- Departments of Neurosurgery, University of São Paulo, São Paulo, Brazil.
- Department of Neurosurgery, Air Force Galeão Hospital, Rio de Janeiro, Brazil.
- Departments of Pathology, University of São Paulo, São Paulo, Brazil.
Correspondence Address:
Eberval Gadelha Figueiredo
Departments of Neurosurgery, University of São Paulo, São Paulo, Brazil.
DOI:10.25259/SNI_492_2019
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Nicollas Rabelo, Vinicius Trindade Gomes da Silva, Marcelo Prudente do Espírito Santo, Davi Solla, Dan Zimelewicz Oberman, Bruno Sisnando da Costa, Fernando Pereira Frassetto, Manoel Jacobsen Teixeira, Eberval Gadelha Figueiredo. Orbit ossifying fibroma – Case report and literature review. 28-Feb-2020;11:35
How to cite this URL: Nicollas Rabelo, Vinicius Trindade Gomes da Silva, Marcelo Prudente do Espírito Santo, Davi Solla, Dan Zimelewicz Oberman, Bruno Sisnando da Costa, Fernando Pereira Frassetto, Manoel Jacobsen Teixeira, Eberval Gadelha Figueiredo. Orbit ossifying fibroma – Case report and literature review. 28-Feb-2020;11:35. Available from: https://surgicalneurologyint.com/surgicalint-articles/9883/
Abstract
Background:Ossifying fibroma (OF) is benign bone lesions, most frequent in young children, more common in the maxillary sinus and mandible (75–89%), the pathogenesis of the tumor is not clear, there are many subtypes of OF. This paper aims to report an OF a case and literature review.
Case Description:Male, 19 years old, with a progressive history proptosis since 2012, diagnosed as a right supraorbital lesion at an external service and assigned to conservative management. Then, he evolved with double vision, which worsened in February of 2018, associated with a moderate headache. On admission: proptosis and downward deviation of the right orbit was noticed on the physical exam and with exception of limited right upgaze, external ocular movements were maintained. Head computed tomography showed a multiloculate expansive osteolytic lesion at the right orbital roof. On magnetic resonance imaging, the lesion had an inner content with septations, T1-weighted imaging heterogeneous signal, T2-weighted imaging high signal intensity, and peripheral contrast enhancement. The patient underwent a right frontal craniotomy with a gross total resection and the postoperative follow-up was uneventful. Menzel reported the first case in 1782. The clinical findings depend on localization. There are five subtypes. In general, the lesions have a radiological appearance with hyperdense boundary and cause deformity and destruction in bones with high recurrence risk. Radical resection is curative.
Conclusion:As a result, the correlation of clinical, radiologic, and pathologic data is significant while going for a specific diagnosis in cases of craniofacial fibrous lesions. Total excision is the best treatment, but it can recur.
Keywords: Cranium tumors, Neurosurgery, Orbit lesions, Ossifying fibroma, Proptosis
INTRODUCTION
Ossifying fibroma (OF) is benign bone lesions, most frequent in young children (10 years). They are more found in the maxillary sinus and mandible (75–89%). It has also been reported in the paranasal sinuses, frontal, ethmoid, and sphenoid bones, and orbital roof.[
Primary orbital bone tumors represent 0.6–2% of all orbital tumors and 23% of all lesions involving bone, the most common of which are fibrous dysplasia (FD) and osteoma. The incidence of orbital OF is difficult to estimate; however, a review of 3000 fibro-osseous lesions collected by the Armed Forces Institute of Pathology reported 30 cases.[
The pathogenesis of the tumor is not clear and a few theories have been proposed. Trauma has been suggested as a biological factor. A developmental abnormality has also been recommended since this tumor usually arises from membranous bone and occurs in patients in a young age group.[
They are generally slow-developing benign tumors. However, these lesions are destructive and have a high risk of recurrence unless surgeons eradicate them. The term juvenile is used primarily in children and a young adult population occurrence and can be more aggressive than adults. OF which arise on the middle face and the paranasal sinuses are also more aggressive.[
CASE REPORT
D.L.F., male, 19-year-old, presented a progressive proptosis in 2012, associated with occasional mild headache. On the same year, he sought medical consultation at an external service and after imaging investigation, a right supraorbital lesion was found. It was decided conservative management with imaging follow- up. Three years later, the patient joined a phosphoethanolamine clinical trial, which he left after approximately 1 year. At that time, he also presented with double vision. On February of 2018, the headache worsened, as well as the diplopia. Due to the worsening, he was referred to the Hospital das Clinicas at the University of Sao Paulo. In the neurological exam, he was alert and oriented; there was proptosis (Grade I) and downward deviation of the right eye. The external ocular movements, visual acuity, and campimetry were preserved, and there were no motor or sensorial impairments.
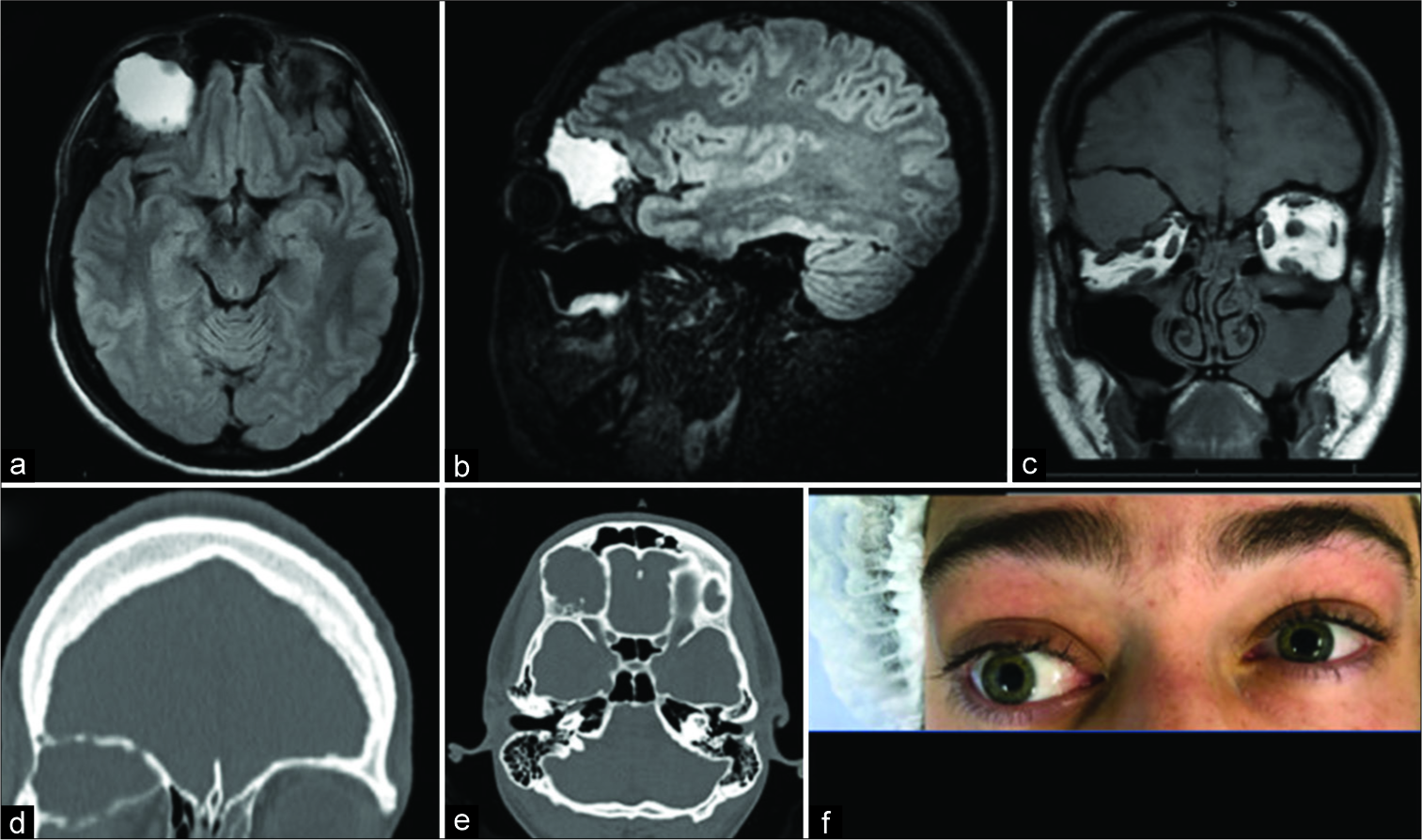
Head computed tomography (CT) showed a multiloculated expansive lesion on the right orbital roof, sized 3.3 × 4.0 × 2.8 cm (LL × AP × CC), with osteolytic characteristics. There was a bulging of the anterior cranial fossa and right frontal sinus superiorly. The superior orbital fissure and the optic nerve canal were preserved.
Magnetic resonance imaging (MRI) revealed a well- circumscribed multicystic lesion with peripheral hypointense capsule and mild internal septations with variable signal intensity at T1-weighted imaging (T1WI). On T2, the cystic cavities showed high signal intensity. There was the obliteration of the extra and intraconal fat tissue and inferior dislocation of the lachrymal gland and extraocular muscles. Cystic walls were enhanced after injection of gadolinium [
Figure 1:
Expansive cystic bone formation in the right orbital roof, with peripheral enhancement through contrast with thin septations, measuring 3.3 × 4.0 × 2.8 cm (LL × AP × CC). It presents clear limits, with a “frosted glass” aspect in the bone portion in its periphery, especially in its inferomedial aspect. (a-c) Magnetic resonance imaging images, axial, sagittal, and coronal view, respectively. (d and e) Computed tomography images, coronal and axial view (f) there is consequent degree I proptosis of this side and displacement of the optic nerve.
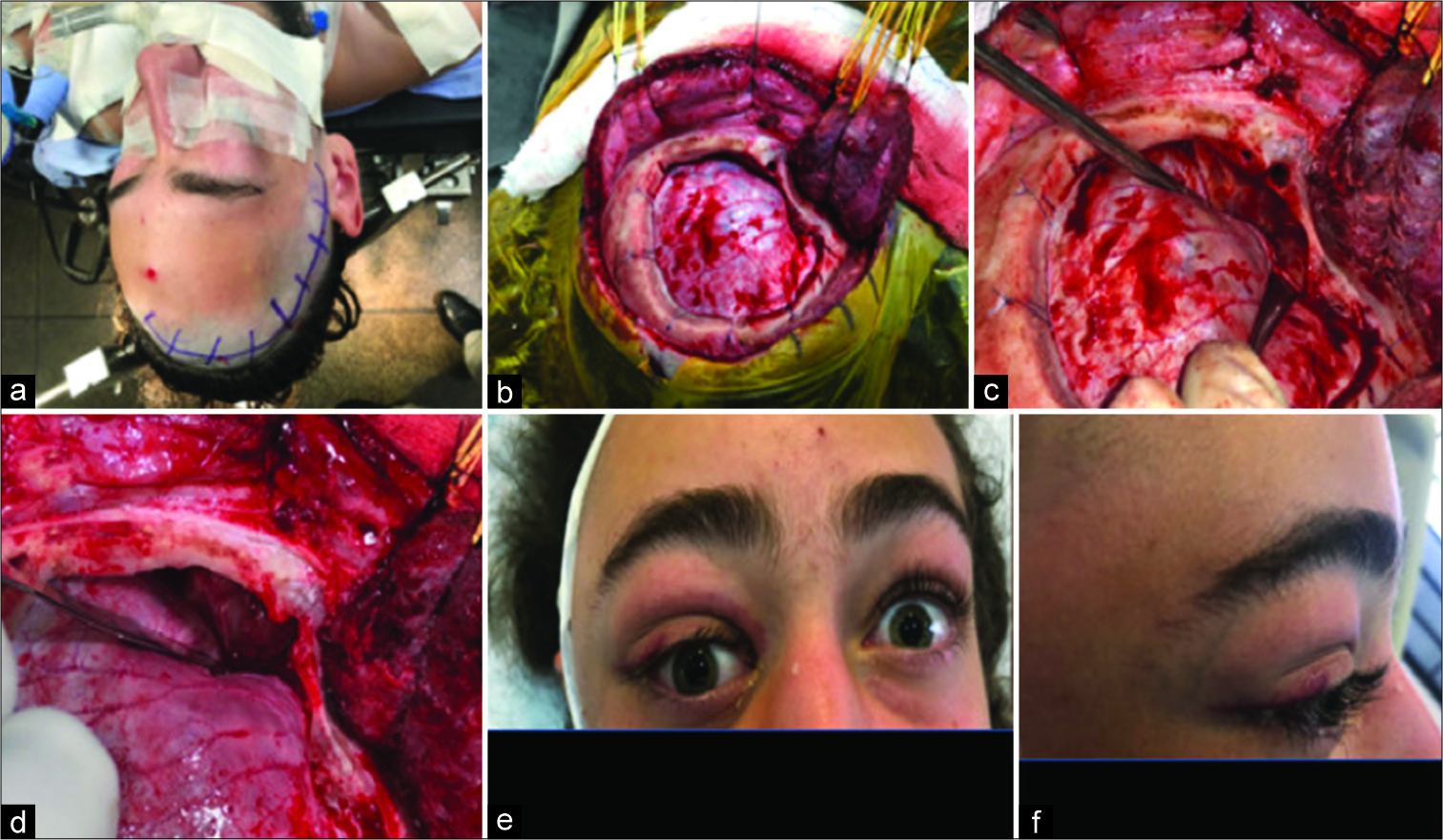
On March 7, he underwent a right frontal craniotomy for resection of the supraorbital lesion associated with high- speed drilling. Was made extended frontal pretemporal craniotomy, with wide orbital skull exposure. The main objective due to decompress optic nerve. All bone block was removed by drilling. Afterword’s the skull was reconstructed by methacrylate. The drilling was very tough. A solid bone makes it more difficult to remove. The postoperative follow- up was uneventful, with reduction of the proptosis [
Figure 3:
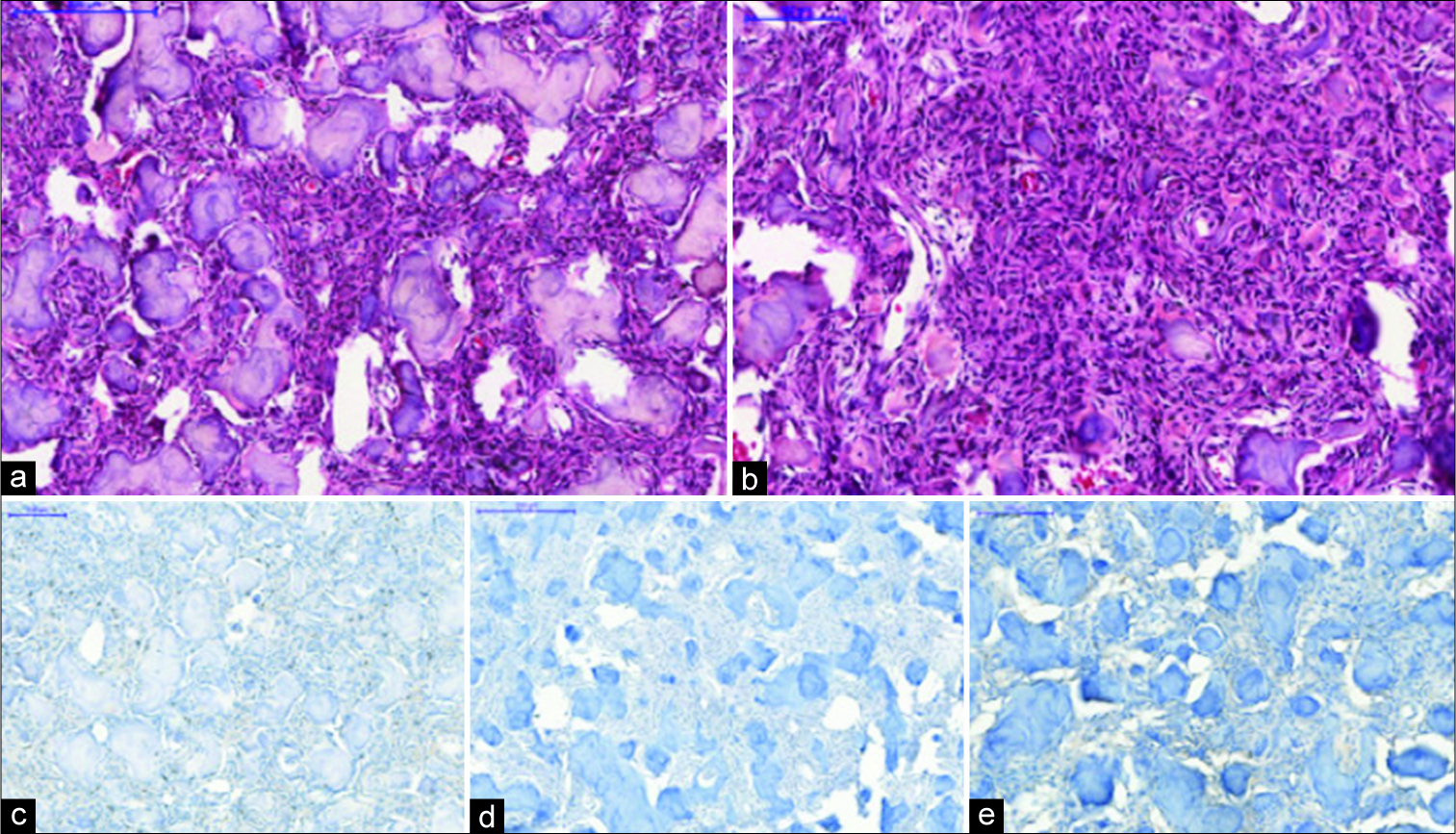
Juvenile psammomatoid: (a and b) hematoxylin and eosin analysis: disconnected spicules of irregularly shaped bone often with hemorrhage and occasional giant cells; prominent osteoblast lining may be seen, as well as occasional partially lamellar bone with numerous round psammoma-like calcified bodies are identified. (c-e) Immunohistochemistry analysis: the markers performed are only for a differential with meningothelial/neural sheath tumors. The three are negative: progesterone receptor, epithelial membrane antigen, and S-100.
DISCUSSION
There are many differential diagnoses for bone lesions in the skull base. The spectrum of possibilities includes benign lesions, as osteomas and osteoid osteomas, reactive expansile nonneoplastic lesions, primary malignant tumors, and metastatic lesions. Although rare, fibro-osseous lesions are one of these possibilities.[
Benign fibro-osseous lesions (BFOLs) are characterized by a fibrocellular stroma with varying degree of mineralized material leading to the replacement of physiological bone architecture with fibro-osseous tissue. FD, OF, and cemento- osseous dysplasia are the noted BFOLs.[
The recent World Health Organization classification of head and neck tumors in 2017 described four fibro-osseous lesions: OF, FD, familial gigantiform cementoma (FGC), and cemento-osseous dysplasia.[
OFs are benign fibro-osseous neoplasms affecting the craniofacial skeleton.[
FD is a skeletal developmental anomaly in which normal medullary bone is replaced by fibrous tissue. The lesions of the ethmoidal and sphenoid sinuses are seen less commonly. The monostotic form is observed in approximately 70–80%, whereas the involvement of the craniofacial bones in these lesions is approximately 25%. The polyostotic form is observed in approximately 30%, and in these lesions, which are observed in younger ages, the involvement of the craniofacial bones is approximately 50%. The association between polyostotic disease, abnormal skin pigmentation, and endocrinopathies may configure the McCune-Albright syndrome.[
FGC is a rare fibro-osseous disease. It affects da jaws characterized by a multifocal lesion with progressive growth I can be autosomal dominant but sporadic cases are also described. The treatment is challenging and complete surgical resection usually is impossible and the recurrence rates are high.[
Cemento-osseous dysplasia is the most common benign fibro-osseous lesion of the jaw. It occurs exclusively in the tooth-bearing regions of the jaw. In general, require no treatment and can be monitored during routine dental appointments.[
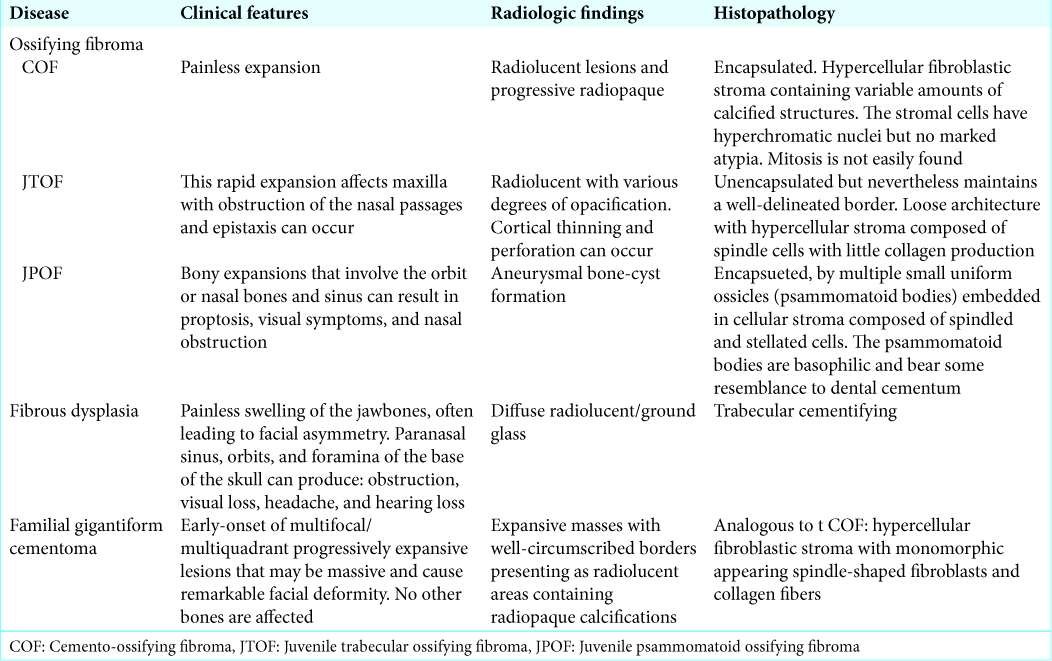
Clinical, radiographic, and microscopic parameters that distinguish among OFs and FD are summarized in
CONCLUSION
There are many differential diagnoses in skull base lesions. Most common are benign bone tumors; however, fibro- osseous lesions should be remembered mainly FD and OFs as possible causes. In general, these lesions must be treated with a complete surgical resection, minimizing the recurrence rates.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
HIGHLIGHTS
OF are benign bone lesions, most frequent in young children, and maxillary sinus and mandible (75–89%) Primary orbital bone tumors represent 0.6–2% of all orbital tumors and 23% of all lesions involving bone Head CT showed a multiloculate expansive osteolytic lesion at the right orbital roof. On MRI, the inner content had septations, T1WI variable signal intensity and T2-weighted imaging high signal intensity with fluid-fluid level, and contrast enhancement of its walls Pathology: disconnected spicules of irregularly shaped bone often with hemorrhage and occasional giant cells; prominent osteoblast lining may be seen, as well as occasional partially lamellar bone. The immunohistochemical markers performed are only for a differential with meningothelial/neural sheath tumors. The three are negative: progesterone receptor, epithelial membrane antigen, and S-100 As a result, the correlation of clinical, radiologic, and pathologic data is significant while going for a specific diagnosis in cases of craniofacial fibrous lesions. Total excision is the best treatment, but recurrence can be seen.
References
1. Barrena López C, Bollar Zabala A, Úrculo Bareño E. Cranial juvenile psammomatoid ossifying fibroma: Case report. J Neurosurg Pediatr. 2016. 17: 318-23
2. Boyce AM, Burke A, Cutler Peck C, DuFresne CR, Lee JS, Collins MT. Surgical management of polyostotic craniofacial fibrous dysplasia: Long-term outcomes and predictors for postoperative regrowth. Plast Reconstr Surg. 2016. 137: 1833-9
3. Brademann G, Werner JA, Jänig U, Mehdorn HM, Rudert H. Cemento-ossifying fibroma of the petromastoid region: Case report and review of the literature. J Laryngol Otol. 1997. 111: 152-5
4. Commins DJ, Tolley NS, Milford CA. Fibrous dysplasia and ossifying fibroma of the paranasal sinuses. J Laryngol Otol. 1998. 112: 964-8
5. El-Mofty SK, Nelson B, Toyosawa S, El-Naggar AK, Chan JK, Grandis JR, Takata T, Slootweg PJ.editors. Ossifying fibroma. World Health Organization Classification Head and Neck Tumours. Lyon: IARC; 2017. p.
6. Hasturk A, Tun K, Guvenc Y, Kaptanoglu E. Cranial ossifying fibroma causing visual disorder. J Craniofac Surg. 2010. 21: 768-70
7. Johnson LC, Yousefi M, Vinh TN, Heffner DK, Hyams VJ, Hartman KS. Juvenile active ossifying fibroma. Its nature, dynamics and origin. Acta Otolaryngol. 1991. 488: 1-40
8. Katti G, Khan MM, Chaubey SS, Amena M. Cemento-ossifying fibroma of the jaw. BMJ Case Rep. 2016. 2016: bcr2015214327-
9. Linhares P, Pires E, Carvalho B, Vaz R. Juvenile psammomatoid ossifying fibroma of the orbit and paranasal sinuses. A case report. Acta Neurochir (Wien). 2011. 153: 1983-8
10. Margo CE, Ragsdale BD, Perman KI, Zimmerman LE, Sweet DE. Psammomatoid (juvenile) ossifying fibroma of the orbit. Ophthalmology. 1985. 92: 150-9
11. Martínez-Mañas RM, Rey MJ, Gastón F. Aggressive psammomatoid ossifying fibroma. Ann Otol Rhinol Laryngol. 2002. 111: 466-8
12. Marvel JB, Marsh MA, Catlin FI. Ossifying fibroma of the mid-face and paranasal sinuses: Diagnostic and therapeutic considerations. Otolaryngol Head Neck Surg. 1991. 104: 803-8
13. Rossi DC, Fiaschi P. Extensive fibrous dysplasia of skull base: Case report. Neurol Sci. 2015. 36: 1287-9
14. Sarode SC, Sarode GS, Ingale Y, Ingale M, Majumdar B, Patil N. Recurrent juvenile psammomatoid ossifying fibroma with secondary aneurysmal bone cyst of the maxilla: A case report and review of literature. Clin Pract. 2018. 8: 1085-
15. Villemure JG, Meagher-Villemure K. Giant ossifying fibroma of the skull. Case report. J Neurosurg. 1983. 58: 602-6