- Departments of Neurosurgery, Mohammed V University of Rabat, Hospital of Specialities-Rabat, Rabat, Morocco
Correspondence Address:
Meriem Kajeou, Department of Neurosurgery, Mohammed V University of Rabat, Hospital of Specialties Rabat, Rabat, Morocco.
DOI:10.25259/SNI_201_2025
Copyright: © 2025 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Meriem Kajeou, Israe Almaghribi, Yasser Arkha. Orbital leiomyoma mimicking a cavernous hemangioma. 06-Jun-2025;16:233
How to cite this URL: Meriem Kajeou, Israe Almaghribi, Yasser Arkha. Orbital leiomyoma mimicking a cavernous hemangioma. 06-Jun-2025;16:233. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=13606
Abstract
Background: Orbital leiomyoma is a rare benign tumor of the smooth muscles of the orbit with intraconal or extraconal location. The tumor affects twice as many men as women, with an average age of 30 years.
Case Description: A 38-year-old female presented with proptosis: Axile, nonpulsatile, painless, nonreducible, Grade III, with impairment of oculomotricity, associated with a decrease in visual acuity on the affected side with an AV at 03/10, and fundus: Grade I papilledema. The computed tomography scan showed a solitary, tissue mass, well-limited, encapsulated, and usually homogeneous, with homogeneous enhancement after contrast injection. The magnetic resonance imaging showed a rounded, homogeneous lesion, isointense on T1 and hyperintense on T2, with homogeneous enhancement after gadolinium injection. Suggestive of an intraorbital cavernous hemangioma. The patient underwent surgery via a subfrontal approach, with macroscopically complete resection. Histopathological examination was in favor of an orbital leiomyoma.
Conclusion: Although very rare, orbital leiomyoma should be considered in the differential diagnosis of patients with orbital tumors.
Keywords: Cavernous hemangioma, Leiomyoma, Orbital tumors
INTRODUCTION
Leiomyoma is a benign tumor arising from the smooth muscle, but its occurrence in the orbit is rare. Although these tumors are common, their unusual orbital location can make diagnosis challenging. Surgical excision is recommended to reduce exophthalmos and confirm the diagnosis. The prognosis after surgery is generally favorable.[
CASE REPORT
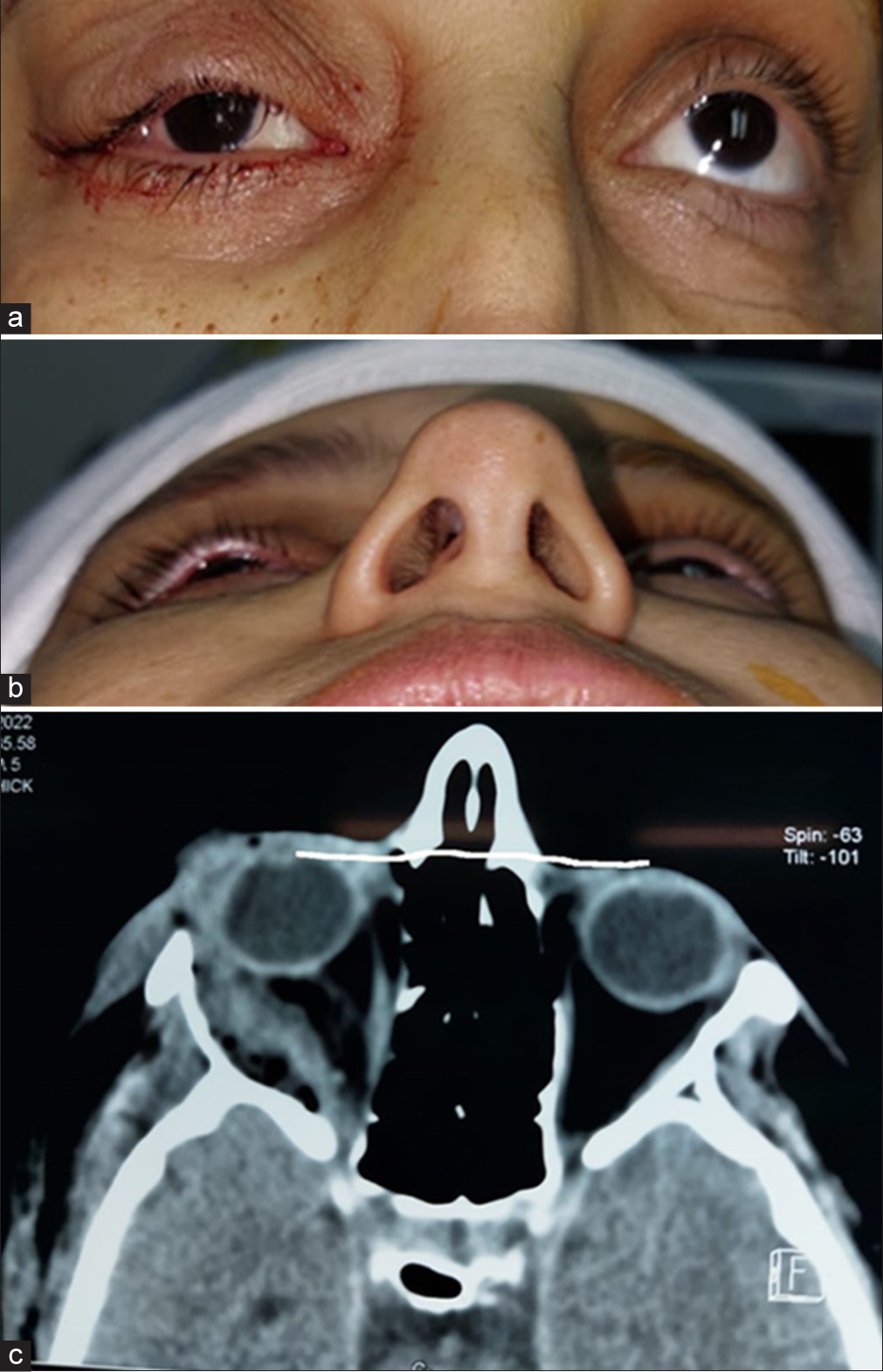
A 38-year-old female presented with right axial exophthalmos [
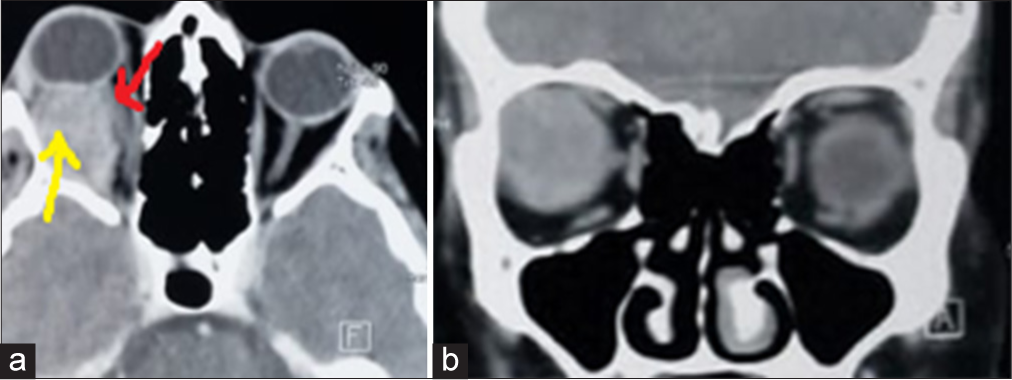
Computed tomography (CT) scan [
Figure 3:
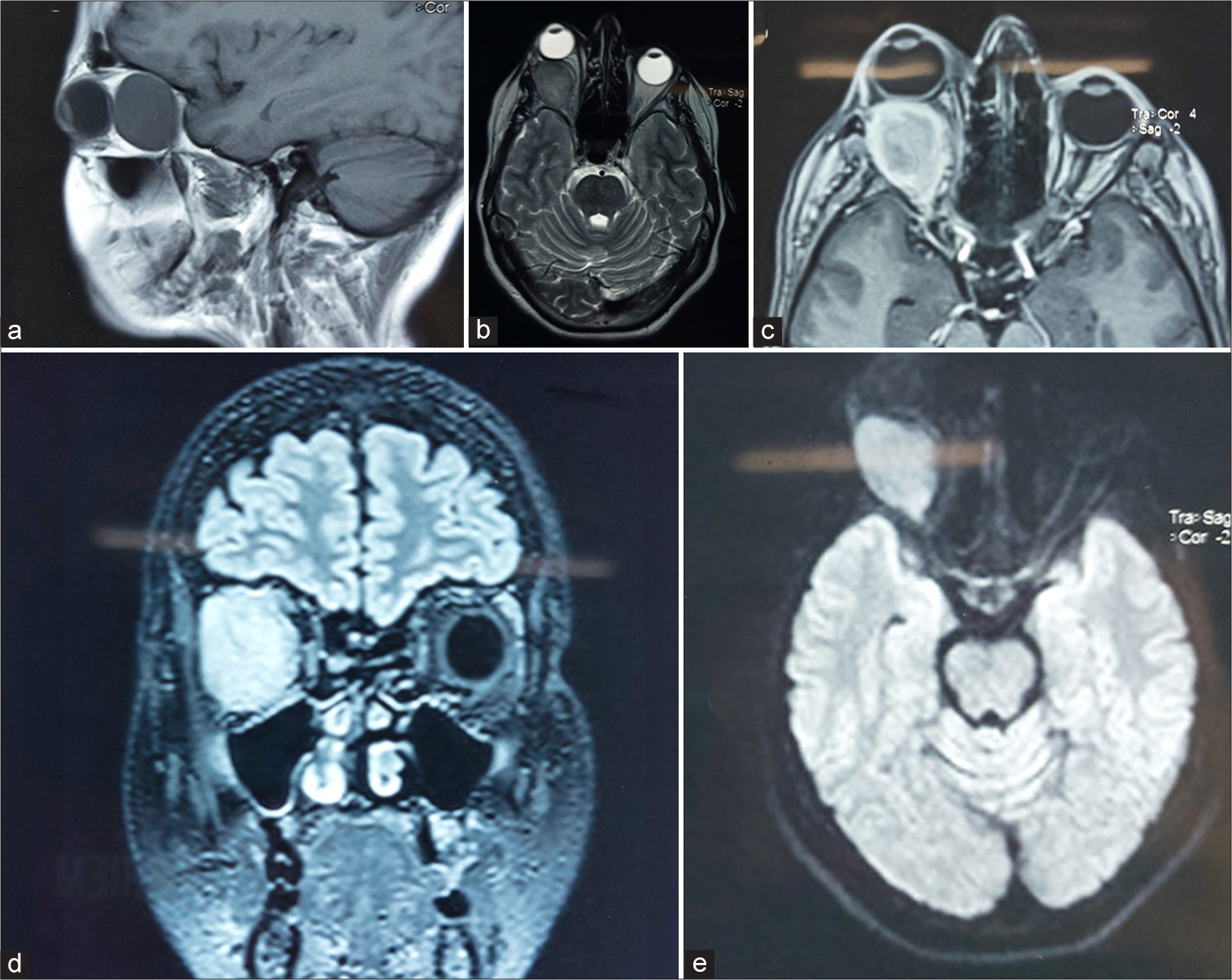
Magnetic resonance imaging showing a well-circumscribed right intracoronal lesion. (a) T1-weighted sagittal image and (b) T2-weighted axial image showing a well-defined isosignal area. (c) Axial T1-weighted image after gadolinium injection showing homogeneous contrast. (d) Coronal fluid-attenuated inversion recovery-weighted image and (e) axial diffusion-weighted image showing an isointense lesion.
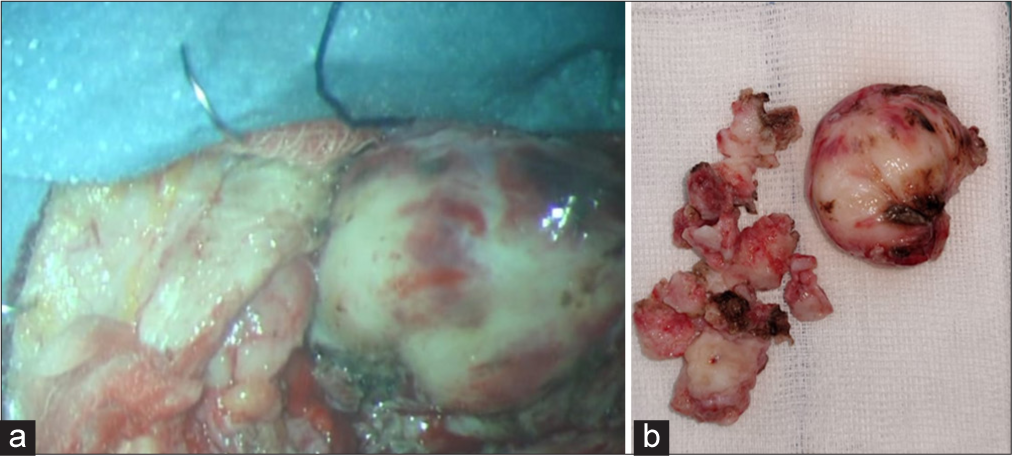
Surgical management was chosen, and the patient underwent surgery via a subfrontal approach. During the procedure, the lesion [
Figure 5:
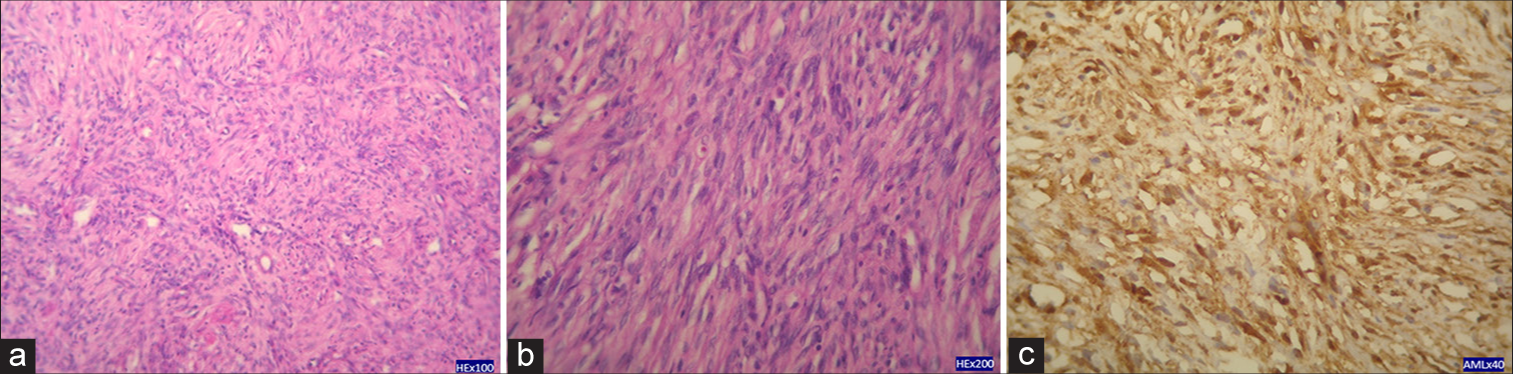
(a and b) Photomicrograph showing characteristic compact bundles of spindle cells with cigar-shaped nuclei. Nuclear palisading, mitotic activity, and necrosis are absent (hematoxylin– eosin, original magnification ×100). (c) Immunohistochemical analysis showing strong expression of smooth muscle actin (×40).
DISCUSSION
Leiomyoma is a rare tumor in the orbit due to the limited presence of smooth muscle tissue in this region. Lodato described the first case in 1896.[
MRI signal characteristics in this case were isointense in T1 and T2, with intense enhancement after gadolinium injection. The appearance was identical to that of cavernous hemangioma.[
A tumor composed of dense smooth muscle cells and relatively sparse vascularization could display signal characteristics similar to those of uterine leiomyomas, namely a weaker signal at T2. The differential diagnosis includes several entities. Cavernous hemangioma and schwannoma should be considered. MRI can distinguish a leiomyoma from a cavernous hemangioma, the latter being T2 hyperintense. However, the differentiation between a leiomyoma and a schwannoma is more complex, as both tumors show signals of similar intensity. Nevertheless, definitive diagnosis relies primarily on histopathological examination.[
Moreover, various surgical approaches may be considered depending on the tumor’s location and extent. Paluzzi et al. suggested that the orbit can be viewed as a clock, with the approach varying based on tumor position.[
The principle when choosing a surgical corridor is to avoid working across or around nerves. Specifically, one should avoid crossing the plane of the optic nerve. Therefore, orbital pathology lateral to the optic nerve is accessed through lateral orbitotomies, and medial pathology is accessed through medial orbitotomies.
Conventionally, external approaches to the orbit provide excellent access to tumors located superiorly and laterally to the optic nerve and orbit. These tumors are usually best approached via a pterional or fronto-orbital temporal craniotomy, with or without orbitozygomatic osteotomies.[
Extended endonasal approaches (EEAs) provide excellent access for intraconal and extraconal tumors that are medial and inferior to the optic nerve and can be applied to any medial intracranial extension, provided that key neurovascular structures (e.g., the optic nerve and internal carotid artery) remain lateral to the tumor. EEAs also provide access to most of the orbit, from the posterior globe to the orbital apex.[
In our case, although a minimally invasive approach could have been considered based on the tumor’s location, the initial radiological suspicion of a cavernous hemangioma with potential bleeding risk justified the choice of a subfrontal approach, offering better exposure and surgical control.
Histologically, the tumor consists of bundles of spindle-shaped smooth muscle cells interspersed with abundant endothelial sinusoids or dilated capillaries.[
At the end of the vascular spectrum, the tumor transitions into a cavernous hemangioma. Regardless of subtype, these tumors are encapsulated within a well-defined fibrous capsule. In some instances, satellite lobulations are observed, necessitating wide excision to ensure complete removal.[
The definitive treatment for orbital leiomyoma is a complete surgical extraction. Leiomyoma is a rare tumor in the orbit due to the limited presence of smooth muscle tissue in this region.[
CONCLUSION
Leiomyoma is a well-circumscribed benign orbital mass that is usually intracanal and probably arises from the orbital smooth muscle. The MRI appearance is similar to other well-encapsulated masses, such as cavernous hemangioma and schwannoma. Although rare, leiomyoma should be considered in this differential.
Ethical approval:
Institutional Review Board approval is not required.
Declaration of patient consent:
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship:
Nil.
Conflict of interest:
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation:
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript, and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Atlas SW. MR Imaging of the orbit: Current status. Magn Reson Q. 1989. 5: 39-96
2. Badoza D, Weil D, Zárate J. Orbital leiomyoma: A case report. Ophthalmic Plast Reconstr Surg. 1999. 15: 460-2
3. Carrier DA, Mawad ME, Kirkpatrick JB. MR appearance of an orbital leiomyoma. AJNR Am J Neuroradiol. 1993. 14: 473-4
4. Da Silva SA, Yamaki VN, Solla DJ, de Andrade AF, Teixeira MJ, Spetzler RF. Pterional, pretemporal, and orbitozygomatic approaches: Anatomic and comparative study. World Neurosurg. 2019. 121: e398-403
5. Henderson JW, Harrison E. Vascular leiomyoma of the orbit: Report of a case. Trans Am Acad Ophthalmol Otolaryngol. 1970. 74: 970-4
6. Jakobiec FA, Howard GM, Rosen M, Wolff M. Leiomyoma and leiomyosarcoma of the orbit. Am J Ophthalmol. 1975. 80: 1028-42
7. Jakobiec FA, Jones IS, Tannenbaum M. Leiomyoma, an unusual tumor of the orbit. Br J Ophthalmol. 1973. 57: 825-31
8. Lodato GE. Fibro-mioma dell’orbita. Arch Ottal. 1896. 4: 120
9. Merani R, Khannah G, Mann S, Ghabrial R. Orbital leiomyoma: A case report with clinical, radiological and pathological correlation. Clin Exp Ophthalmol. 2005. 33: 408-11
10. Nath K, Shukla BR. Orbital leiomyoma and its origin. Br J Ophthalmol. 1963. 47: 369-71
11. Paluzzi A, Koutourousiou M, Tormenti M, Fernandez-Miranda J, Snyderman C, Gardner P. “Round-the-Clock” surgical access to the orbit. J Neurol Surg Part B Skull Base. 2012. 73: 2
12. Sanborn GE, Valenvuela RE, Green RW. Leiomyoma of the orbit. Am J Ophthalmol. 1979. 87: 371-5
13. Sendul SY, Atilgan CU, Kabukcuoglu F, Demir ST, Guven D. Anterior orbital leiomyoma originating from the supraorbital neurovascular bundle. SAGE Open Med Case Rep. 2017. 5: 2050313X17740991
14. Signorelli F, Anile C, Rigante M, Paludetti G, Pompucci A, Mangiola A. Endoscopic treatment of orbital tumors. World J Clin Cases. 2015. 3: 270-4
15. Wolter RJ. Hemangio-leiomyoma of the orbit. Ear Nose Throat Man. 1965. 44: 42-6