- Department of Neurosurgery, Global Neurosciences Institute, Philadelphia, Pennsylvania, United States.
- Department of Neurosurgery, Medical College of Wisconsin, Milwaukee, Wisconsin, United States.
- Drexel Neurosciences Institute, Drexel University School of Medicine, Philadelphia, Pennsylvania, United States.
Correspondence Address:
Hirad S. Hedayat, Department of Neurosurgery, Medical College of Wisconsin, 8701 W Watertown Plank Rd, Milwaukee - 53226, Wisconsin, United States.
DOI:10.25259/SNI_136_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Randall Faber1, Christina N. Feller2, Natalie Gofman1, John Fletcher3, Hirad S. Hedayat2. Pediatric middle meningeal artery embolization for chronic subdural hematoma: A case report. 25-May-2021;12:239
How to cite this URL: Randall Faber1, Christina N. Feller2, Natalie Gofman1, John Fletcher3, Hirad S. Hedayat2. Pediatric middle meningeal artery embolization for chronic subdural hematoma: A case report. 25-May-2021;12:239. Available from: https://surgicalneurologyint.com/surgicalint-articles/10822/
Abstract
Background: The most common neuroradiological finding in pediatric nonaccidental trauma (NAT) is subdural hematoma (SDH). Management options for pediatric SDH range from conservative clinical surveillance to craniotomy or decompressive craniectomy. The middle meningeal artery (MMA) indirectly feeds the hematoma; thus, MMA embolization is an alternative or adjunct to current surgical treatments in adults. Herein, we present, to the best of our knowledge, the first reported case of successful MMA embolization in a pediatric patient as an adjunct to current standard treatment for chronic SDH (cSDH).
Case Description: An 18-month-old male with a history of NAT presented at 5 months of age with an acute right parietal skull fracture and bilateral SDH treated with burr hole drainage. He was lost to follow-up until 15 months of age with an increased head circumference and new dysconjugate gaze. Imaging revealed a right-sided cSDH and underwent craniotomy. Six-week follow-up revealed significant improvement in the SDH but cSDH remained at the periphery of the craniotomy’s reach. The patient symptoms continued. The right-sided MMA embolization was offered as option to avoid repeat craniotomy. Follow-up CTs at 2 weeks, 3 months, and 6 months postprocedure revealed decrease of cSDH size and density. At 8-month follow-up, the patient continued to meet developmental milestones with near resolution of his dysconjugate gaze.
Conclusion: This case report details the first successful use of MMA embolization in the treatment of pediatric cSDH as an adjunct to standard treatment. Further investigation of MMA embolization in pediatrics should be made to expand options available for cSDH in this patient population.
Keywords: Chronic SDH, MMA embolization, Pediatric neurotrauma
INTRODUCTION
The most common neuroradiological finding in pediatric abusive head trauma is subdural hematoma (SDH).[
The middle meningeal artery (MMA) has been found to provide vascular supply to capillaries that feed hematoma and membrane formation.[
CASE PRESENTATION
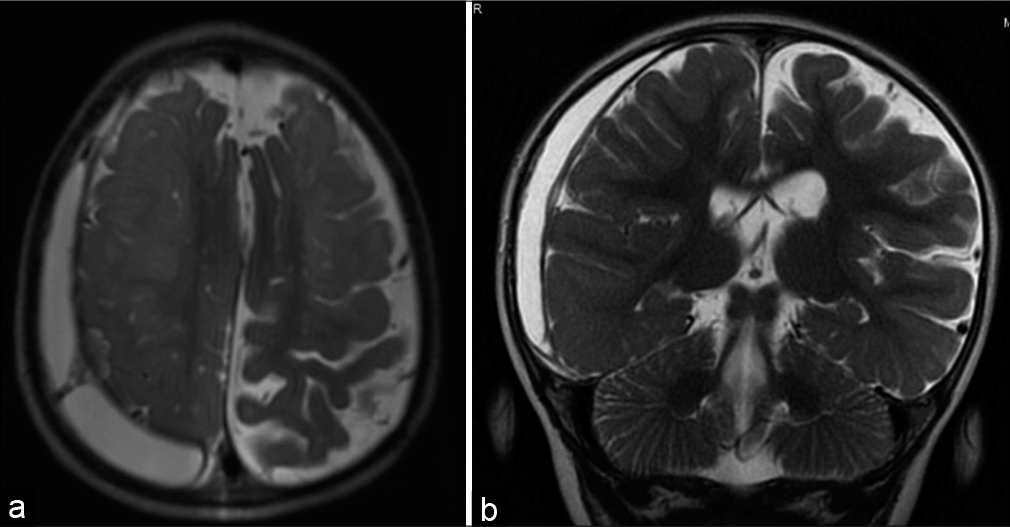
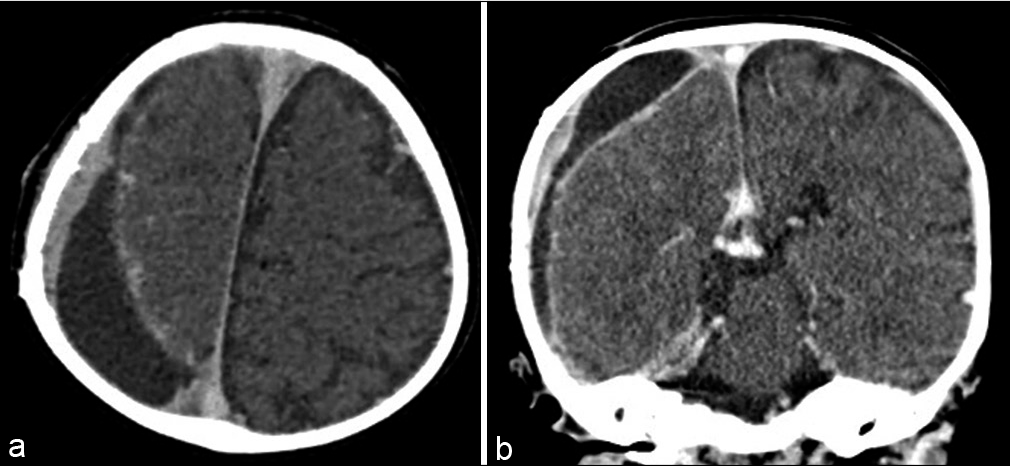
An 18-month-old with a history of nonaccidental trauma (NAT) originally presented at 5 months of age with an acute right parietal skull fracture and bilateral SDH treated with burr hole drainage [
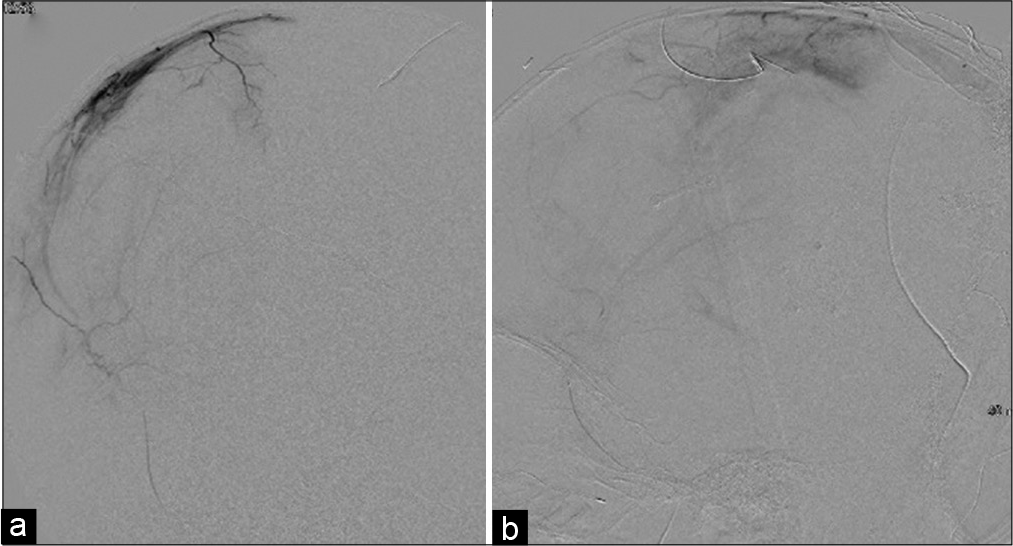
The right-sided MMA embolization was offered as option to avoid repeat craniotomy as his dysconjugate gaze did not resolve during follow-up. At 18 months of age, under general anesthesia, with neurological monitoring, vascular access was achieved using a micropuncture technique in the left femoral artery and the 4-French Berenstein catheter was used. The right MMA was selectively catheterized [
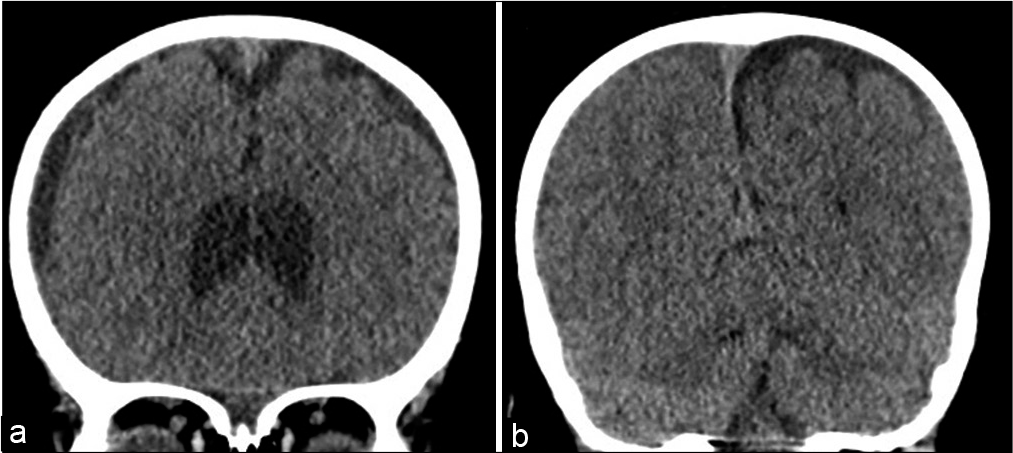
Follow-up CTs were performed at 2 weeks, 3 months, and 6 months postprocedure [
DISCUSSION
NAT is the leading cause of fatal head injuries in children younger than 2 years of age and responsible for 53% of serious or fatal traumatic brain injury cases.[
cSDH describes a serosanguinous, petroleum, or “crankcase-like” fluid collection occasionally loculated within neomembranes. After the initial occurrence of SDH, an inflammatory response occurs with proliferation of dural border cells, fibroblasts, and inflammatory cells resulting in the formation of a membrane around the SDH.[
The management options for SDH in the pediatric population are varied and range from conservative clinical surveillance (nonsurgical management) to subdural punctures, external subdural drainage, subcutaneous reservoirs, subduralsubgaleal shunts, subdural-peritoneal shunts, craniotomy, and decompressive craniectomy.[
Our patient was treated initially with bilateral burr hole drainage without drain placement and experienced resolution of the left SDH. The development of a cSDH with membranes on the right may be related to the parietal skull fracture and acute on chronic hemorrhage secondary to additional NAT. Unfortunately, he was lost to follow-up for several months after his burr hole drainage and presented to his pediatrician with enlarging head circumference and exotropia of the left eye, an oft noted clinical scenario,[
CONCLUSION
The use of middle meningeal artery embolization for treatment of our patient’s chronic subdural hematoma resulted in significant size and density reduction of the cSDH on imaging and almost full resolution of clinical symptoms. To the best of our knowledge, this report details the first successful use of MMA embolization in the treatment of pediatric cSDH as an adjunct to standard treatment. Further investigation of the less invasive technique of MMA embolization in pediatrics should be made to expand options available for cSDH in this patient population.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
I want to first thank the family and patient described in this case report for allowing us to write about their case to allow increased awareness and education about the treatment of chronic subdural hematomas.
I want to also thank both Global Neurosciences Institute and Drexel University School of Medicine for allowing the creation and completion of this case through the use of a novel technique.
Finally, I would like to thank all those involved in the revision and submitting process at the Medical College of Wisconsin.
References
1. Choudhary AK, Servaes S, Slovis TL, Palusci VJ, Hedlund GL, Narang SK. Consensus statement on abusive head trauma in infants and young children. Pediatr Radiol. 2018. 48: 1048-65
2. Ducruet AF, Grobelny BT, Zacharia BE, Hickman ZL, DeRosa PL, Andersen KN. The surgical management of chronic subdural hematoma. Neurosurg Rev. 2012. 35: 155-69
3. Feldman KW, Sugar NF, Browd SR. Initial clinical presentation of children with acute and chronic versus acute subdural hemorrhage resulting from abusive head trauma. J Neurosurg Pediatr. 2015. 16: 177-85
4. Hedlund G, Kleinman PK.editors. Abusive head trauma: Extraaxial hemorrhage and nonhemic collections. Diagnostic Imaging of Child Abuse. Cambridge: Cambridge University Press; 2015. p. 394-452
5. Link TW, Boddu S, Paine SM, Kamel H, Knopman J. Middle meningeal artery embolization for chronic subdural hematoma: A series of 60 cases. Neurosurgery. 2019. 85: 801-7
6. Melo JR, Di Rocco F, Bourgeois M, Puget S, Blauwblomme T, Sainte-Rose C. Surgical options for treatment of traumatic subdural hematomas in children younger than 2 years of age. J Neurosurg Pediatr. 2014. 13: 456-61
7. Orman G, Kralik SF, Meoded A, Desai N, Risen S, Huisman TA. MRI findings in pediatric abusive head trauma: A review. J Neuroimaging. 2020. 30: 15-27
8. Rovlias A, Theodoropoulos S, Papoutsakis D. Chronic subdural hematoma: Surgical management and outcome in 986 cases: A classification and regression tree approach. Surg Neurol Int. 2015. 6: 127
9. Srivatsan A, Mohanty A, Nascimento FA, Hafeez MU, Srinivasan VM, Thomas A. Middle meningeal artery embolization for chronic subdural hematoma: Meta-analysis and systematic review. World Neurosurg. 2019. 122: 613-9
10. Wittschieber D, Karger B, Pfeiffer H, Hahnemann ML. Understanding subdural collections in pediatric abusive head trauma. AJNR Am J Neuroradiol. 2019. 40: 388-95