compartment. An eyebrow incision was made, and endoscopic transorbital surgery was performed to remove the intraorbital region. Multi-perspective views during EETOA enabled gross total resection of the tumor and confirmed by intraoperative MRI. The pathological diagnosis was schwannoma. The patient’s abducens nerve palsy improved after surgery.
ConclusionEETOA can offer maximal exposure and resection for tumors extending from the cavernous sinus to the orbit without craniotomy in selected cases.
Keywords: Combined endoscopic endonasal and transorbital approach, Multiport surgery, Pregnancy, Schwannoma
INTRODUCTION
The orbit is an anatomically complex area, and intraorbital tumors can be approached from different surgical corridors.[
The evolution of the endoscopic endonasal approach (EEA) has enabled the removal of tumors that would have required craniotomy in the past.[
In this report, we present a case of intraorbital schwannoma that grew rapidly during pregnancy. After spontaneous vaginal delivery, the multiport combined endoscopic endonasal and transorbital approach (EETOA) was successfully performed to remove the tumor completely, demonstrating that the combination of both corridors could provide safer extensive resection.
CASE PRESENTATION
History and examination
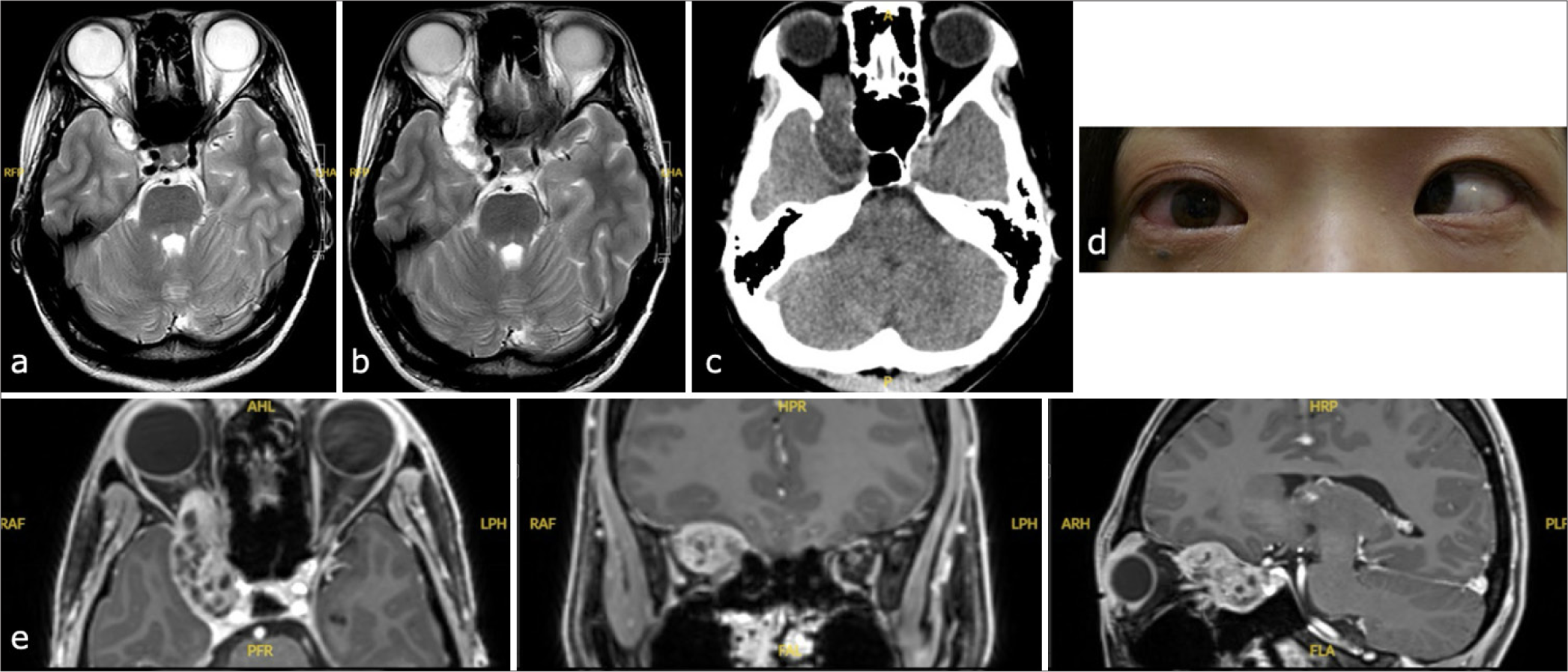
A 27-year-old Japanese woman presented with a headache was discovered incidentally to have a tumor mass 1 cm in diameter near the right superior orbital fissure [
Figure 1:
(a) Initial magnetic resonance T2-weighted imaging of the tumor. (b)The tumor grew rapidly during pregnancy and extended to the intraorbital area. (c) Head computed tomography showing the enlargement of superior orbital fissure. (d) At the last trimester, the patient developed right abducens palsy and a mildly dilated pupil. (e) Preoperative Gadolinium-enhanced T1 imaging of the tumor in axial, coronal, and sagittal views from left to right.
MRI showed that a contrast-enhanced mass with a clear boundary and diameter of 5 cm had extended into the right intraconal space of the orbit through the superior orbital fissure to displace the optic nerve, causing proptosis [
Based on the symptoms[
Combined EETOA
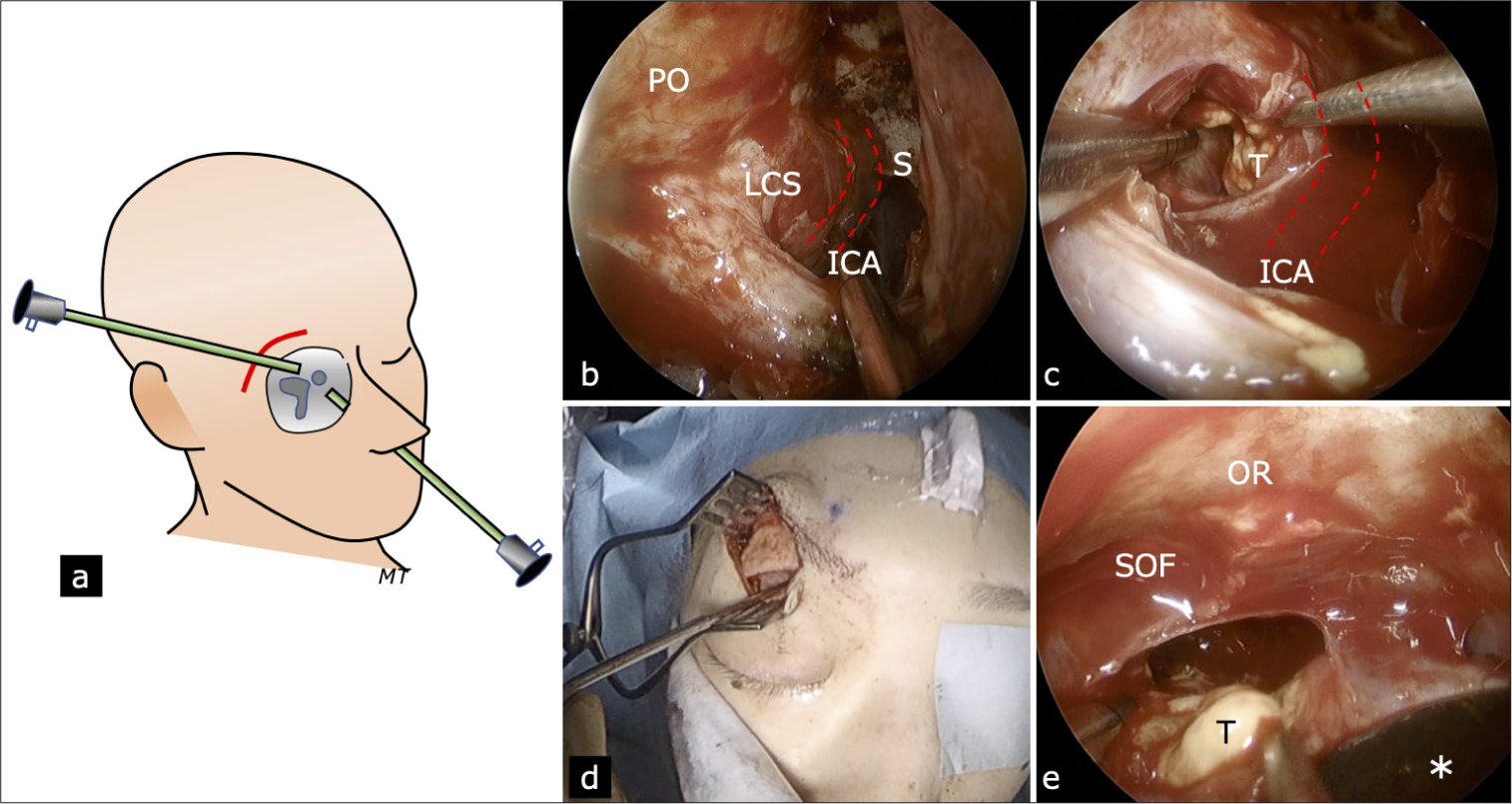
The operation involved a collaboration of neurosurgeons and otolaryngologists [
Figure 2:
(a) Schema of multiport combined endoscopic endonasal and transorbital approach via an eyebrow incision. (b) After exposing the periorbita and lateral compartment of the cavernous sinus, the internal carotid artery was identified by Doppler sonography and electromagnetic field guide navigation. (c) The lateral cavernous sinus compartment was incised, and the tumor was removed in a subcapsular fashion. (d) An eyebrow incision was made, and the superior orbital rim was exposed in a subperiosteal fashion. After the orbit was compressed downward with a spatula (*), the endoscope was introduced, and the tumor was removed piece by piece. (e) An enlarged superior orbital fissure was noted. ICA:Internal carotid artery; LCS :Lateral compartment of the cavernous sinus; OR :Optic roof; PO :Periorbita; S:Sella; SOF:Superior orbital fissure; T:Tumor.
Video 1
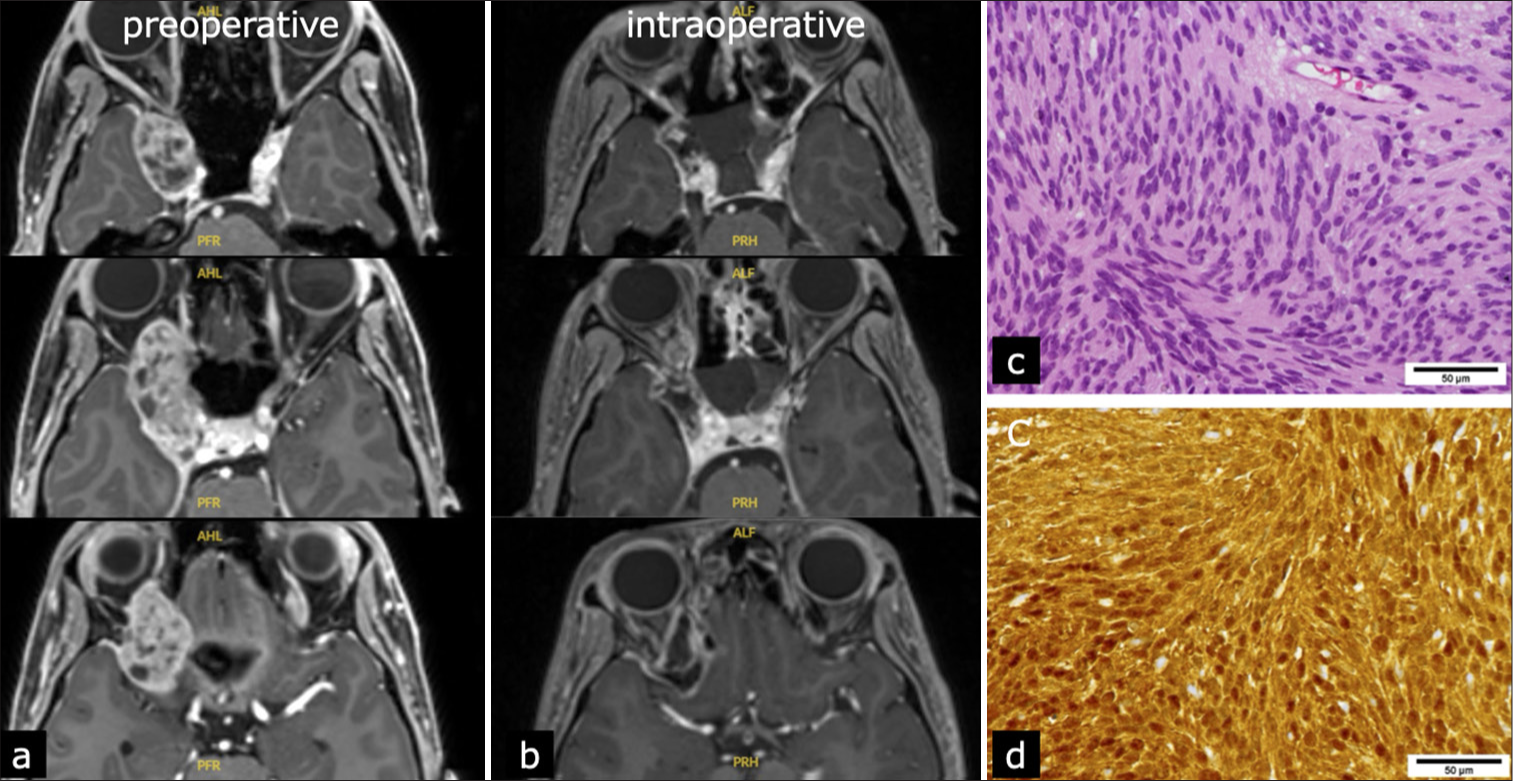
Pathological examination showed spindle-shaped cell tumors with hyaline small blood vessels [
Combining the intraoperative and pathological findings, the final diagnosis was trigeminal ophthalmic division schwannoma.
The patient recovered completely without any complications. She was discharged home 4 days postoperatively. At the 4-month follow-up, her abducens nerve palsy and proptosis had resolved completely. The mildly dilated pupil remained, possibly due to irreversible damage to the ciliary ganglion.
DISCUSSION
Since trigeminal schwannoma progresses to various sites and is anatomically complex, an understanding of surgical anatomy and selecting the appropriate approach are important considerations. Yoshida and Kawase[
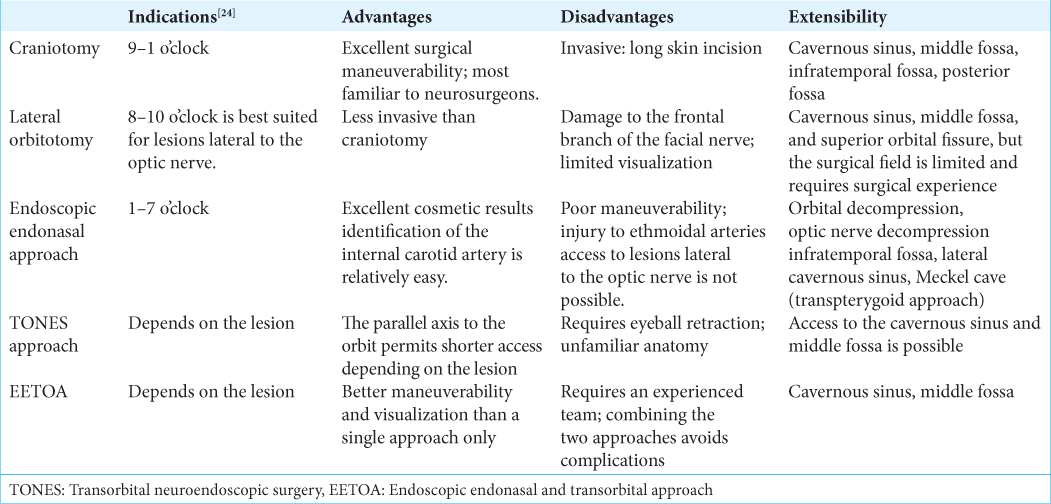
Approaches to intraorbital tumors are broadly divided into the transcranial, endonasal, and transorbital approaches [
The transcranial approach to the orbit[
Lateral orbitotomy involves opening the outer rim of the orbit and entering the posterior surface of the eye from the lateral side.[
Cases employing the endonasal approach to resect orbital tumors are increasing.[
The transorbital approach has undergone recent developments, and its indication has been extended by endoscopy.[
A multiport approach combining the endoscopic endonasal and endoscopic transorbital approaches has been recently reported. Ciporen et al.[
Our patient had a large lesion extending from the cavernous sinus to the orbit, which ostensibly indicated the transcranial approach. However, in the pursuit of a minimally invasive method and shorter hospitalization, we decided to employ endoscopy in combination with both the nasal and transorbital approaches. We inferred that the intraorbital region could not be removed through the endonasal approach alone. Furthermore, removal of the cavernous sinus region would probably be difficult through the transorbital approach alone. Furthermore, decompressing the orbit and managing the ICA would have been particularly difficult.
In the case of EETOA surgery, a part of the orbital paper-like plate was first separated into an elliptical shape through the nasal approach to provide mobility. Pressure on the eyeball during the transorbital operation was relieved, and sufficient working space was secured to perform the intraorbital operation more safely. Although abducens nerve monitoring was not performed in this case, a safer surgery could have been possibly performed if monitoring was performed at the time of incision. In addition, we considered the possibility of additionally performing supraorbital craniotomy if transorbital manipulation was insufficient and made the tumor difficult to resect. The eyebrow incision is more familiar to neurosurgeons[
CONCLUSION
This report demonstrated that EETOA was successfully performed in the resection of an intraorbital schwannoma. The findings highlight how surgeons may apply multiple corridors in successfully accessing and resecting complex skull base tumors.
Ethical approval
The research/study was approved by the Institutional Review Board at Kyoto University Hospital, number R2088, dated February 01, 2020.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Almeida JP, Omay SB, Shetty SR, Chen YN, Ruiz-Treviño AS, Liang B. Transorbital endoscopic eyelid approach for resection of sphenoorbital meningiomas with predominant hyperostosis: Report of 2 cases. J Neurosurg. 2018. 128: 1885-95
2. Alqahtani A, Padoan G, Segnini G, Lepera D, Fortunato S, Dallan I. Transorbital transnasal endoscopic combined approach to the anterior and middle skull base: A laboratory investigation. Acta Otorhinolaryngol Ital. 2015. 35: 173-9
3. Berhouma M, Jacquesson T, Abouaf L, Vighetto A, Jouanneau E. Endoscopic endonasal optic nerve and orbital apex decompression for nontraumatic optic neuropathy: Surgical nuances and review of the literature. Neurosurg Focus. 2014. 37: E19
4. Bhuskute GS, Gosal JS, Alsavaf MB, Abouammo MD, Manjila S, Kandregula S. Morphometric comparison of endoscopic endonasal transpterygoid and precaruncular contralateral medial transorbital approaches to sphenoid sinus lateral recess. Oper Neurosurg (Hagerstown). 2024. 27: 96-105
5. Bhuskute GS, Gosal JS, Alsavaf MB, Manjila S, Wu KC, Alwabili M. Endoscopic precaruncular medial transorbital and endonasal multiport approaches to the contralateral skull base: A clinicoanatomical study. Neurosurg Focus. 2024. 56: E10
6. Bounajem MT, Rennert RC, Budohoski KP, Azab M, Karsy M, Couldwell WT. Modified lateral orbitotomy approach to lesions of the orbital apex, superior orbital fissure, cavernous sinus, and middle cranial fossa. Oper Neurosurg (Hagerstown). 2023. 24: 514-23
7. Castelnuovo P, Dallan I, Locatelli D, Battaglia P, Farneti P, Tomazic PV. Endoscopic transnasal intraorbital surgery: our experience with 16 cases. Eur Arch Otorhinolaryngol. 2012. 269: 1929-35
8. Castelnuovo P, Turri-Zanoni M, Battaglia P, Locatelli D, Dallan I. Endoscopic endonasal management of orbital pathologies. Neurosurg Clin N Am. 2015. 26: 463-72
9. Cavallo LM, Solari D, Cappabianca P. Multiportal Approach to the skull base: One key, multiple gates. World Neurosurg. 2015. 84: 630-1
10. Chang BY, Moriarty P, Cunniffe G, Barnes C, Kennedy S. Accelerated growth of a primary orbital schwannoma during pregnancy. Eye (Lond). 2003. 17: 839-41
11. Ciporen JN, Moe KS, Ramanathan D, Lopez S, Ledesma E, Rostomily R. Multiportal endoscopic approaches to the central skull base: A cadaveric study. World Neurosurg. 2010. 73: 705-12
12. Cornelis MM, Lubbe DE. Pre-caruncular approach to the medial orbit and landmarks for anterior ethmoidal artery ligation: A cadaveric study. Clin Otolaryngol. 2016. 41: 777-81
13. Dallan I, Castelnuovo P, Locatelli D, Turri-Zanoni M, AlQahtani A, Battaglia P. Multiportal combined transorbital transnasal endoscopic approach for the management of selected skull base lesions: Preliminary experience. World Neurosurg. 2015. 84: 97-107
14. DI Somma A, Guizzardi G, Valls Cusiné C, Hoyos J, Ferres A, Topczewski TE. Combined endoscopic endonasal and transorbital approach to skull base tumors: A systematic literature review. J Neurosurg Sci. 2022. 66: 406-12
15. Dubal PM, Svider PF, Denis D, Folbe AJ, Eloy JA. Short-term outcomes of purely endoscopic endonasal resection of orbital tumors: A systematic review. Int Forum Allergy Rhinol. 2014. 4: 1008-15
16. Fukaya R, Yoshida K, Ohira T, Kawase T. Trigeminal schwannomas: Experience with 57 cases and a review of the literature. Neurosurg Rev. 2010. 34: 159-71
17. Goel A, Shah A, Muzumdar D, Nadkarni T, Chagla A. Trigeminal neurinomas with extracranial extension: Analysis of 28 surgically treated cases. J Neurosurg. 2010. 113: 1079-84
18. Guizzardi G, Prats-Galino A, Mosteiro A, Santos C, Topczewski T, Torales J. Multiportal combined endoscopic endonasal and transorbital pathways: Qualitative and quantitative anatomic studies of the “connection” skull base areas. Oper Neurosurg (Hagerstown). 2023. 24: e342-50
19. Hardesty DA, Montaser AS, Carrau RL, Prevedello DM. Limits of endoscopic endonasal transpterygoid approach to cavernous sinus and Meckel’s cave. J Neurosurg Sci. 2018. 62: 332-8
20. Hofstetter CP, Singh A, Anand VK, Kacker A, Schwartz TH. The endoscopic, endonasal, transmaxillary transpterygoid approach to the pterygopalatine fossa, infratemporal fossa, petrous apex, and the Meckel cave. J Neurosurg. 2010. 113: 967-74
21. Hötte GJ, Meijer N, Verdijk RM, Paridaens D. Accelerated growth of orbital schwannomas during pregnancy does not correlate with sex hormone-or growth factor receptor status. Orbit. 2021. 40: 120-6
22. Kikuchi M, Nakagawa T. Recent progress in endoscopic skull base surgery: Functional preservation and multiportal approaches. Auris Nasus Larynx. 2023. 50: 32-9
23. Kim KS, Jung JW, Yoon KC, Kwon YJ, Hwang JH, Lee SY. Schwannoma of the orbit. Arch Craniofac Surg. 2015. 16: 67-72
24. Lee RP, Khalafallah AM, Gami A, Mukherjee D. The lateral orbitotomy approach for intraorbital lesions. J Neurol Surg B Skull Base. 2020. 81: 435-41
25. Lee WJ, Hong SD, Woo KI, Seol HJ, Choi JW, Lee JI. Combined endoscopic endonasal and transorbital multiportal approach for complex skull base lesions involving multiple compartments. Acta Neurochir (Wien). 2022. 164: 1911-22
26. Li P, Wang Z, Zhou Q, Li S, Zhang J, Wang Y. A Retrospective analysis of vision-impairing tumors among 467 patients with neurofibromatosis type 2. World Neurosurg. 2017. 97: 557-64
27. Moe KS. The precaruncular approach to the medial orbit. Arch Facial Plast Surg. 2003. 5: 483-7
28. Paluzzi A, Gardner Pa, Fernandez-Miranda JC, Tormenti MJ, Stefko ST, Snyderman CH. “Round-the-clock” surgical access to the orbit. J Neurol Surg B Skull Base. 2015. 76: 12-24
29. Park HH, Hong SD, Kim YH, Hong CK, Woo KI, Yun IS. Endoscopic transorbital and endonasal approach for trigeminal schwannomas: A retrospective multicenter analysis (KOSEN-005). J Neurosurg. 2020. 133: 467-76
30. Polster SP, Beale O, Patel VA, Abou-Al-Shaar H, Stefko ST, Gardner PA. The transcaruncular corridor of the medial transorbital approach to the frontal lobe: Technical nuances and applications. Oper Neurosurg (Hagerstown). 2023. 24: e458-62
31. Rootman J, Goldberg C, Robertson W. Primary orbital schwannomas. Br J Ophthalmol. 1982. 66: 194-204
32. Salgado-López L, Campos-Leonel LC, Pinheiro-Neto CD, Peris-Celda M. Orbital anatomy: Anatomical relationships of surrounding structures. J Neurol Surg B Skull Base. 2020. 81: 333-47
33. Salgado-Lopez L, Leonel LCPC, O’brien M, Adepoju A, Graffeo CS, Carlstrom LP. Anatomical step-by-step dissection of complex skull base approaches for trainees: Endoscopic endonasal approach to the orbit. J Neurol Surg B Skull Base. 2022. 84: 79-88
34. Shah KJ, Chamoun RB. Large vestibular schwannomas presenting during pregnancy: Management strategies. J Neurol Surg B Skull Base. 2014. 75: 214-20
35. Sugo N, Yokota K, Nemoto M, Hatori T, Kano T, Goto S. Accelerated growth of an orbital schwannoma during pregnancy. J Neuroophthalmol. 2007. 27: 45-7
36. Tanji M, Ogunbameru I, Garni Barkhoudarian DF, Cappabianca P, Cavallo L, de Divitiis O, Esposito F, editors. Supraorbital approach. Midline skull base surgery. Cham: Springer; 2016. p. 137-53
37. Tham T, Costantino P, Bruni M, Langer D, Boockvar J, Singh P. Multiportal combined transorbital and transnasal endoscopic resection of fibrous dysplasia. J Neurol Surg Rep. 2015. 76: e291-6
38. Ulutas M, Boyacı S, Akakın A, Kılıç T, Aksoy K. Surgical anatomy of the cavernous sinus, superior orbital fissure, and orbital apex via a lateral orbitotomy approach: A cadaveric anatomical study. Acta Neurochir (Wien). 2016. 158: 2135-48
39. Yamashita J, Asato R, Handa H, Nakao S, Ogata M. Abducens nerve palsy as initial symptom of trigeminal schwannoma. J Neurol Neurosurg Psychiatry. 1977. 40: 1190-7
40. Yoshida K, Kawase T. Trigeminal neurinomas extending into multiple fossae: Surgical methods and review of the literature. J Neurosurg. 1999. 91: 202-11