- Department of Neurosurgery, Children's Hospital ‘Aghia Sofia’, Athens, Greece
- Department of Neurosurgery, University of Athens Medical School, “Evangelismos” General Hospital, Athens, Greece
- Department of Imaging, Children's Hospital “Aghia Sophia”, Athens, Greece
- Department of Neurosurgery, G. Gennimatas General Hospital, Athens, Greece
Correspondence Address:
Marios S. Themistocleous
Department of Neurosurgery, Children's Hospital ‘Aghia Sofia’, Athens, Greece
DOI:10.4103/sni.sni_394_17
Copyright: © 2018 Surgical Neurology International This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.How to cite this article: Eleftherios Neromyliotis, Dimitrios Giakoumettis, Evangelos Drosos, Ioannis Nikas, Alexios Blionas, George Sfakianos, Marios S. Themistocleous. Pediatric infratentorial subdural empyema: A case report. 24-May-2018;9:104
How to cite this URL: Eleftherios Neromyliotis, Dimitrios Giakoumettis, Evangelos Drosos, Ioannis Nikas, Alexios Blionas, George Sfakianos, Marios S. Themistocleous. Pediatric infratentorial subdural empyema: A case report. 24-May-2018;9:104. Available from: http://surgicalneurologyint.com/surgicalint-articles/pediatric-infratentorial-subdural-empyema-a-case-report/
Abstract
Background:Infratentorial subdural empyemas in children are extremely rare and potentially lethal intracranial infections. Delay in diagnosis and therapy is associated with increased morbidity and mortality.
Case Description:A 4-year-old boy presented with cerebellar signs following a failed treatment of otitis media. Imaging studies revealed a subdural empyema and left transverse and sigmoid sinus thrombosis. The empyema was evacuated operatively and antibiotic treatment was initiated and administered for 6 weeks. The patient recovered fully and was discharged 4 weeks following the evacuation of the empyema.
Conclusion:While prompt identification and treatment of subdural infratentorial empyemas are crucial for favorable outcomes, their diagnosis in children might be initially missed. This is, in part because they are so rare and in part, because imaging artifacts arising from the complex posterior fossa anatomy may obscure their presence in the computer tomography (CT) scan. Therefore, high level of suspicion is necessary, given the appropriate history and clinical presentation. In children, this is a recent history of protracted otitis media and central nervous system symptomatology—cerebellar or other.
Keywords: Child, empyema, infratentorial, pediatric, subdural
INTRODUCTION
A subdural empyema is defined as the focal intracranial collection of purulent material between the dura and the arachnoid mater. Most often, it presents as a complication of other pathologies such as sinusitis, mastoiditis, and bacterial meningitis or posttraumatically.[
CASE REPORT
A 4-year-old boy presented to the pediatric emergency department with symptoms of cerebellar ataxia and gait disturbances. Sixteen days prior to that, his parents had consulted a primary care physician due to left earache and fever. No purulent discharge from the ear was evident at the time. Then, the patient was diagnosed with otitis media and was prescribed oral amoxicillin-clavulanic acid. Due to symptoms persistence, treatment was subsequently switched to oral cefuroxime.
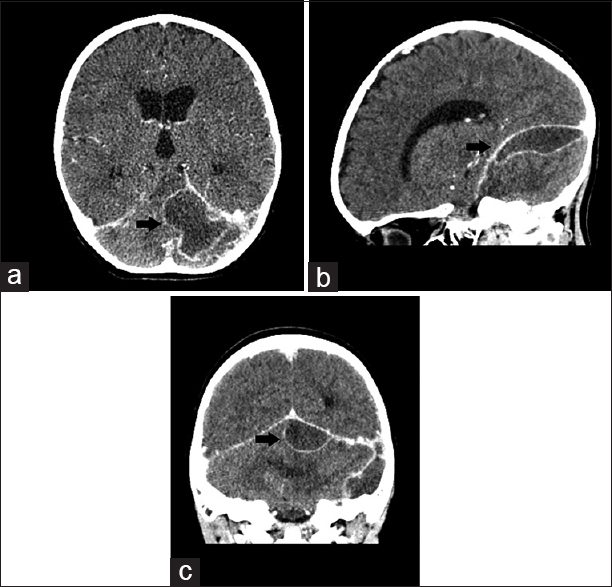
Upon presentation to our emergency department, a complete blood count showed leukocytosis and neutrophilia. The prominence of cerebellar symptoms raised suspicion for an intracranial pathology and thus an emergency contrast-enhanced CT scan was performed. The scan revealed a multilobular cystic lesion with peripheral contrast enhancement, located in the subdural space of the posterior fossa, in contact with the tentorium cerebelli superiorly [
Intravenous antibiotic treatment with piperacillin-tazobactam and teicoplanin was initiated. After 4 days the patient had no fever, no neurological deficits, and was ambulatory. Follow-up MRI scan documented the successful evacuation of the empyema and subsiding inflammation [
DISCUSSION
Infratentorial subdural empyema is an extremely rare clinical entity both in children and in adults. Apart from the Madhugiri et al.[
Our patient presented with cerebellar signs and a recent history of otitis media. In the Madhugiri series,[
The primary cause of infratentorial empyemas is a complicated otogenic infection. This is the case for our patient who underwent a prolonged antibiotic treatment for an otitis media infection that proved resistant. The same course was described in 19 out of 22 Nathoo's[
In terms of diagnosis, high clinical suspicion is the first step. Despite the greater accuracy of MRI scans in diagnosing intracranial pathologies, the initial imaging study of choice is CT scan, due to its speed and availability.[
The culture of the purulent collection we obtained intraoperatively did not identify any pathogens. This is a frequently encountered mischief in subdural empyemas. Sterile collections are reported in the Nathoo[
Finally, the course of our patient was complicated with left transverse and sigmoid sinus thrombosis. Sinus thrombosis was encountered in one of the Madhugiri[
Infratentorial subdural empyemas compared to the more common supratentorial variants are associated with higher mortality. This has been attributed to delays in diagnosis and treatment.[
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Agrawal A, Timothy J, Pandit L, Shetty L, Shetty J. A review of subdural empyema and its management. Infect Dis Clin Pract. 2007. 15: 149-53
2. Borovich B, Johnston E, Spagnuolo E. Infratentorial subdural empyema: Clinical and computerized tomography findings. Report of three cases. J Neurosurg. 1990. 72: 299-301
3. Calfee DP, Wispelwey B. Brain abscess, subdural empyema, and intracranial epidural abscess. Curr Infect Dis Rep. 1999. 1: 166-71
4. Gupta A, Karanth SS, Raja A. Infratentorial subdural empyemas mimicking pyogenic meningitis. J Neurosci Rural Pract. 2013. 4: 213-5
5. Kanev PM, Salazar JC. Unusual CNS infection from a subtorcular dermal sinus. Acta Paediatr. 2010. 99: 627-9
6. Madhugiri VS, Sastri BV, Bhagavatula ID, Sampath S, Chandramouli BA, Pandey P. Posterior fossa subdural empyema in children – management and outcome. Childs Nerv Syst. 2011. 27: 137-44
7. Morgan DW, Williams B. Posterior fossa subdural empyema. Brain. 1985. 108: 983-92
8. Nathoo N, Nadvi SS, van Dellen JR. Infratentorial empyema: Analysis of 22 cases. Neurosurgery. 1997. 41: 1263-
9. Osman Farah J, Kandasamy J, May P, Buxton N, Mallucci C. Subdural empyema secondary to sinus infection in children. Childs Nerv Syst. 2009. 25: 199-205
10. Renaudin JW, Frazee J. Subdural empyema – importance of early diagnosis. Neurosurgery. 1980. 7: 477-9
11. Sahjpaul RL, Lee DH. Infratentorial subdural empyema, pituitary abscess, and septic cavernous sinus thrombophlebitis secondary to paranasal sinusitis: Case report. Neurosurgery. 1999. 44: 864-
12. Sengul G. Infratentorial subdural empyema. Turk Neurosurg. 2009. 19: 200-2
13. Taha MM, Hassanain S. Subtentorial subdural empyema: Report of two cases and review of the literatures. Turk Neurosurg. 2011. 21: 669-673
14. van de Beek D, Campeau NG, Wijdicks EF. The clinical challenge of recognizing infratentorial empyema. Neurology. 2007. 69: 477-81