- Department of Surgery, Hawler Medical University, College of Medicine, Erbil, Iraq
Correspondence Address:
Injam Ibrahim Sulaiman, Department of Surgery, Hawler Medical University, College of Medicine, Erbil, Iraq.
DOI:10.25259/SNI_551_2024
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Injam Ibrahim Sulaiman. Neuroanatomical refinement of Kocher’s point for enhanced precision in ventriculostomy: A technical note and a literature review. 09-Aug-2024;15:274
How to cite this URL: Injam Ibrahim Sulaiman. Neuroanatomical refinement of Kocher’s point for enhanced precision in ventriculostomy: A technical note and a literature review. 09-Aug-2024;15:274. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=13036
Abstract
Background: This study was designed to assess the effectiveness and safety of using a modified Kocher’s point for ventriculostomy using endoscopic third ventriculostomy (ETV) and external ventricular drainage (EVD) in 200 patients at PAR Private Hospital in Erbil, Iraqi Kurdistan.
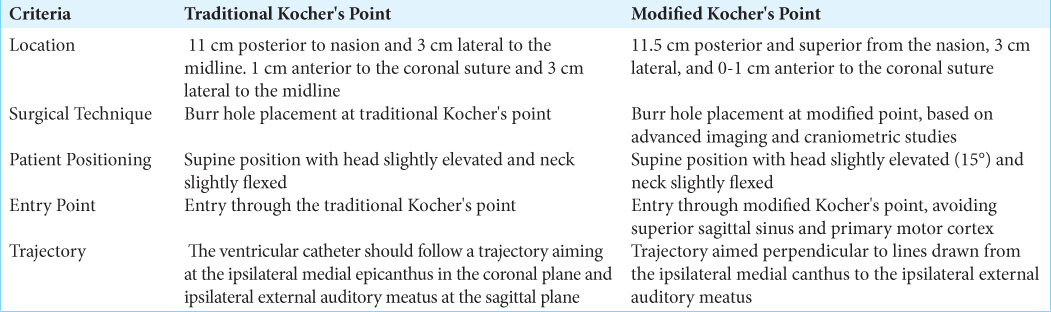
Methods: In this retrospective analysis, a total of 200 patients who were diagnosed with obstructive hydrocephalus and underwent ETV and EVD utilizing a modified entry site were included. The revised Kocher point was located 11.5 cm posterior and superior to the nasion, 3 cm laterally, and 0–1 cm before the coronal suture.
Results: The use of this modified Kocher’s point has brought much improvement in surgical precision and safety. This would minimize incidences of bleeding and misplacement of the catheters. The anatomical structure was well organized, and nothing was challenging in the process of traversing through the foramen of Monro into the third ventricle. It was easily introduced through the modified Kocher point with increasing efficacy and near zero possibility of sustaining injury to the limiting cerebral region.
Conclusion: Using the modified point of Kocher provides added reliability and accuracy to ventriculostomy, thereby reducing complications and increasing the overall outcome of surgeries. It overcomes all the drawbacks of classical entry sites and, further, helps in increasing the productivity of ETV and EVD. More research must be done to support the benefits of this modification in other clinical settings.
Keywords: Craniometrics, Endoscopic third ventriculostomy, External ventricular drainage, Kocher point, Neuroanatomy, Surgical precision
INTRODUCTION
The ventriculostomy is a surgical opening into a cerebral ventricle for drainage of cerebrospinal fluid (CSF). It has been the most life-saving measure in managing hydrocephalus and elevated intracranial pressure (ICP). This procedure can be life-saving, providing immediate relief in conditions such as traumatic brain injury, subarachnoid hemorrhage, and other causes of acute hydrocephalus.[
Endoscopic third ventriculostomy (ETV) is a well-established procedure for treating obstructive hydrocephalus, providing an effective alternative to ventriculoperitoneal shunting by creating a bypass for CSF flow through the floor of the third ventricle.[
In this paper, we propose a modification of the traditional Kocher point based on our experience in PAR private hospital in Erbil, Iraq, since 2014. We anticipate that this modification will give an exact entry point for both EVD and ETV and, therefore, help bring better surgical outcomes with reduced complications. We believe that as we share our technique, so shall we continue optimizing the ventriculostomy procedure.
MATERIALS AND METHODS
This study was conducted at PAR Private Hospital in Erbil, Iraq, and included 200 patients who underwent ETV and EVD from 2014 to May 2024. The patients were selected based on their diagnosis of obstructive hydrocephalus, with careful consideration of their ventricular anatomy and surrounding structures to ensure the feasibility of the procedure.
Preoperative planning
Preoperative magnetic resonance imaging scans were meticulously examined, both T1-weighted and T2-weighted, to plan the optimum trajectory of the endoscope. Attention was paid in detail to anatomic variants such as enlarged massa intermedia and tumors that may distort the ventricles or obscure normal anatomy. Basilar artery positioning relative to the dorsum sella was evaluated to avoid potential complications during the procedure.
Surgical procedure
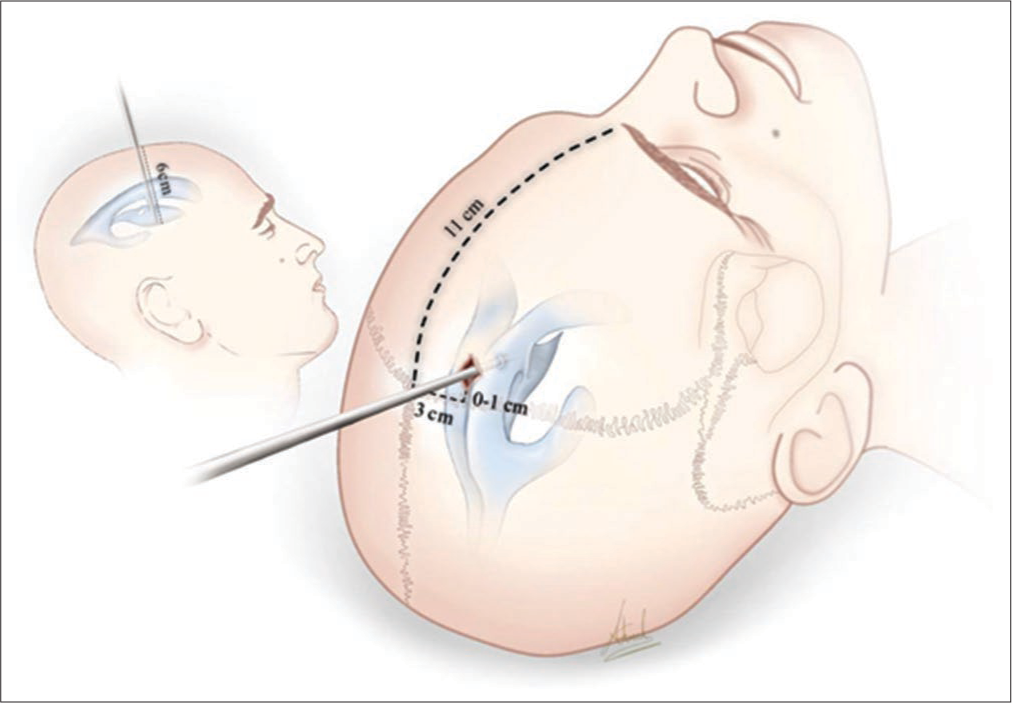
Patients were placed in a supine position with the head slightly elevated (15°) and the neck slightly flexed. The head was kept in a neutral position, aligned with the operating surgeon’s elbow level for ergonomic ease. The operating room was arranged with the patient’s head positioned 180° away from the anesthesia team, and the screens displaying neuronavigation and endoscope views were placed within the natural sight line of the surgical team. The patient’s head was registered to the neuronavigation system. The modified entry point was marked 11.5 cm posterior and superior from the nasion to the coronal suture, 3 cm lateral (preferably to the right), and 0–1 cm anterior to the coronal suture. A linear or curved incision was made based on the planned trajectory to optimize access to the floor of the third ventricle. A high-speed drill was used to create a burr hole at the marked entry point. The dura was coagulated and opened in a cruciate fashion. The pia was also coagulated and opened to allow the insertion of a peel-away sheath into the ventricle with the aid of neuronavigation. The endoscope was inserted through the peel-away sheath into the lateral ventricle. The choroid plexus and thalamostriate veins were identified to confirm correct ventricular entry. The endoscope was then advanced through the foramen of Monro to visualize the third ventricle. The floor of the third ventricle was punctured just anterior to the mammillary bodies using a stylet or endoscopic grasping forceps. The stoma was then enlarged using a Fogarty balloon catheter or spread with grasping forceps. It was crucial to confirm entry into the prepontine cistern by visualizing the basilar artery. The endoscope was withdrawn after ensuring the stoma was pulsating and free of obstructions. Minor bleeding was managed with gentle irrigation. The peel-away sheath was removed along with the endoscope, and an absorbable gelatin sponge was placed over the cortical defect to prevent CSF leakage. A burr hole cover was considered if necessary.
The surgical steps for placing an EVD using the modified Kocher’s point begin with positioning the patient in the supine position. The head must be elevated at 15° and slightly flexed at the neck. After marking the new entry point, incision is made in a straight or curvilinear manner. The marked entry point is drilled to make a burr hole using a high-speed drill and to coagulate the dura and cross-open, followed by coating and opening of the pia. Subsequently, the EVD catheter is placed through neuronavigation along a line from the ipsilateral medial canthus to the ipsilateral external auditory meatus on a perpendicular trajectory, then advanced about 6 cm or to the tip of the frontal horn of the ipsilateral lateral ventricle. The catheter is tunneled under the galea and attached to the externally attached drainage system with staples to the exterior to ensure fall-proof placement close to the foramen of Monro to maximize the removal of CSF [
Figure 1:
A 47-year-old male who works as an office manager presented to the emergency department with severe headache, nausea, and vomiting that began suddenly approximately 6 h before arrival. He describes the headache as diffuse, 10/10 in intensity, and not relieved by over-the-counter analgesia. He denies any recent trauma, loss of consciousness, or seizure activity. He has uncontrolled hypertension, and he is a heavy smoker. Physical examination revealed blood pressure 170/110 mmHg, heart rate 98 bpm, respiratory rate 18/min, and temperature 36.8°. Computed tomography (CT) scan reveals significant dilation of the lateral ventricles, consistent with hydrocephalus, and hyperdense areas within the ventricular system, indicating intraventricular hemorrhage. No significant midline shift or acute ischemic changes were noted. The patient was monitored in the intensive care unit with serial neurological assessments and imaging. A surgical plan to insert external ventricular drainage using a modified Kocher’s point was conducted. The outcome was good, with no intraoperative complications. (a) Preoperative CT planning for modified Kocher’s point. (b) Surgical positioning and burr hole placement for modified Kocher’s point. (c) Intraoperative view of the inserted drain. (d) Intraoperative view of modified Kocher’s point access.
Postoperative care
The patients were monitored for complications such as seizures, blood pressure lability, bradycardia, hyperthermia, and diabetes insipidus in the postoperative period. Furthermore, antibiotics were given for 24 h: high-dose dexamethasone and antiseizure medications if necessary. Patients were usually discharged within 1–2 days without complications.
RESULTS
In this study, we evaluated the modified Kocher point for ventriculostomy in 200 patients at PAR Private Hospital in Erbil, Iraq, from 2014 to 2023. The modified entry point was positioned 11.5 cm posterior and superior from the nasion to reach the coronal suture, then moving 3 cm laterally, preferably to the right, and 0–1 cm anterior to the coronal suture. The working point of entry for the modified Kocher point was based on a burr hole placed 11 cm superior and posterior from the nasion and 3 cm lateral to the midline. This location generally lay along the mid pupillary line and was lateral to the superior sagittal sinus and anterior to the primary motor cortex, two critical areas to avoid. The ventricular catheter was aimed at an angle perpendicular to the intersection of lines drawn from the ipsilateral medial canthus and the ipsilateral external auditory meatus and passed to a depth of approximately 6 cm or until the frontal horn of the ipsilateral lateral ventricle was reached. The optimal catheter placement aimed for the tip to be near the foramen of Monro to maximize CSF drainage.
There was considerable improvement in surgical precision for modifying entry points in 200 patients. Angle and depth measurements give more reliable trajectories to finesse access to the floor of the third ventricle, which did not require changes during surgery. Less hemorrhage and inaccurate catheter placement lead to better overall procedural success. The modified approach also proved advantageous in avoiding critical areas such as the superior sagittal sinus and the primary motor cortex. This precision in targeting significantly reduced postoperative complications, including seizures and infections, contributing to shorter hospital stays and faster recovery times. In addition, the technique facilitated easier management of patients with complex anatomical variations, such as an enlarged massa intermedia or distorted ventricles due to tumors.
DISCUSSION
The modified Kocher point presented in this article has brought considerable improvement in surgical accuracy and safety concerning the classic Kocher point and all other ventricular access points. By placing an entry point 11.5 cm posterior and superior from the nasion, 3 cm laterally, and 0–1 anteriorly concerning the coronal suture, we managed to increase the accuracy of ETVs and EVDs. This modification was based on our experience with 200 patients at PAR Private Hospital, Erbil, Iraq, from 2014 to May 2024. EVD is a critical procedure for managing acute hydrocephalus and elevated ICP. The traditional technique involves placing a burr hole at Kocher’s point, approximately 2 cm lateral to the midline and 2 cm anterior to the coronal suture. However, discrepancies between surface bony anatomy and internal cranial structures can result in suboptimal placement, increasing the risk of complications such as hemorrhage and inaccurate catheter placement.[
Advanced imaging techniques, together with craniometric studies, call for rethinking of already established entry points in EVD and ETV. Indeed, the accuracy needed to avoid complications in ETV seems all but achievable to the challenges evident in the placement of an EVD. It is through the acquisition, learning, and assimilation of such factors as from the management of the former, like continuous versus intermittent drainage that the modified Kocher point technique becomes a better chance to guarantee the precision and safety of both.
Advantages of the modified Kocher point
Our results showed that the modified entry point reduces the risk of complications such as hemorrhage and inaccurate catheter placement, which are commonly associated with the traditional Kocher point.[
Neuroanatomical pathway of the modified Kocher point
The advanced Kocher point makes the ventriculostomy more individualized by producing an entrance that is more precise and safer. It is generally 11 cm superior and posterior to the nasion and 3 cm lateral to the midline. This places the incision along the mid-pupillary line and anterior to the coronal suture [
This better orients the burr hole about essential internal anatomic landmarks. In its travel, the surgical probe passes through the frontal lobe, avoiding the superior sagittal sinus and the primary motor cortex to minimize the risk of hemorrhage and also to prevent functional devastation. The surgical probe proceeds to pass through the foramen of Monro, an important inside landmark between the lateral ventricles and the third ventricle. From the foramen of Monro, the probe is directed toward the floor of the third ventricle, specifically targeting the thin region anterior to the mammillary bodies and posterior to the infundibular recess.
Less distortion in adjacent brain parenchyma with this exact alignment will make it a safer means with improved effectiveness in entering the third ventricle. With the neuroanatomical route being so enhanced, apart from this, one can accurately place a stoma using the modified Kocher point, which will dramatically decrease the morbidity in terms of complications, for example, bleeding and catheter malpositioning, when compared to the traditional Kocher point. This improved pathway provides a safer and more reliable approach to ETV and EVD than traditional techniques, ensuring improved overall surgical outcomes.
Anatomical perspectives of other ventricular entry points
Although there are various other ventriculostomy entry points for EVD or shunt, compared to Kaufman’s, Paine’s, and Menovsky’s points, the modified Kocher point has several advantages. For example, Kaufman’s point is located 5 cm superior to the nasion and 3 cm lateral to the midline. Still, currently, it is rarely used due to its poor cosmetic results and lower success rates.[
Our approach aligns well with the key principles of minimizing invasiveness and maximizing the effectiveness of the procedure.[
Limitations
Although the cannulation of the ventricles through Kocher’s point is highly popular and widely practiced, accuracy remains relatively low. Miss rates were as wide as 4–40%.[
CONCLUSION
The modified Kocher point for both ETV and EVD offers a secure and precise site of entry. Based on the experiences of our 200 patients, it has been established that this strategy effectively reduces problems and enhances the outcomes of the treatments. Subsequent research should investigate the enduring advantages and potential applications of this change in various clinical contexts.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent was not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
Acknowledgment
We would like to present our gratitude to Doctor Ahmed Muthana for providing the medical illustration that has been used in this paper.
References
1. Abdoh MG, Bekaert O, Hodel J, Diarra SM, Le Guerinel C, Nseir R. Accuracy of external ventricular drainage catheter placement. Acta Neurochir (Wien). 2012. 154: 153-9
2. Abongha GB, Afunui NM, Elvira NA, Ezie KN, Kyaruzi VM, Lv X, Wu Y, Liang S, editors. Ventriculostomy. Frontiers in Hydrocephalus. IntechOpen; 2023. p.
3. Aref MH, Martyniuk A, Nath S, Koziarz A, Badhiwala J, Algird A. Endoscopic third ventriculostomy: Outcome analysis of an anterior entry point. World Neurosurg. 2017. 104: 554-9
4. Bertuccio A, Marasco S, Longhitano Y, Romenskaya T, Elia A, Mezzini G. External ventricular drainage: A practical guide for neuro-anesthesiologists. Clin Pract. 2023. 13: 219-29
5. Chau CY, Craven CL, Rubiano AM, Adams H, Tülü S, Czosnyka M. The evolution of the role of external ventricular drainage in traumatic brain injury. J Clin Med. 2019. 8: 1422
6. Chen CC, Freeman D, Warnke P. Frame-based stereotacticendoscopic third ventriculostomy-towards improved precision and minimizing morbidities. World Neurosurg. 2020. 140: e240-6
7. Chen F, Nakaji P. Optimal entry point and trajectory for endoscopic third ventriculostomy: Evaluation of 53 patients with volumetric imaging guidance. J Neurosurg. 2012. 116: 1153-7
8. Chung DY, Mayer SA, Rordorf GA. External ventricular drains after subarachnoid hemorrhage: Is less more?. Neurocrit Care. 2018. 28: 157-61
9. Decq P, Le Guerinel C, Palfi S, Djindjian M, Kéravel Y, Nguyen J. A new device for endoscopic third ventriculostomy. J Neurosurg. 2000. 93: 509-12
10. Dezena RA, editors. Surgical technique of endoscopic third ventriculostomy (ETV). Endoscopic third ventriculostomy. Cham: Springer; 2019. p.
11. Ge X, Xu X, Yu X, Chen X, Li D, Xu Y. Smartphone-assisted endoscopic surgery via Kocher’s point for intraventricular hemorrhage caused by thalamic hemorrhage: A comparison with external ventricular drainage. Exp Ther Med. 2019. 18: 1870-6
12. Hyun SJ, Suk JS, Kwon JT, Kim YB. Novel entry point for intraoperative ventricular puncture during the transsylvian approach. Acta Neurochir (Wien). 2007. 149: 1049-51 discussion 1051
13. Kaufmann GE, Clark K. Emergency frontal twist drill ventriculostomy. J Neurosurg. 1970. 33: 226-7
14. Menovsky T, De Vries J, Wurzer JA, Grotenhuis JA. Intraoperative ventricular puncture during supraorbital craniotomy via an eyebrow incision. J Neurosurg. 2006. 105: 485-6
15. Paine JT, Batjer HH, Samson D. Intraoperative ventricular puncture. Neurosurgery. 1988. 22: 1107-9
16. Park B, Han S, Byoun H, Han SB, Choi SW, Lim J. The assessment of geometric reliability of conventional trajectory of ventriculostomy in a three dimensional virtual model and proposal of a new trajectory. Neurol Med Chir. 2020. 60: 264-70
17. Park YG, Woo H, Kim E, Park J. Accuracy and safety of bedside external ventricular drain placement at two different cranial sites: Kocher’s point versus forehead. J Korean Neurosurg Soc. 2011. 50: 317-21
18. Raouf A, Zidan I. Endoscopic removal of third ventricular colloid cyst: Experience of 90 cases. Neurosurg Q. 2015. 25: 46-50
19. Rehman T, Rehman A, Ali R, Rehman A, Bashir H, Bhimani SA. A radiographic analysis of ventricular trajectories. World Neurosurg. 2013. 80: 173-8
20. Sahana D, Rathore L, Kumar S, Sahu R. Endoscopic anatomy of lateral and third ventricles: A must know for performing endoscopic third ventriculostomy. Neurol India. 2021. 69: 45-8
21. Techataweewan N, Dudzik B, Kitkhuandee A, Duangthongphon P, Tayles N. Gender and population variation in craniometry and Freehand pass ventriculostomy. World Neurosurg. 2018. 117: e194-203