- Department of Intensive Care, State University of Ponta Grossa, Brazil.
- Department of Neurological Surgery, State University of Ponta Grossa, Brazil.
- Department of Medical Student, State University of Ponta Grossa, Brazil.
- Department of Brain Care, University of Taubaté, Brazil.
- Department of Medical Student, University of Taubaté, Brazil.
- Department of Neurosurgery, University of São Paulo, São Paulo, Brazil.
Correspondence Address:
Leonardo C. Welling, Department of Neurological Surgery, State University of Ponta Grossa, Ponta Grossa, Parana, Brazil.
DOI:10.25259/SNI_124_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Thomas Markus Dhaese1, Leonardo C. Welling2, Alice Magro Koscianski3, Gustavo Frigeri4, Judy Auada5, Nícollas Nunes Rabelo6, Eberval Gadelha Figueiredo6. Non-invasive intracranial pressure monitoring in idiopathic intracranial hypertension and lumbar puncture in pediatric patient: Case report. Surg Neurol Int 30-Sep-2021;12:493
How to cite this URL: Thomas Markus Dhaese1, Leonardo C. Welling2, Alice Magro Koscianski3, Gustavo Frigeri4, Judy Auada5, Nícollas Nunes Rabelo6, Eberval Gadelha Figueiredo6. Non-invasive intracranial pressure monitoring in idiopathic intracranial hypertension and lumbar puncture in pediatric patient: Case report. Surg Neurol Int 30-Sep-2021;12:493. Available from: https://surgicalneurologyint.com/surgicalint-articles/non-invasive-intracranial-pressure-monitoring-in-idiopathic-intracranial-hypertension-and-lumbar-puncture-in-pediatric-patient-case-report/
Abstract
Background: Intracranial pressure (ICP) monitoring has been variously explored as a diagnostic and therapeutic modality in many pathological conditions leading neurological injury. This monitoring standardly depends on an invasive procedure such as cranial or lumbar catheterization. The gold standard for ICP monitoring is through an intraventricular catheter, but this invasive technique is associated with certain risks such as haemorrhage and infection. (1) Also, it is a high-cost procedure and consequently not available in a variety of underprivileged places and clinical situations in which intracranial hypertension is prevalent (3). An accurate non-invasive and low-priced method to measure elevated ICP would therefore be desirable. Under these circumstances, Brazilian scientists developed a non-invasive method for intracranial pressure monitoring (ICP-NI), which uses an electric resistance extensometer that measures micro deformations of the skull and transforms it into an electrical signal. In this case report, the authors describe a pediatrician patient with the diagnosis of idiopathic intracranial hypertension who was successfully submitted to a lumbar puncture under monitorization with this device.
Case description: 7 year old girl with progressive symptoms that lead to the diagnosis of idiopathic intracranial hypertension. The patient was submitted to a lumbar punction with continuous non-invasive ICP monitoring.
Conclusion: Estimating ICP (non-invasive) from LP monitoring (invasive) often reflect inaccurate ICP results, and affects negatively on IIH diagnosis and a non-invasive diagnostic method could reduce the requirement for invasive approaches, improving patient health outcomes.
Keywords: Idiopathic intracranial hypertension, Intracranial pressure monitoring, Intracranial pressure, Lumbar puncture
INTRODUCTION
Intracranial pressure (ICP) is defined as the pressure inside the skull, and therefore, the pressure inside the brain tissue and the cerebrospinal fluid (CSF). The relationship between CSF and intracranial blood volumes is described by the Monroe Kellie doctrine; because the brain is incompressible when the skull is intact, the sum of the volumes of the brain, CSF, and intracranial blood is constant.[
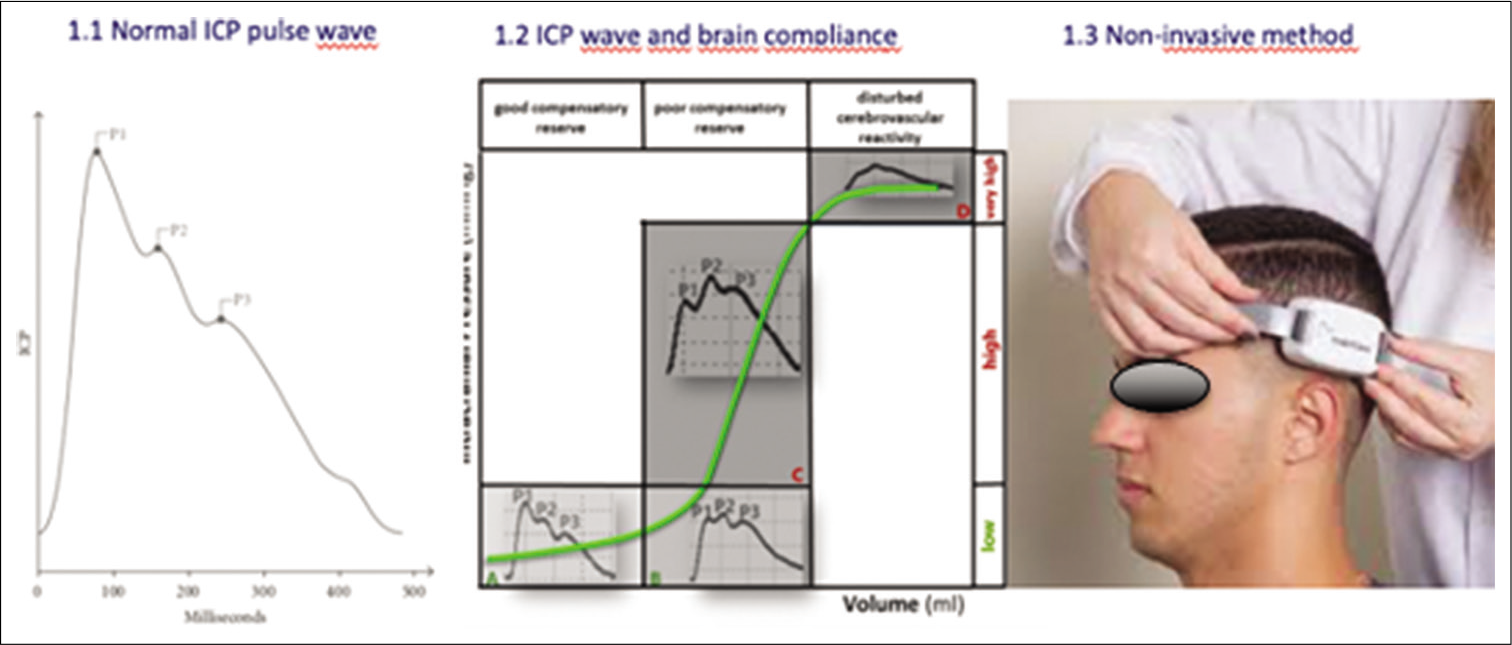
In this context, a group of Brazilian scientists (Braincare inc.) developed a non-invasive method for ICP monitoring, which uses an electric resistance extensometer that measures micro deformations of the skull and transforms this into an electrical signal. The notion that measuring the expansion of the skull as a reflection of increasing ICP has been explored in animal studies and cadavers since 1985 by Pitlyk. Subsequently, in 2009 Yue showed a positive correlation between increasing ICP and skull deformation.[
The equipment’s electric signal reflects the ICP waveform with its three classical peaks (P1, P2, and P3). Alterations in brain compliance change the pattern of ICP pulse morphology, leading to elevations of P2. Thus, the relation between P2/P1 indicates disturbed brain compliance and reflects elevated ICP indirectly[
The main utility of this new ICP monitoring equipment lies in utilizing it as a mean of predicting and preventing inordinate cerebral perfusion pressure. The idea of this non-invasive method is captivating once it is less inconvenient and avoid complications such as hemorrhage and infection.[
CASE PRESENTATION
A previously healthy 7-year-old girl started with progressive neck pain and headache, and after being evaluated for 2 weeks with several pediatrician consultations, progressed with a visual loss following these initial symptoms, and papilledema was observed in the ophthalmologist consultation. Subsequently, the patient was submitted for a MRI exam, which showed a partially empty sella, tortuosity of the optic nerves, and also the rectification of the retina. All of the MRI signs are common imaging findings in idiopathic intracranial hypertension (IIH)[
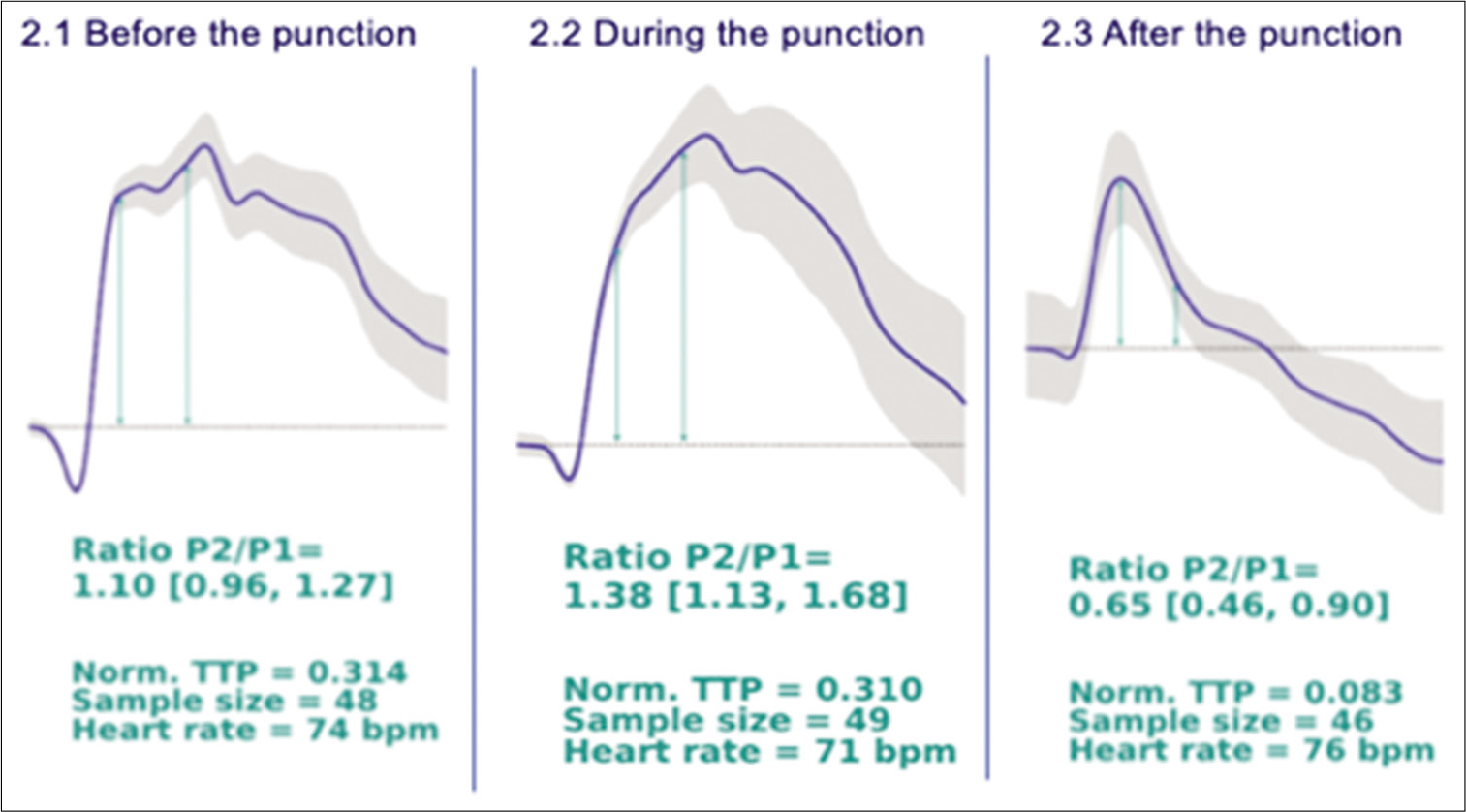
A LP with opening and closing pressure was performed, with continuous non-invasive ICP monitoring. Before the beginning of the procedure, the non-invasive measure showed a P2/P1 ratio of 1.1, reflecting altered brain compliance which expresses the capability to buffer an intracranial volume increase while avoiding a rise in ICP. During the procedure, the child started crying, with some loss on the quality of the signal acquired; however, the software could identify 1 min of good quality signal that showed a P2/P1 ratio of 1.38. The opening pressure was 32 cm H2O, and the closing pressure was 15 cm H2O and as a result, the child had prompt relief in her headache. Authors recommended that for children an opening pressure above 28 cm H2O should be considered as elevated ICP. Another study also considered CSF measures n28 cm H2O as “normal” for most children.[
After the procedure, the non-invasive method showed an evident normalization of ICP pulse curve morphology, with the P2/P1 ratio coming to 0.65 [
Figure 2:
Show the evolution of the wave form, (2.1) 30 min before punction represent P2/P1 wiht 1.10, representing high pressure, (2.2) represent an little bit higher during the procedure, (2.3) nevertheless after 60 min the punction pression get better, showing, that the noninvasive method might help in decision-making.
DISCUSSION
This is a concern because of the high morbidity in undiagnosed patients, and knowing the diagnostic criteria’s can be life-saving. The criteria’s for IIH is called modified Dandy criteria and include (1) signs and symptoms of raised ICP (headache, nausea, vomiting, transient visual obscurations, or papilledema), (2) the absence of localizing neurological signs with the exception of unilateral or bilateral abducens nerve palsy, (3) CSF opening pressure of >25 cm H2O with normal composition, and (4) normal to small ventricles as demonstrated by computed tomography (today, magnetic resonance imaging is the modality of choice). All findings corroborate to confirm the intracranial IIH.[
The most widespread use of measuring ICP (non-invasive) is via LP (invasive) and estimating ICP from LP is common in neurological practice and is widely used for assessing ICP in individuals with IIH events, although the limitations involved in estimating ICP by LP are well known, especially in overweight or obese patients.[
At this time, the patient results show a consistent change in the ICP pulse morphology accessed noninvasively before, during, and after the LP. We believe that the worsening of the P2/P1 ratio during the procedure was due to the discomfort caused by the puncture, with the child severely agitated, causing increased intrathoracic pressure, which reduces venous return and consequently increases ICP.
IIH treatment consists of reducing ICP seeking to eliminate symptoms such as headache and preserving visual function. Treatment options are quite varied in part due to the variety of specialists that treat patients with IIH, but regardless of the method, the goal is to decrease ICP that has to be closely monitored during treatment. Therefore, non-invasive methods to monitor ICP in patients with IIH would have significant impact not only during diagnosis but also during continuous treatment once it could reduce the requirement for gold standard, invasive approaches such as LP.
This new ICP monitoring wire not only showed accurate and reliable results but also can be easily managed, requiring minimal training and has a low cost. It can be an incredibly helpful tool in the follow-up of these patients helping clinical decisions like the need for new LPs or response to therapy, reducing the need for seriated MRI scans, costs and risk, collaborating to the patient’s well-being. It should be noted that intracranial disease processes and pathophysiological events involve complex cascades of events beyond alterations in ICP. ICP should always be measured along with other parameters such as brain tissue oxygenation, temperature, cerebral blood flow velocity, cerebral metabolism (micro-dialysis), and assessment of electrocortical activity. The multi-modality approach is fundamental and allows for incorporation of different aspects of the brain state in patient surveillance and can contribute to a more holistic view of the patient’s condition.[
CONCLUSION
ICP monitoring has become a clinical routine worldwide and represents a cornerstone in surveillance of patients with acute brain injury or disease, and diagnostic of individuals with chronic neurological disease. Certainly, seeking to reduce risks of infection, hemorrhage, falsely increased numbers and misplacement, the non-invasive monitoring technique should be taken into consideration in certain clinical scenarios such as IIH patients following up. Additionally, this new monitoring device is inexpensive, accurate, and also simple and convenient to use which can open doors toward a more equal medicine, especially in underdeveloped nations. In this case report, the ICP results were consistent elucidating that the use of this device in universities and research centers can expand the horizons of knowledge, but further evidence is needed before it becomes an alternative to invasive techniques.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Abraham M, Singhal V. Intracranial pressure monitoring. J Neuroanaesthesiol Crit Care. 2015. 2: 193-203
2. Avery RA. Interpretation of lumbar puncture opening pressure measurements in children. J Neuroophthalmol. 2014. 34: 284-7
3. Bidot S, Saindane A, Peragallo J, Bruce B, Newman N, Biousse V. Brain imaging in idiopathic intracranial hypertension. J Neuroophthalmol. 2015. 35: 400-11
4. Mascarenhas S, Vilela GH, Carlotti C, Damiano LE, Seluque W, Colli B. The new ICP minimally invasive method shows that the Monro-Kellie doctrine is not valid. Acta Neurochir Suppl. 2012. 114: 117-20
5. Mokri B. The Monro-Kellie hypothesis: Applications in CSF volume depletion. Neurology. 2001. 56: 1746-8
6. Nag DS, Sahu S, Swain A, Kant S. Intracranial pressure monitoring: Gold standard and recent innovations. World J Clin Cases. 2019. 7: 1535-53
7. Prabhakar H, Bithal P, Suri A, Rath G, Dash H. Intracranial pressure changes during valsalva manoeuvre in patients undergoing a neuroendoscopic procedure. Minim Invasive Neurosurg. 2007. 50: 98-101
8. Schexnayder LK, Chapman K. Presentation, investigation and management of idiopathic intracranial hypertension in children. Curr Paediatr. 2006. 6: 336-41
9. Thurtell MJ. Idiopathic intracranial hypertension. Continuum (Minneap Minn). 2019. 25: 1289-309
10. Xu DS, Hlubek RJ, Mulholland CB, Knievel KL, Smith KA, Nakaji P. Use of intracranial pressure monitoring frequently refutes diagnosis of idiopathic intracranial hypertension. World Neurosurg. 2017. 104: 167-70
11. Yue X, Wang L. Deformation of skull bone as intracranial pressure changing. Afr J Biotechnol. 2009. 8: 745-50






Dinesh Naidoo
Posted November 12, 2021, 7:11 pm
I rarely reform,if ever, LP in the prone position .Flouroscopy can be used equally well in the lateral position ,if needed and is rarely necessary in children