- Chief of Neurosurgical Spine and Education, Winthrop University Hospital, Mineola, New York - 11501, USA
- NYU Winthrop Hospital, NYU Winthrop NeuroScience, Mineola, USA
Correspondence Address:
Nancy E. Epstein
NYU Winthrop Hospital, NYU Winthrop NeuroScience, Mineola, USA
DOI:10.4103/sni.sni_150_17
Copyright: © 2017 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Nancy E. Epstein, Renee D. Hollingsworth. Nursing Review Section of Surgical Neurology International Part 2: Lumbar Spinal Stenosis. 07-Jul-2017;8:139
How to cite this URL: Nancy E. Epstein, Renee D. Hollingsworth. Nursing Review Section of Surgical Neurology International Part 2: Lumbar Spinal Stenosis. 07-Jul-2017;8:139. Available from: http://surgicalneurologyint.com/surgicalint-articles/nursing-review-section-of-surgical-neurology-international-part-2-lumbar-spinal-stenosis/
Abstract
Background:The lumbar spine includes 5 lumbar vertebral bodies, L1, L2, L3, L4, and L5. At each level, there is a disc space defined by the two bones (vertebral bodies) in the back; for example, there is a disc space at the L5-S1 level etc. The normal front to back (anterior to posterior or AP diameter) measurement of the spinal canal is typically 18-20 mm, but some patients have narrowing called spinal stenosis.
Methods:Lumbar stenosis is defined by two major types. Central stenosis compresses the midline (in the middle) sac of nerve tissue (dural or thecal sac containing the lumbar nerve roots). Lateral recess stenosis (off to the sides) compresses the individual exiting nerve roots.
Results:At each lumbar level, there may be compression of the nerve tissue centrally (dura also called cauda equina) or the nerve roots (on one or both sides). Compression may occur due to soft or calcified discs in the front (anteriorly) of the spine at different levels or from behind (posteriorly) due to arthritic enlargement (hypertrophy) or calcification (ossification) of the yellow ligament, facet joints, and/or bones (laminae). Surgery to remove bone and arthritic structures from the back of the spinal canal to decompress nerve tissue is called a laminectomy.
Conclusions:Patients with narrowing of the lumbar spinal canal may have central or lateral recess stenosis that compresses the thecal sac and/or exiting nerve roots at any of 5 levels. Laminectomy, performed at single or multiple levels, decompresses lumbar spinal stenosis.
Keywords: Laminectomy, lumbar stenosis, ossified yellow ligament, neurogenic claudication
INTRODUCTION
In this review, we define the clinical presentation, radiographic findings [e.g., X-ray, magnetic resonance (MR), and computed tomographic (CT) studies] and surgery consisting of laminectomy performed for lumbar spinal stenosis [Figures
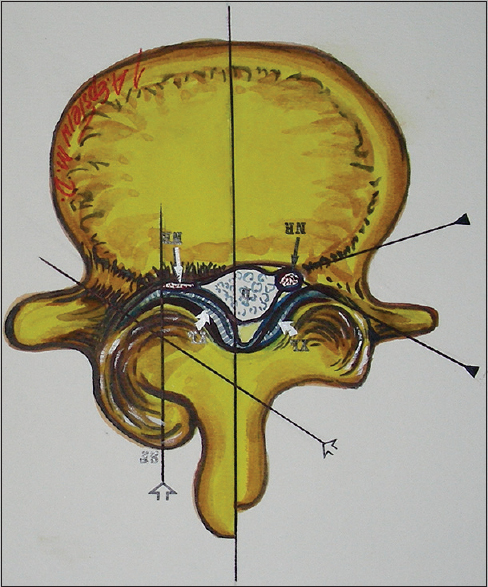
Figure 1
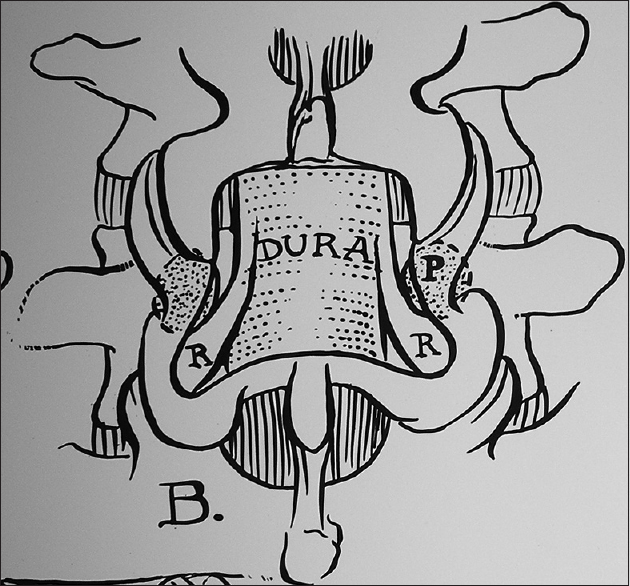
Illustration anatomy of lumbar stenosis: Definitions of central and lateral recess stenosis. The normal anterior posterior (AP) diameter of the lumbar spinal canal is 18 mm. Congenital central stenosis is defined as 10 mm in AP diameter, measured from the mid aspect of the ventral vertebral body to just under the spinous process in the midline. Acquired stenosis is defined by a central 13 mm in canal AP diameter. There is also lateral recess stenosis that compresses the nerve root off to the side (labeled NR)
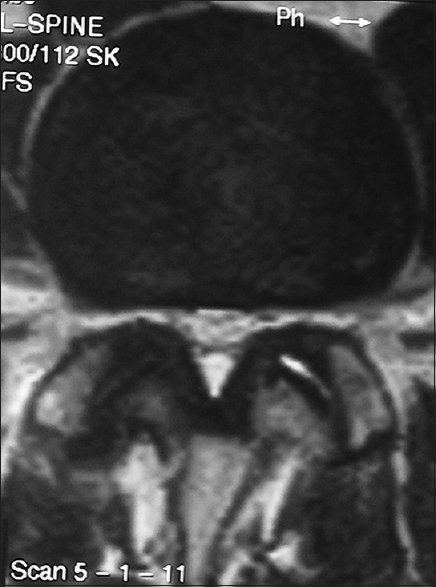
Figure 3
Axial T2-weighted MR documenting central and lateral recess stenosis. This axial T2-weighted MR (when the spinal fluid is turned white or hyperintense) of the lumbar spine shows diffuse front to back (anterior/posterior) compromise of the thecal sac (that contains the neural tissue in the spinal canal). From behind, there is enlargement of the yellow ligament (appearing black or hypointense) that markedly reduces the room available for the thecal sac centrally, as well as for the nerve roots (off to the side). Note there is also a small amount of fluid (hyperintense/white) in the left facet joint
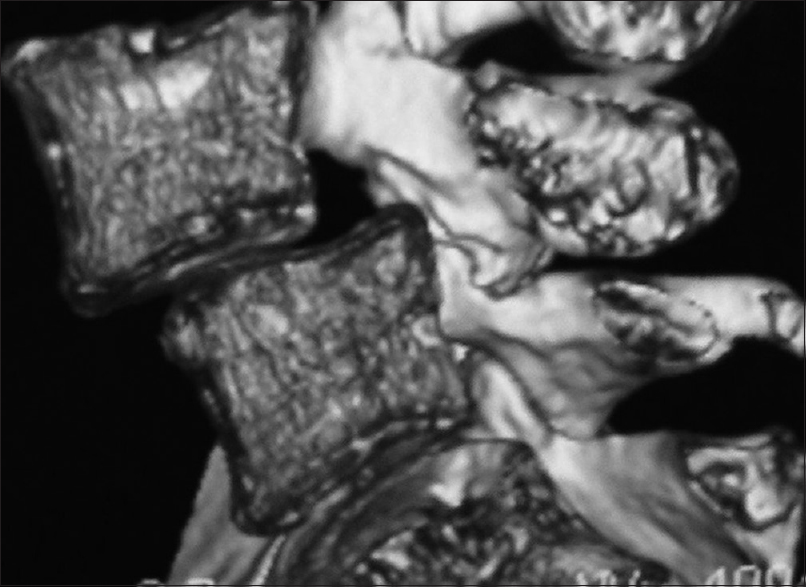
Figure 4
Sagittal T2-weighted MR showing marked L4-L5 spinal stenosis. On sagittal T2 MR (the spinal fluid is white or hyperintense) image, there is multilevel compression of the thecal sac (dural sac containing nerve roots of the lumbar spinal canal; cauda equina). This results in scalloping anteriorly (arthritic changes of the discs in the front) and posterior compression (hypertrophy/ossification of the yellow ligament and laminae from the back). Also note a minimal grade I slip at the L4-L5 level (spondylolisthesis) contributing to the narrowing
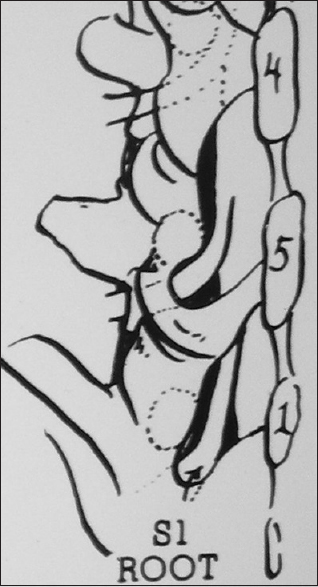
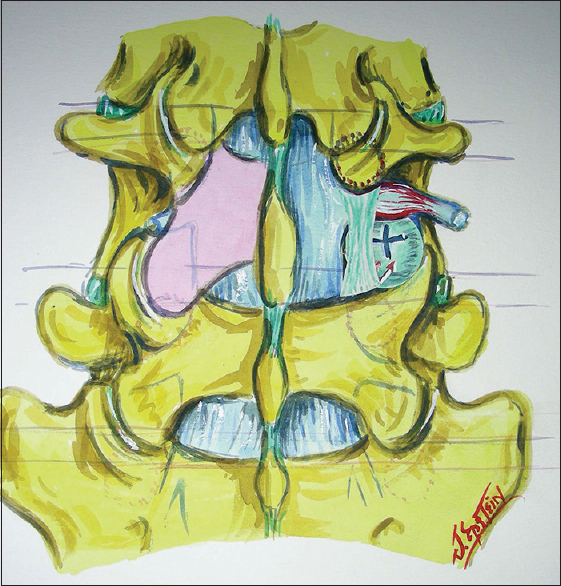
Figure 6
Illustration of two level laminotomy at the L4-L5 and L5S1 levels. In this illustration (Joseph A. Epstein M.D., Copyright Nancy E. Epstein M.D.), on the left, there are two laminotomies decompressing the L4-L5 and L5S1 levels. At the L4-L5 level, you can see the thecal sac/dura centrally and the inferiorly exiting L5 nerve root. At the L5-S1 level, the thecal sac/dura is again seen centrally, but the S1 nerve root has been skeletonized/decompressed (labeled S1 Root)
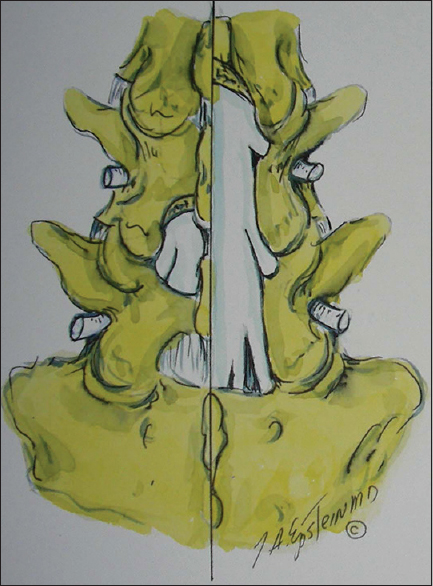
Figure 7
Coronal hemilaminectomy (laminectomy of part of the L4 and L5 levels). In this illustration (Joseph A. Epstein M.D., Copyright Nancy E. Epstein M.D.) half of the lamina of L4 above (superiorly) and half of the lamina below (inferiorly) of L5 have been removed. This provides central decompression of the thecal sac and the nerve roots on both sides
Figure 8
Left-sided partial laminectomy L4-L5 (laminotomy) and right-sided multilevel laminectomy L3, L4, L5, and S1. In this illustration (Joseph A. Epstein M.D., Copyright Nancy E. Epstein M.D.) on the left side of the spinal canal at the L4-L5 level, part of the lamina above of L4 and below of L5 has been removed (e.g., laminotomy). On the right side, a multilevel laminectomy of the L3, L4, L5, and S1 levels has been completed
Figure 9
Illustration of left L4 hemlaminectomy with inferior facectectomy and right L4 hemilaminectomy with full L4-L5 facet removal. In this illustration (Joseph A. Epstein M.D., Copyright Nancy E. Epstein M.D.) the Left L4 hemilamina has been removed along with the inferior articular facet (this attaches the L4 lamina to the L4-L5 facet joint). There is an L4 hemilaminectomy on the right with full removal of the L4-L5 facet joint. The latter may be warranted for discs that extend off to the side (lateral/foraminal/far lateral)
ANATOMY OF LUMBAR STENOSIS
The lumbar spine includes 5 lumbar vertebrae L1- L5. At each level, the structures in front of the spine (anterior) include the vertebral bodies, with ligaments; in front of the vertebral bodies you have the anterior longitudinal ligament (ALL), whereas behind the vertebral bodies you have the posterior longitudinal ligament (PLL). Both ligaments extend from the occiput all the way down to the sacrum. In the back (posterior) of the spinal canal, there is a lamina at each of the L1-S1 levels (L1, L2, L3, L4, L5, and S1 the top of the sacrum), a yellow ligament that goes from the lamina above (mid aspect) to the lamina below (top edge), a central spinous process, and facet joints on both sides that connect to the adjacent levels above (superiorly) and below (inferiorly) [Figures
Definitions of lumbar stenosis: Central and lateral recess stenosis
The normal front to back (anterior to posterior or AP canal diameter) measurement of the spinal canal in the midline is 18-20 mm. In some cases, patients are born with narrowed spinal canals (congenital stenosis: 10 mm AP diameter), and in other instances, they acquire arthritic changes resulting in narrowing over time (13 mm: relative stenosis). Patients may have narrowing of the lumbar spinal canal centrally (central stenosis) or off to the sides (lateral recess stenosis). Compression of the neural tissues may be attributed to arthritis/hypertrophy/ossification/calcification of the discs and/or ligaments in the front of the spinal canal (anteriorly). Similar arthritic changes may involve the laminae, yellow ligaments, and/or facet joints behind (posteriorly) the spinal canal. Midline stenosis compresses the central sac of nerve tissue (e.g., the dural/thecal sac containing the spinal fluid and lumbar nerve roots called the cauda equina). Compression to the sides impinges on the individual exiting nerve roots. At any disc space level, the higher numbered nerve root is compressed; for example, at L4-L5, stenosis compresses the L5 nerve root or roots.
CLINICAL SYMPTOMS OF LUMBAR STENOSIS
Pain
Low back pain is a very nonspecific finding. It may be due to lumbar spinal stenosis involving individual nerve roots or compression of all the nerve roots (cauda equina). It may be present with the patient at rest and/or with ambulation and/or other movement. It is important to differentiate the source of pain, as up to 10% of older patients with upper thigh/groin pain may have hip disease and others may have arterial vascular compromise (peripheral vascular disease).
Radiculopathy
Radiculopathy defines pain or a neurological deficit that correlates with compression/compromise of a nerve root in a specific distribution. This may involve single or multiple nerve roots within the stenotic lateral recesses, or centrally with diffuse midline stenosis.
Neurogenic claudication
Neurogenic claudication defines pain that occurs when a patient with lumbar stenosis ambulates a specific distance. This typically starts with patients complaining of pain on one or both sides after walking a few blocks (e.g., last year), and with time (e.g., this year), the distance is shorter. To relieve the pain, the patient has to stop, rest, bend forward, and/or sit down (this “opens” the spinal canal and temporarily relieves compression). Once the pain resolves, the patient starts up all over again. Eventually, these symptoms progress to the point they are present just upon standing, and eventually even sitting does not relieve the pressure (e.g., with the most severe stenosis). Alternatively, patients with vascular claudication just have to stop and rest.
Cauda equina syndrome
In patients with severe lumbar central stenosis, the marked compression of the dural sac containing the lumbar nerve roots may result in paralysis of the lower extremities accompanied by bowel/bladder (sphincter) dysfunction. This deficit is also called a cauda equina syndrome.
CLINICAL SIGNS OF SPINAL STENOSIS
Mechanical findings (femoral stretch test and straight leg raising signs)
Due to the typically slow progression of lumbar stenosis, patients often have minimal mechanical findings defined by the femoral stretch test (L2-L4) or the straight leg raising (sciatic nerve L5-S1) sign. The femoral stretch test (L2-L4) is elicited by stretching one leg (at a time) backward with the patient standing or laying down. The straight leg raising test (L5, S1) can be assessed with the patient laying down, sitting or standing, and lifting the left to 90 degrees. These maneuvers compromise the individual nerves at the site of stenosis.
Motor deficits
Patients with lumbar stenosis may or may not have motor weakness on one or both sides. The location of weakness depends on where the stenosis is located; it may impact the nerve root(s) off to one or both sides (lateral recess stenosis), or in the midline (central stenosis with dural compression). Weakness is graded as 0 (paralysis), 1 (flicker/no movement), 2 (movement not against gravity), 3 (movement against gravity but not against resistance), 4 (movement against some resistance), and 5 (normal strength).
L1-L2, L2-L3, L3-L4 levels (L2-L4 femoral nerve compromise)
A motor deficit involving the L2-L4 nerve roots on one or both sides (femoral nerve) may result in weakness in lifting the leg/thigh (iliopsoas) and/or straightening the knee (quadriceps). If there is central stenosis and marked compression of the entire dural/thecal sac, the patient may demonstrate paralysis (e.g., cauda equina syndrome) with sphincter loss (bladder and rectal dysfunction).
L4-L5 level (L5 sciatic nerve distribution deficits)
If there is compression at the L4-L5 level, L5 root compromise on one or both sides may result in a foot drop (e.g. difficulty pulling the foot/ankle up or weakness of the extensor hallucis longus/dorsiflexors). If there is profound central canal compression, the patient may exhibit a cauda equina syndrome with bowel/bladder dysfunction and a bilateral foot drop (L5).
L5-S1 level (S1 sciatic nerve distribution deficits)
Stenosis at the L5-S1 level compresses the S1 nerve root that is responsible for pushing the foot down (plantar flexor weakness indicated by an inability to walk on toes) on one or both sides. Again, if there is central compromise, the patient may demonstrate a cauda equina syndrome with accompanying plantar flexor weakness.
Reflex changes
Reflex loss is graded as 0 (absent reflex), 1+ (trace), 2+ (normal), 3+ (brisk), 4+ (nonsustained clonus), and 5+ (sustained clonus). The former 0–1+ are considered hypoactive, 2+ is normal, whereas the latter, 3+–5+ are defined as hyperactive. With compression of the L2-L4 nerve roots (at the L12/L23/L34 levels), the knee jerk (Patellar responses) may be diminished/absent. Compromise of the L5, S1 roots at the L4-L5 and L5-S1 levels, respectively, may result in loss of the ankle jerk (Achilles responses). Alternatively, if a patient has a lesion higher up in the spinal canal resulting in cord compressino (e.g. cervical, thoracic), Patellar and Achiles responses may be hyepractive (3+ to 4+).
Sensory loss
The sensory exam tests for pin, light touch, vibration, and position appreciation. However, the latter loss of vibration and position appreciation often correlates with disease higher up in the spine involving the cervical and thoracic cord.
L1-L2, L2-L3, L3-L4 levels
Compromise at the L1-L2, L2-L3, and L3-L4 levels many result in loss of pin appreciation and light touch sensation in the L2, L3, and L4 root distributions. For the L2 and L3 nerve roots, sensory deficits involve the groin and thigh regions. For L4, it extends over the lower (distal) thigh, crosses the knee, and involves the inner (medial) aspect of the calf.
L4-L5, L5-S1 levels
At the L4-L5 level, the L5 nerve root may be compromised. This results in sensory loss to pin/light touch over the outside (lateral aspect) of the calf and over the top (dorsum) of the foot. At the L5-S1 level, S1 sensory changes involve the outside (lateral) portion of the foot and the sole of the foot.
Cerebellar dysfunction
Cerebellar dysfunction is tested in the lower extremities by having the patient walk heel to toe on an imaginary line [(e.g., tandem gait testing also called the DWI test (drinking while intoxicated test)]. In addition, the patient is asked to run the heel of one foot down the shin on the other side, looking for incoordination. An inability to perform either of these tests may indicate disease not only of the lumbar spine but also potentially pathology involving the cervical or thoracic spinal cord.
RADIOGRAPHIC FINDINGS OF LUMBAR STENOSIS
X-rays
Plain X-rays of the lumbar spine are used to demonstrate alignment (stability/instability), bony configuration (no bony destruction, osteoporosis, fractures, etc.), and whether there is a lumbosacral anomaly (e.g., some patients have 4 and others 6 lumbar vertebral bodies – normal anatomic variant). Plain X-rays may show static motion (slippage that does not move and is therefore not unstable), whereas flexion/extension films may demonstrate active motion/instability.
Magnetic resonance
MRI of the lumbar spine best demonstrates soft tissue changes; it is like the chocolate inside the M and M, whereas the hard candy shell is the CT [Figures
CT
CT images of the lumbar spine best demonstrate the bones/calcified changes; it is like the hard candy shell of the M&M [
NONSURGICAL MANAGEMENT OF LUMBAR STENOSIS
Patients have differing degrees of symptoms/signs of lumbar stenosis. Those with only mild/moderate complaints may be managed without surgery and can be referred to neurology, psychiatry, physical therapy, etc. In addition, select older patients and/or those with multiple major comorbid risk factors (e.g., major cardiovascular disease/stents on blood thinners, artificial heart valves, obstructive pulmonary disease, morbid obesity, etc.) may not be appropriate candidates for lumbar surgery, and therefore, must be managed non surgically. Epidural injections for spinal stenosis have not been documented to offer any long-term benefit, and pose many major risks/complications (e.g., meningitis spinal abscess, spinal fluid leak/headaches, increased scarring, adhesive arachnoidits, death). Therefore Epidural Steroid Injections should not be performed.
SURGICAL OPTIONS FOR SPINAL STENOSIS
Surgery for lumbar stenosis most commonly includes single/multilevel laminectomy/laminectomies. are performed with patients face down (prone) and involve the removal of bone from the back of the spinal canal along with the attendant arthritic tissues (e.g., compressive ossified/hypertrophied yellow ligament, cysts, and laminae).
CONCLUSION
The lumbar spine includes 5 lumbar vertebral bodies (L1-L5) and 5 disc spaces (i.e., L1-L2, L2-L3, L3-L4, L4-L5, and L5-S1). Spinal stenosis may compress the midline lumbar nerve roots (central stenosis; cauda equina compromise) or the nerve roots off to the sides (lateral recess stenosis). Patients may exhibit pain, radiculopathy, and neurogenic claudication that correlates with mild-to-major neurological deficits (e.g., cauda equina syndrome/major paralysis). Although select patients may improve with nonsurgical options, many others will maximally benefit from surgery consisting of lumbar laminectomy.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.









Donald Willis
Posted May 4, 2020, 2:22 pm
Back in Feb I had spinal fusion surgery I could walk when I went and 16 weeks can’t walk at all now my doctor want to work on L2. 3.4.5 to remove spar .
I’m really not sure this is for me i understand 75 percent dont work