- Department of Surgery, University of Baghdad, College of Medicine, Baghdad, Iraq
Correspondence Address:
Najah K. Mohammad Department of Surgery, University of Baghdad, College of Medicine, Baghdad, Iraq.
DOI:10.25259/SNI_38_2025
Copyright: © 2025 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Najah K. Mohammad. Orbital tumors: A retrospective analysis of cases from Iraq and orbital anatomical perspectives. 28-Feb-2025;16:62
How to cite this URL: Najah K. Mohammad. Orbital tumors: A retrospective analysis of cases from Iraq and orbital anatomical perspectives. 28-Feb-2025;16:62. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=13424
Abstract
BackgroundWith its vital ocular and adnexal structures, the orbit may be affected by a wide array of neoplasms, including primary, secondary, and metastatic neoplasms. These lesions pose significant diagnostic and therapeutic challenges in view of complex orbital anatomy and overlapping clinical presentations. This study aimed to analyze the epidemiology, clinical features, refractive impacts, and management outcomes of orbital tumors, providing insights to optimize diagnosis and treatment strategies.
MethodsThis study retrospectively analyzes 22 patients who had a presentation of orbital tumors at the Istishari Ophthalmic Eye Hospital between January 2019 and January 2024. Collected data were demographic, clinical, refractive, tumor type, laterality, and management outcome. Advanced imaging studies and histopathological diagnoses confirm the diagnoses. Statistical tests will be applied in assessing the relationship among tumor types, clinical presentations, and refractive changes by means of Analysis of Variance and Chi-square tests.
ResultsCavernous hemangioma was the most prevalent tumor (54.5%), followed by adenoid cystic carcinoma and optic nerve meningioma (13.6% and 9.1%, respectively). Proptosis (31.8%) was the predominant symptom. Significant refractive changes were noted across tumor types (P = 0.012). Lateral orbitotomy was the most common surgical approach (68.2%), with adjuvant therapies utilized in 22.7% of cases. Tumors predominantly affected females (54.5%) and the left orbit (77.3%).
ConclusionOrbital tumors present diverse clinical and refractive manifestations, necessitating individualized, multidisciplinary approaches for effective management. This study underscores the importance of advanced imaging, tailored surgical strategies, and the integration of minimally invasive techniques. Future multicenter studies are needed to validate these findings and enhance therapeutic outcomes.
Keywords: Lateral orbitotomy, Multidisciplinary management, Orbital tumors, Proptosis, Refractive changes
INTRODUCTION
The orbit is a complex anatomic structure that houses the eye and its adnexa, comprising muscles, nerves, blood vessels, and connective tissue. This limited, closed space is very prone to both primary and secondary tumor growth. Orbital tumors encompass a broad category of benign and malignant neoplasms.[
MATERIALS AND METHODS
Study design
This study was a retrospective observational analysis conducted on patients diagnosed with orbital tumors at Istishari Ophthalmic Eye Hospital. The primary objective was to analyze the epidemiological, clinical, and refractive characteristics of orbital tumors and assess the surgical and adjuvant management outcomes. Thus, the study recruited 22 patients diagnosed with orbital tumors between January 2019 and January 2024 based on specific inclusion and exclusion criteria. Besides, the inclusion criteria included confirmed orbital tumors by histopathology and availability of complete clinical, diagnostic, and management data. On the other hand, incomplete records constituted the criteria for exclusion.
Data collection
Clinical and demographic data were extracted from the records of patients with orbital tumors, including age, gender, presenting complaints, tumor type, laterality, and surgical outcomes. In addition, detailed refractive measurements such as intraocular pressure (IOP), spherical power (SPH), cylindrical power (CYL), and orientation of astigmatism were recorded for the affected eye. The study analyzed various variables and parameters: epidemiological variables included age, gender, and tumor laterality; clinical variables encompassed presenting complaints (e.g., proptosis, vision distortion, pain), tumor type, and location; refractive parameters such as IOP, SPH, CYL, and astigmatism orientation were assessed to determine the impact of the tumor type on ocular parameters; and management outcomes focused on the types of surgical approaches and the use of adjuvant therapies such as chemotherapy and radiotherapy.
Diagnostic and therapeutic approaches
The general comprehensive ophthalmologic examination of patients with a diagnosis of an orbital tumor condition includes imaging studies such as CT and MRI for tumor extent, location, invasion possibility determination, and histopathological diagnosis on biopsy specimen for the definitive diagnosis of tumor types. Surgical interventions included lateral orbitotomy, enucleation, and endoscopic sinus surgery, which were selected according to the type and location of the tumor. Besides, adjuvant therapies, including chemotherapy and radiotherapy, were performed in cases of malignant or aggressive tumors.
Statistical analysis
Descriptive and inferential statistical analyses were conducted using the Statistical Package for the Social Sciences software to evaluate the data from patients with orbital tumors. Descriptive statistics included the calculation of frequencies, percentages, means, medians, and standard deviations (SDs) for demographic, clinical, and refractive data. The Chi-square test was utilized to determine associations between categorical variables, such as the distribution of gender across different tumor types and main complaints. Analysis of Variance (ANOVA) was applied to compare refractive parameters (e.g., SPH, CYL) across various tumor types. A significance threshold was set, where a p-value of less than 0.05 was considered statistically significant.
Ethical considerations
The protocol was in accordance with the principles of the Declaration of Helsinki. Patient confidentiality was guaranteed by anonymizing the data.
RESULTS
Epidemiological analysis
Among patients with orbital tumors, females comprised 54.5% (n = 12) and males 45.5% (n = 10), indicating a slight female predominance. The mean age of patients was 49 years (SD 16.4), with a wide range spanning from 5 to 73 years and a median age of 49 years [
Clinical presentations
Proptosis was the most common complaint, reported by 31.8% of patients (n = 7). Other symptoms included vision distortion and mass (both 22.7%, n = 5 each), red eye (13.6%, n = 3), and eye pain (9.1%, n = 2).
Tumor types
Cavernous hemangioma is the most commonly observed tumor, accounting for 54.5% (n = 12). Adenoid cystic carcinoma constitutes 13.6% or n = 3. The number of cases constituted optic nerve meningioma to the tune of 9.1% n = 2. Choroidal melanoma had an occurrence to the extent of 9.1%, that is, n = 2. Other miscellaneous rare tumors include lymphoma 4.5% or n = 1, and capillary hemangioma was also of similar occurrence; a further type of sinonasal carcinoma amounted to the remaining 4.5%, n = 1, which is reported as given in
Laterality
Most tumors affected the left eye (77.3%, n = 17), whereas the right eye was involved in 22.7% (n = 5) of cases.
Surgical management
Lateral orbitotomy was the most common surgical approach, performed in 68.2% (n = 15) of cases. Other procedures included biopsy (13.6%, n = 3), enucleation (9.1%, n = 2), endoscopic sinus surgery (4.5%, n = 1), and observation (4.5%, n = 1).
Adjuvant therapy
Chemotherapy and radiotherapy were utilized in 22.7% (n = 5) of cases. Oral β-blockers were used in 4.5% (n = 1) of cases, and 72.7% (n = 16) did not require adjuvant therapy [
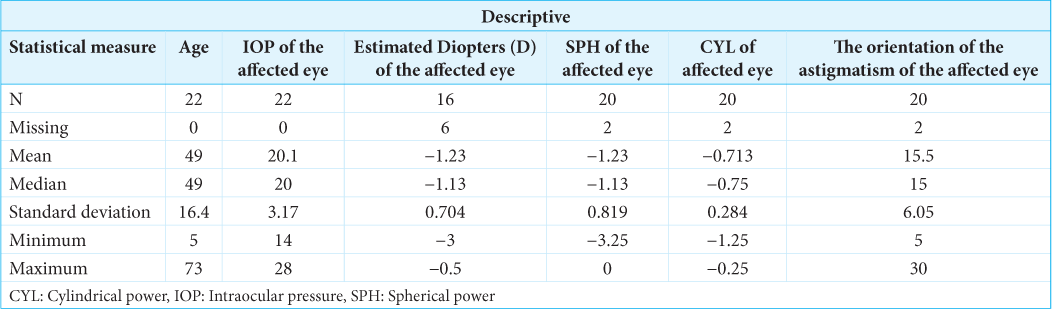
Descriptive statistical profile of orbital tumor cases
The mean IOP of the affected eye was 20.1 mmHg, with an SD of 3.17 mmHg, ranging from 14 mmHg to 28 mmHg and a median value of 20 mmHg. Regarding refractive characteristics, the mean refractive error was −1.23 D (SD 0.704), ranging from −3 D to −0.5 D with a median of −1.13 D. The mean SPH was also −1.23 D (SD 0.819), ranging from −3.25 D to 0 D, with a median of −1.13 D. The mean CYL was −0.713 D (SD 0.284), ranging from −1.25 D to −0.25 D, with a median of −0.75 D. The mean orientation of astigmatism was 15.5° (SD 6.05°), ranging from 5° to 30°, with a median of 15° [
ANOVA for clinical and refractive parameters across tumor types
The ANOVA results demonstrated that IOP showed no significant difference across tumor types (F = 1.71, P = 0.186), indicating that IOP is not influenced by tumor type [
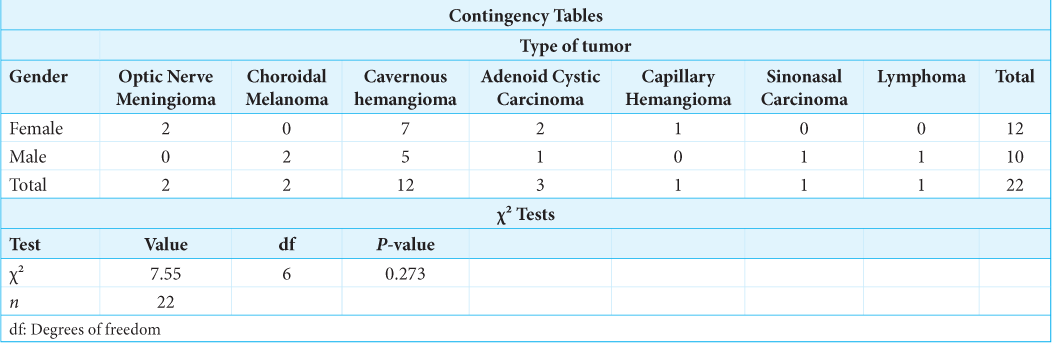
Gender distribution across tumor types
This analysis of sex distribution showed that in the case of cavernous hemangioma, there was a predominance of females (n = 7), while choroidal melanoma, sinonasal carcinoma, and lymphoma were found to affect more males, with one case each. Optic nerve meningioma was found only in females (n = 2). However, according to the Chi-square test, no significant association was found between gender and tumor type (χ2 = 7.55, df = 6, P = 0.273) [
Main complaints across tumor types
The statistical analysis of main complaints revealed that proptosis was most commonly associated with cavernous hemangioma (n = 4), while vision distortion occurred in cases of optic nerve meningioma (n = 1), choroidal melanoma (n = 1), and cavernous hemangioma (n = 2). Mass presentation was frequently observed in cavernous hemangioma (n = 4) and adenoid cystic carcinoma (n = 1), whereas eye pain was relatively rare, reported only in cases of cavernous hemangioma (n = 1) and adenoid cystic carcinoma (n = 1). However, the Chi-square test indicated no statistically significant association between main complaints and tumor type (χ2 = 20.9, df = 24, P = 0.644) [
DISCUSSION
In our study, females represented 54.5% of cases, with cavernous hemangioma being predominantly seen in women. This gender distribution is consistent with findings from prior studies, such as Demirci et al. (2002), which reported a higher prevalence of benign orbital tumors, including cavernous hemangioma, in females.[
The exclusive occurrence of optic nerve meningiomas in females in our study may reflect the known higher incidence of meningiomas in women, possibly linked to hormonal influences.[
CONCLUSION
The information obtained from the in-depth study of the epidemiology, clinical presentation, refractive impact, and outcome of orbital tumors revealed the majority as benign ones, with predominant involvement by the benign tumor being cavernous hemangioma, hence providing significant management approaches both at diagnosis and in the treatment process. Proptosis and refractive changes feature significantly as part of their important clinical manifestations, while the surgical landmark involves a lateral orbitotomy approach. Variations in tumor types, demographics, and clinical presentations underline the necessity for a multidisciplinary approach to optimize diagnosis and management. Future research with larger, multicenter cohorts is essential to validate these findings and improve patient outcomes.
Ethical approval
Institutional Review Board approval is not required as it was a retrospective observational analysis. The protocol was in accordance with the principles of the Declaration of Helsinki.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Arrivi G, Specchia M, Pilozzi E, Rinzivillo M, Caruso D, Santangeli C. Diagnostic and therapeutic management of primary orbital neuroendocrine tumors (NETs): Systematic literature review and clinical case presentation. Biomedicines. 2024. 12: 379
2. Bedell M, Naous R. Primary osseous tumors of the orbit. Virch Arch. 2024. p. Advance online publication
3. Bonham J, Ginat DT, Freitag SK, editors. Imaging after orbital and intraocular oncology therapies. Post-treatment imaging of the orbit. Berlin, Heidelberg: Springer Berlin Heidelberg; 2014. p. 171-200
4. Caballero-García J, Aparicio-García C, Linares-Benavides YJ, López-Sánchez M, Abreu-Perdomo FA, Huanca-Amaru J. Minimally invasive 360-degree approach to intraconal orbital tumors. Am J Ophthalmol. 2021. 224: 301-9
5. Demirci H, Shields CL, Shields JA, Honavar SG, Mercado GJ, Tovilla JC. Orbital tumors in the older adult population. Ophthalmology. 2002. 109: 243-8
6. Dikshit P, Nandan M, Balachandar D, Jaiswal AK, Behari S. Orbital tumors: Current neurosurgical perspectives. Int J Neurooncol. 2021. 4: S78-91
7. El-Habashy DM. 971P Clinical and pathological characteristics of orbital tumours in patients diagnosed at the United States. Ann Oncol. 2020. 31: S683
8. Goldberg RA, Rootman J, Cline RA. Tumors metastatic to the orbit: A changing picture. Survey Ophthalmol. 1990. 35: 1-24
9. Luzzi S, Zoia C, Rampini AD, Elia A, Del Maestro M, Carnevale S. Lateral transorbital neuroendoscopic approach for intraconal meningioma of the orbital apex: Technical nuances and literature review. World Neurosurg. 2019. 131: 10-7
10. Lystratenko OI, Kardash AM, Lystratenko DO, Vashchenko AV, Smyrnova OF. Diagnosis and surgical treatment of orbital tumors of various localizations and histostructures. Gen Surg. 2019. 1: 1015
11. Markowski J, Jagosz-Kandziora E, Likus W, Pająk J, MrukwaKominek E, Paluch J. Primary orbital tumors: A review of 122 cases during a 23-year period: a histo-clinical study in material from the ENT Department of the Medical University of Silesia. Med Sci Monit. 2014. 20: 988-94
12. Nguyen CP, An J, Fox L, Hicks RJ, Li S. MR and CT imaging of orbital tumors. Contemp Diagn Radiol. 2014. 37: 1-7
13. Reshef ER, Bleier BS, Freitag SK. The endoscopic transnasal approach to orbital tumors: A review. Semin Ophthalmol. 2021. 36: 232-40
14. Rizvi SA, Gupta Y, Gupta M. Surgical treatment and histopathological analysis of proptosis. Nepal J Ophthalmol. 2010. 2: 31-4
15. Sa HS, Seo JW, Kang S. Upper fornix approach combined with a superior lateral cantholysis: A minimally invasive approach to the superonasal intraconal space. Jpn J Ophthalmol. 2017. 61: 361-7
16. Zoli M, Sollini G, Milanese L, La Corte E, Rustici A, Guaraldi F. Endoscopic approaches to orbital lesions: Case series and systematic literature review. J Neurosurg. 2020. 134: 608-20