- Neurosurgery Unit, Cheikh Anta Diop University, Fann Teaching Hospital, Avenue Cheikh Anta Diop, Dakar, Senegal.
DOI:10.25259/SNI_148_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Maguette Mbaye, Alioune Badara Thiam, Mohamed Abdoulaye Cissue, Mohameth Faye, S. Y. El hadji Cheikh Ndiaye, Mbaye Thioub, Ndaraw Ndoye, Momar Code Ba, Seydou Boubakar Badiane. Orbital meningocele in two case studies. 23-May-2020;11:119
How to cite this URL: Maguette Mbaye, Alioune Badara Thiam, Mohamed Abdoulaye Cissue, Mohameth Faye, S. Y. El hadji Cheikh Ndiaye, Mbaye Thioub, Ndaraw Ndoye, Momar Code Ba, Seydou Boubakar Badiane. Orbital meningocele in two case studies. 23-May-2020;11:119. Available from: https://surgicalneurologyint.com/surgicalint-articles/10037/
Abstract
Background: Orbital meningocele is a rare congenital malformation characterized by herniation of the meninges into the orbit through a congenital defect in the orbital bones. Much less commonly, it occurs at the site of natural openings (e.g., optic foramen and sphenoidal fissure) or can be attributed to trauma.
Cases Description: We report two patients with progressive proptosis found to have orbital meningoceles, respectively, attributed to congenital and traumatic lesions. The computed tomography scan in one case documented a traumatic orbital bony defect, but in the other case, led the mistaken diagnosis of an arachnoid cyst.
Conclusion: Both patients underwent two operations each to ultimately achieve successful surgical correction of their respective traumatic and congenital orbital meningoceles.
Keywords: Children, Orbital meningocele, Trauma
INTRODUCTION
Primitive orbital meningocele is a rare congenital malformation defined as a herniation of the meninges into the orbit through a congenital or traumatic defect in the orbital bone.[
CASE DESCRIPTION
Case 1
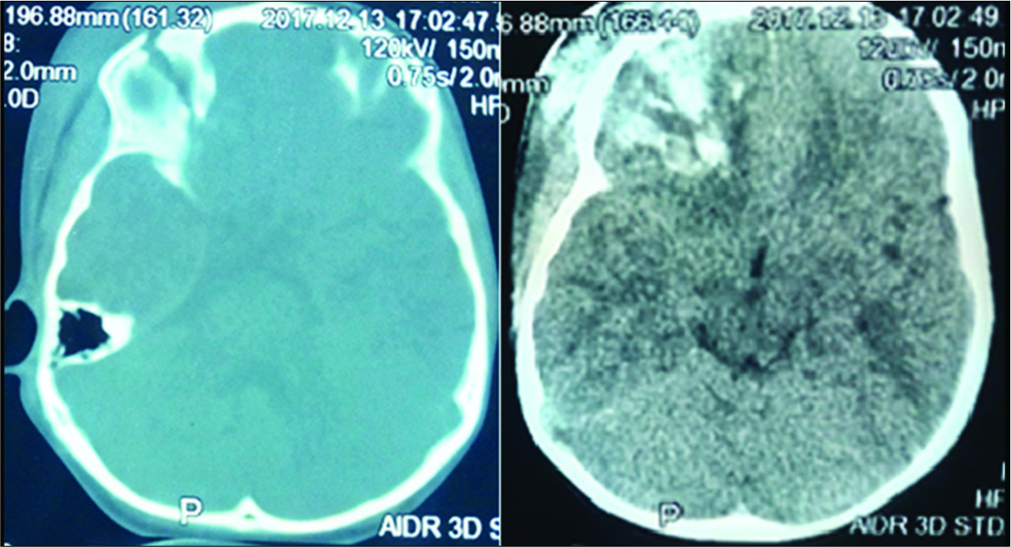
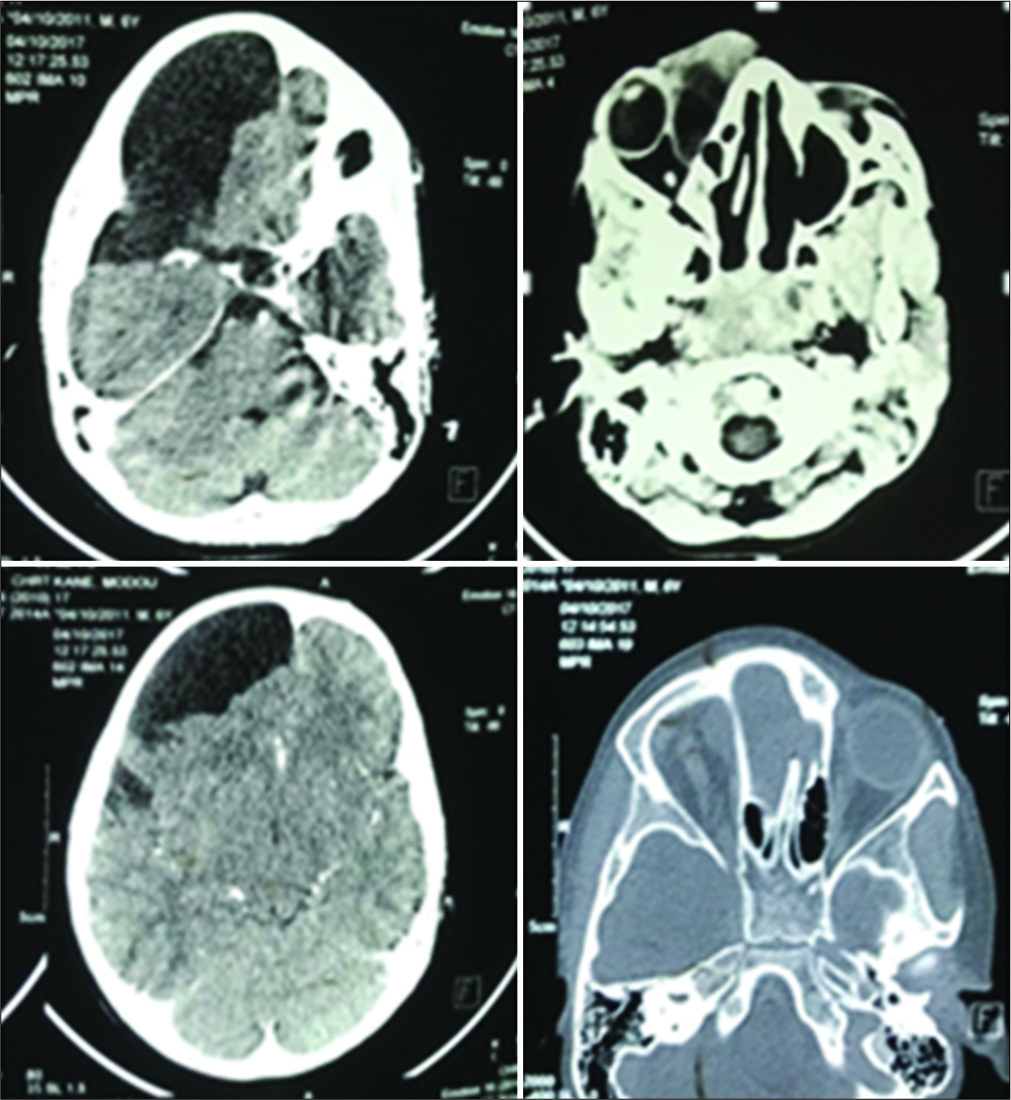
A 3-year-old female sustained a fall resulting, and 1 week later presented with the right orbital swelling. Ten days after the fall, ophthalmology observed persistent swelling; the periorbital tap revealed cerebrospinal fluid (CSF). Two computed tomography (CT) scans were performed 1.5 and 3.5 months after the fall for persistent right periorbital swelling (i.e. the eye remaining closed). The CT studies revealed; (1) a right frontal orbital fracture with parenchymal right frontal brain contusion and an osteodural breach (e.g., displaced fracture of the roof of the right orbit extending to the ipsilateral upper wall/frontal bone) [
Surgery
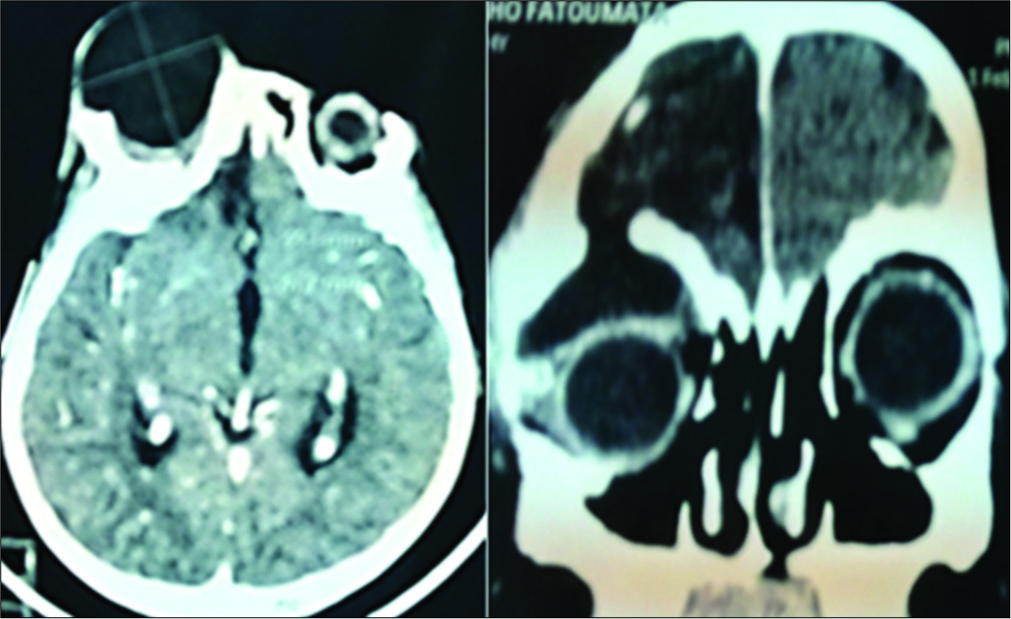
The surgical repair included closure of the meningocele and repair of the fracture utilizing a bone graft to the orbital roof. Postoperatively, she had a persistent CSF leak accompanied by proptosis unresponsive to acetazolamide 250 mg. The postoperative CT scan documented the same findings as recounted above [
Treatment
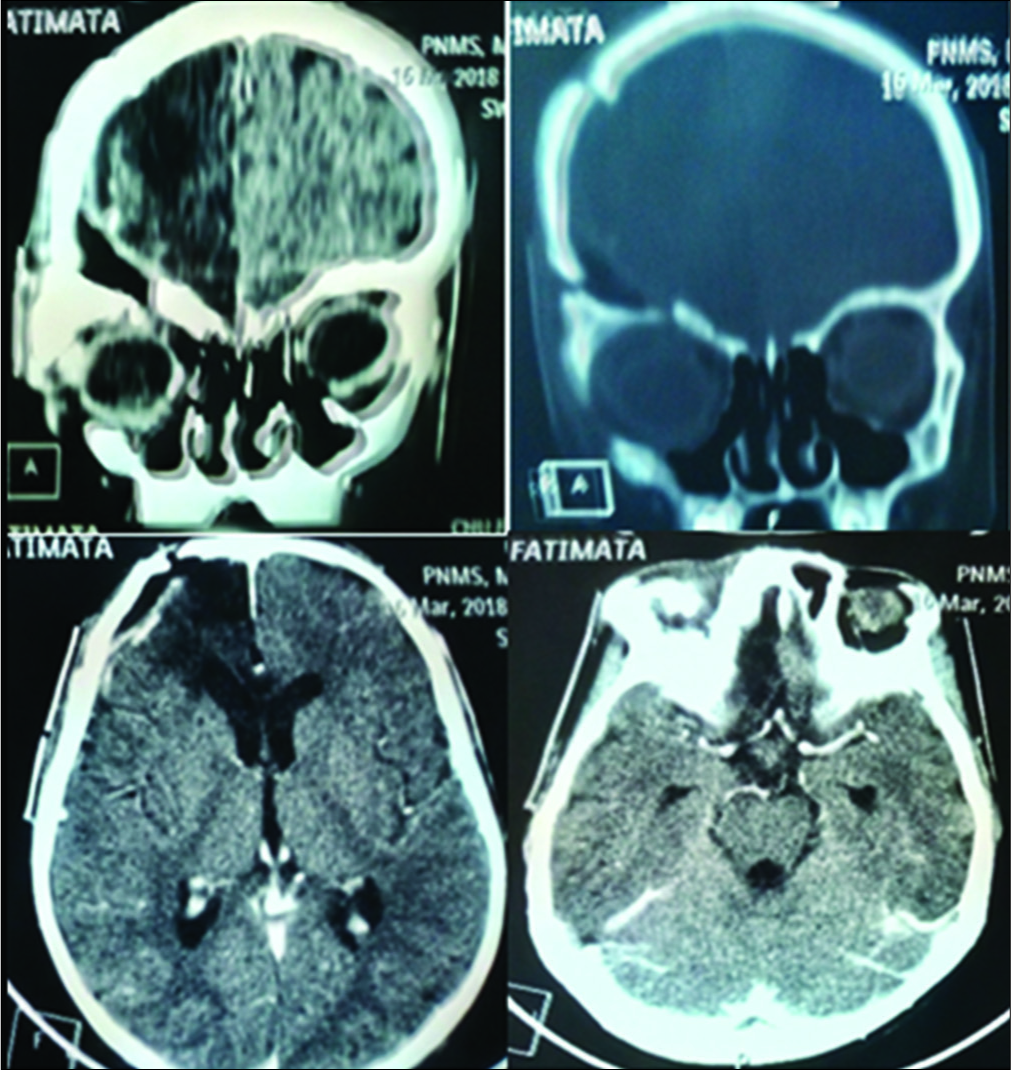
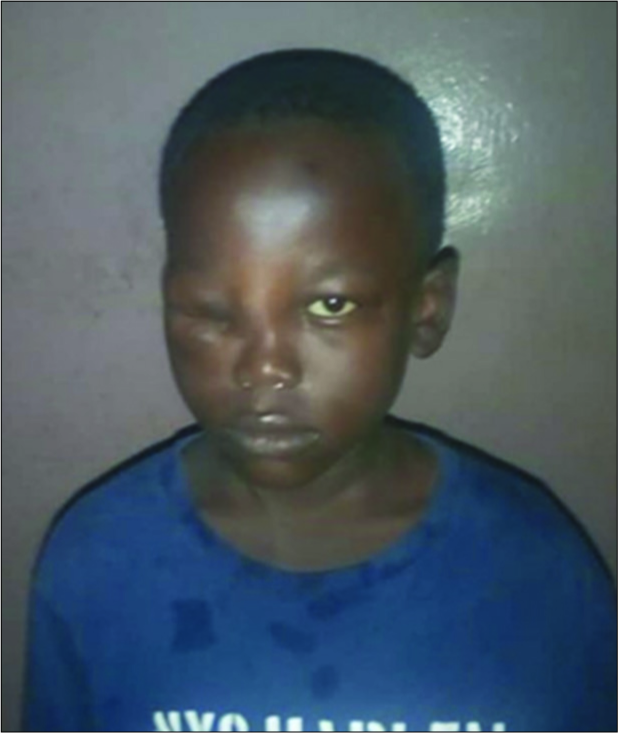
When repeated lumbar punctures failed to resolve the problem, secondary surgery was performed to close the roof of the orbit utilizing abdominal fat. Postoperatively, she developed meningitidis that was appropriately treated with multiple antibiotic. One month later, the meningitis resolved along with her right side proptosis. Further, there was an improvement in the downward gaze/displacement/ ophthalmoplegia [
Case 2
A 7-year-old male presented with a solid right orbital lesion. He had been born with an “inner canthi lesion” extending to the nose and had a “procedure” performed at 1 month of age without resolution of the problem. Six years later, he presented with a solid right eye inner canthus lesion accompanied by increased lacrimation but without any visual loss [
DISCUSSION
Epidemiology
Orbital meningoceles account for between 1 and 1.5% of all meningoceles.[
Delay of management
Early surgical intervention can minimize postoperative morbidity and improve functional and cosmetic results.[
Surgery
For congenital meningoceles, the best treatment is for excision and/ligation of the cyst plus closure of the defect.[
In this report, both patients exhibited postoperative sequelae consisting of 6–12 months of postoperative residual unilateral downward displacement/ophthalmoplegia.[
CONCLUSION
We presented two cases of orbital meningocele; one traumatic and one congenital, where the surgical outcomes could have been improved with earlier diagnosis and treatment.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Badilla J, Dolman PJ. Cerebrospinal fluid leaks complicating orbital or oculoplastic surgery. Arch Ophthalmol. 2007. 125: 1631-4
2. Benharbit M, Rifi LL, El Khamlichi A, Mohcine Z. La méningo-encéphalocèle orbitaire: À propos de 2 cas. J Fr Ophtalmol. 2004. 27: 613-6
3. Connon FV, Austin SJ, Nastri AL. Orbital roof fractures: A clinically based classification and treatment algorithm. Craniomaxillofac Trauma Reconstr. 2015. 8: 198-204
4. Ha AY, Mangham W, Frommer SA, Choi D, Klinge P, Taylor HO. Interdisciplinary management of minimally displaced orbital roof fractures: Delayed pulsatile exophthalmos and orbital encephalocele. Craniomaxillofac Trauma Reconstr. 2017. 10: 11-5
5. Haug RH, Van Sickels JE, Jenkins WS. Demographics and treatment options for orbital roof fractures. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002. 93: 238-46
6. Kim JW, Bae TH, Kim WS, Kim HK. Early reconstruction of orbital roof fractures: Clinical features and treatment outcomes. Arch Plast Surg. 2012. 39: 31-5
7. Mohindra S, Mukherjee KK, Chhabra R, Gupta R. Orbital roof growing fractures: A report of four cases and literature review. Br J Neurosurg. 2006. 20: 420-3
8. Van Rumund A, Verrips A, Verhagen WI. Pulsatile proptosis due to intraorbital meningocele. Front Neurol. 2017. 8: 290-