- Department of Orthopedic Surgery, Akita University Graduate School of Medicine, Hondo, Japan.
- Department of Orthopedic Surgery, Akita Red Cross Hospital, Akita, Japan.
- Department of Orthopedic Surgery, Akita Prefectural Center on Development and Disability, Akita, Japan.
Correspondence Address:
Ryo Shoji
Department of Orthopedic Surgery, Akita University Graduate School of Medicine, Hondo, Japan.
DOI:10.25259/SNI_908_2020
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Ryo Shoji1, Naohisa Miyakoshi1, Michio Hongo1, Yuji Kasukawa1, Yoshinori Ishikawa1, Daisuke Kudo1, Noriyuki Ishikawa2, Yuji Hatakeyama2, Akiko Misawa3, Hitoshi Sakamoto3, Yoichi Shimada1. Pediatric spinal infection with epidural abscess: A report of two cases. 08-Apr-2021;12:139
How to cite this URL: Ryo Shoji1, Naohisa Miyakoshi1, Michio Hongo1, Yuji Kasukawa1, Yoshinori Ishikawa1, Daisuke Kudo1, Noriyuki Ishikawa2, Yuji Hatakeyama2, Akiko Misawa3, Hitoshi Sakamoto3, Yoichi Shimada1. Pediatric spinal infection with epidural abscess: A report of two cases. 08-Apr-2021;12:139. Available from: https://surgicalneurologyint.com/surgicalint-articles/10704/
Abstract
Background: Pediatric spinal infections are rare and often accompanied by abscesses. Delayed diagnosis commonly leads to a poor neurological prognosis, emphasizing the need for early diagnosis and treatment.
Case Description: We report on two cases of spinal infection; one in a 5-year-old boy with a T8-11 epidural abscess and one in a 10-year-old boy with an L5-S1 epidural abscess. Both cases improved with conservative therapy.
Conclusion: Early magnetic resonance imaging diagnosis and systemic treatment in collaboration with pediatricians are key factors in the successful management of children with spinal infections.
Keywords: Epidural abscess, Magnetic resonance imaging, Pediatrics
INTRODUCTION
Spinal infections including epidural abscesses are rare in children and thus not often encountered in routine clinical practice.[
CASE PRESENTATION
Case 1
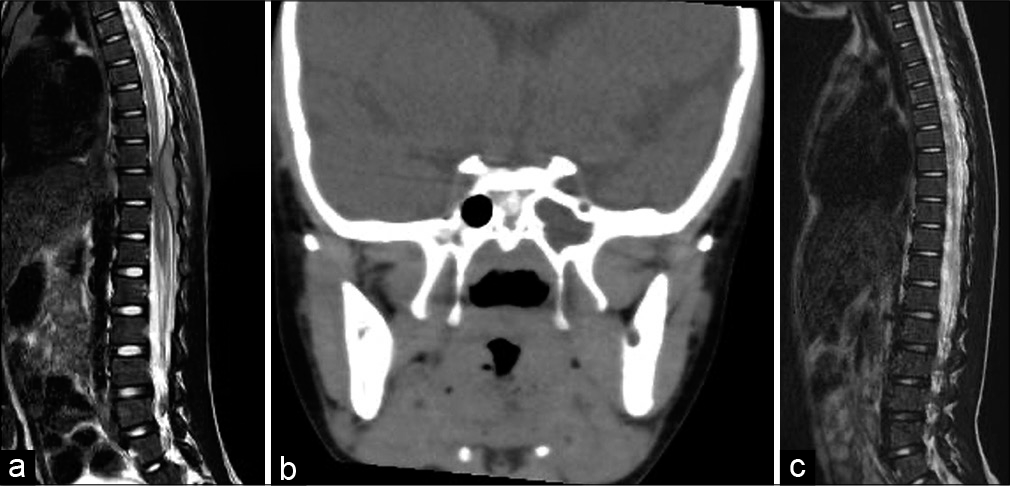
A 5-year-old boy attended another hospital complaining of a 1-month history of worsening back pain and fever. After 1 month, his symptoms had not improved and he attended our facility. On physical and neurological examination, he had a normal level of consciousness, a body temperature of 38.6°C, and no neurological deficits. Blood tests revealed a white blood cell (WBC) count of 12,900/µL, hemoglobin 11.7 g/dL, platelet 30.1 × 104/µL, and C-reactive protein (CRP) 10.83 mg/dL. T2-weighted images of contrast-enhanced MRI revealed a mild hyperintense space-occupying lesion with a ring-shaped contrast effect located epidurally on the dorsal side of the T8-11 level [
Figure 1:
(a) Sagittal T2-weighted magnetic resonance image (MRI) on admission showing mild hyperintensity on the dorsal side of the epidural lining at T8-11. (b) Coronal computed tomography image showing sinusoidal abscess. (c) Sagittal T2-weighted MRI on day 14 showing almost complete resolution of the epidural abscess.
Case 2
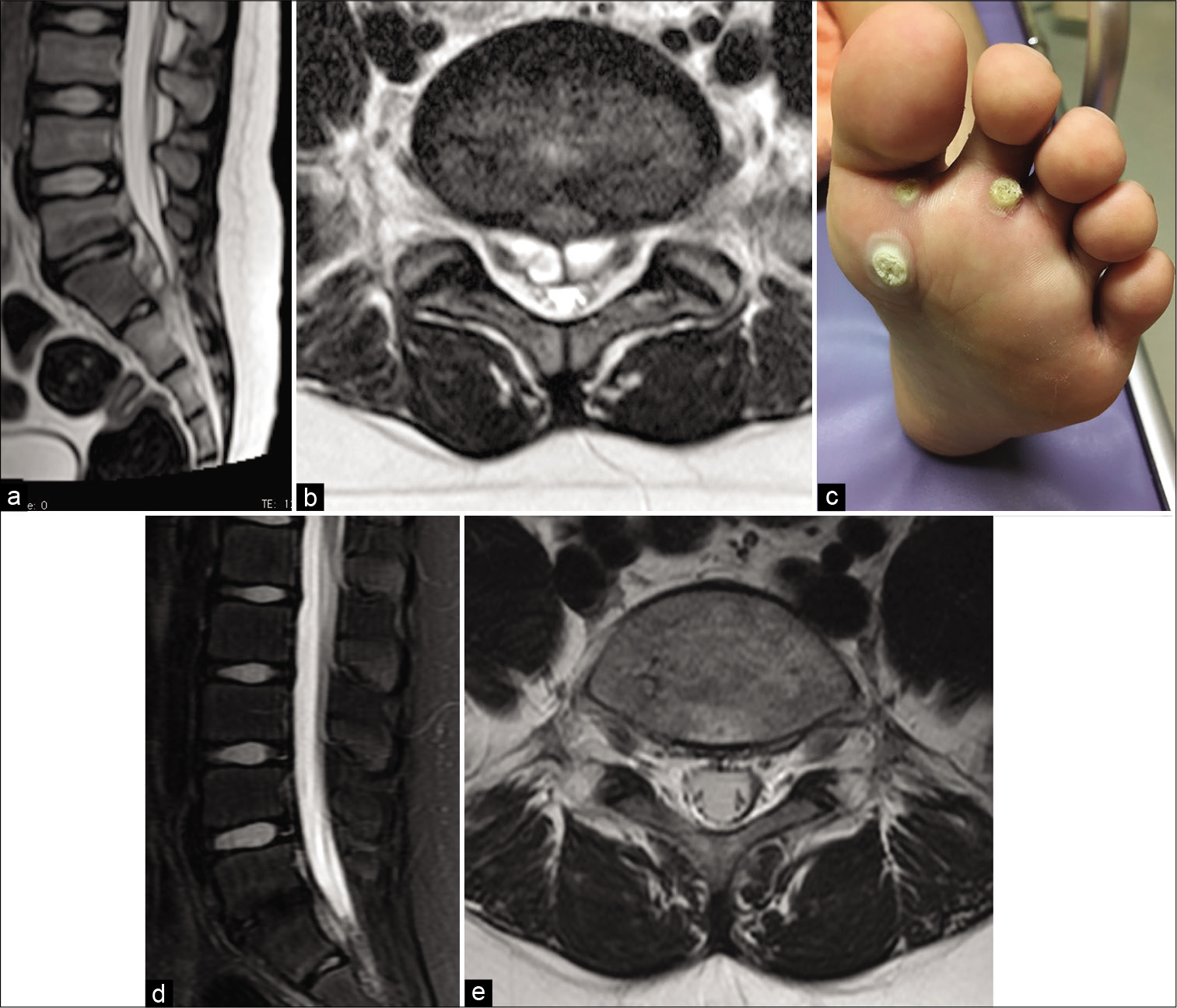
A 10-year-old boy presented to a regional hospital with back pain. His backache continued for 3 weeks, and after developing a fever, he visited another hospital. Blood tests showed high inflammatory markers and the patient was referred to our hospital. On physical examination, his level of consciousness was normal and he had a temperature of 37.7°C. He had no neurological deficits and no paresthesia. Blood tests revealed a WBC of 14,200/µL and CRP was 1.8 mg/dL. MRI revealed a multilocular epidural mass contiguous with the L5/S1 intervertebral disc showing low intensity on T1-weighted image and high intensity on T2-weighted image [
Figure 2:
(a) Sagittal T2-weighted MRIs on admission showing L5/S1 high-intensity lesion of the intervertebral disc and abscess in the spinal canal. (b) Axial T2-weighted MRIs on admission showing L5/S1 high-intensity lesion of the intervertebral disc and abscess in the spinal canal. (c) Tyloma on sole of foot, suspected to be the source of infection. (d) Sagittal T2-weighted MRIs showing complete disappearance of the mass and the intensity change of the intervertebral disc. (e) Axial T2-weighted MRIs showing complete disappearance of the mass and the intensity change of the intervertebral disc.
Purulent spondylitis and an epidural abscess were diagnosed at L5/S1. Cefazolin (CEZ) administration was started based on antibiotic sensitivity tests. A whole-body examination revealed a tyloma on the sole of the foot [
DISCUSSION
Spinal infections are generally caused by hematogenous spread of bacteria to the spine and the tissues around it or from the direct spread of purulent lesions.[
MRI is reported to be an extremely effective diagnostic tool[
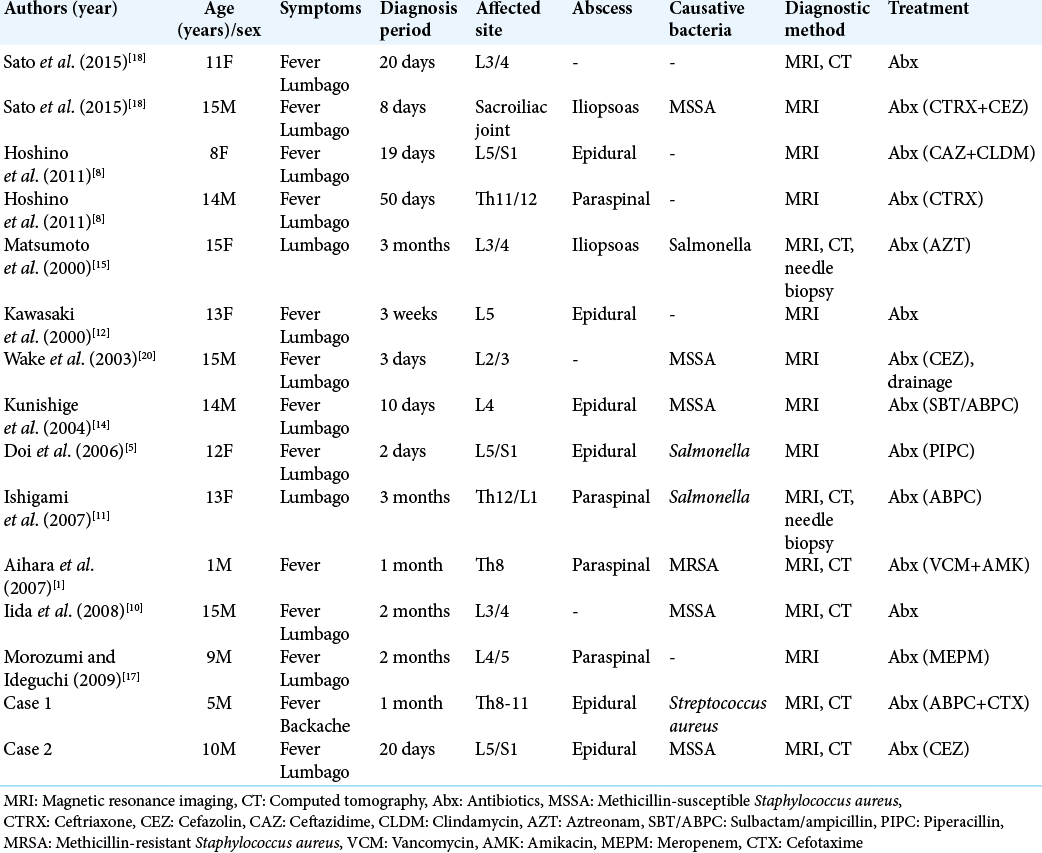
To study the recent trends in spinal infections, we analyzed 12 cases, including our own, in patients under the age of 15 reported in Japan since 2000 [
Imaging studies have been shown to be a poor indicator for disease regression and therefore treatment completion;[
CONCLUSION
A spinal infection should always be considered when examining a child with fever and back pain. Definitive diagnosis through MRI as well as collaboration with pediatricians, full body examination to determine the infection route, and appropriate antibiotic choice are all essential for successful treatment.
Ethical approval
Informed consent was obtained from patients and/or guardians before data use, and patient confidentiality was assured.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Aihara T, Yasuda T, Igarashi H. A case of infantile purulent spondylitis. Orthop Surg (in Japanese). 2007. 58: 415-8
2. An HS, Seldomridge JA. Spinal infections: Diagnostic tests and imaging studies. Clin Orthop Relat Res. 2006. 444: 27-33
3. Cottle L, Riordan T. Infectious spondylodiscitis. J Infect. 2008. 56: 401-12
4. Dayer R, Alzahrani MM, Saran N, Ouellet JA, Journeau P, Tabard-Fougere A. Spinal infections in children: A multicentre retrospective study. Bone Joint J. 2018. 100: 542-8
5. Doi O, Ito K, Takamatsu K, Aikawa J. A case of pyogenic spondylitis due to Salmonella. Tohoku J Orthop Traumatol (in Japanese). 2006. 50: 99-102
6. Grammatico L, Baron S, Rusch E, Lepage B, Surer N, Desenclos JC. Epidemiology of vertebral osteomyelitis (VO) in France: Analysis of hospital-discharge data 2002-2003. Epidemiol Infect. 2008. 136: 653-60
7. Herren C, Jung N, Pishnamaz M, Breuninger M, Siewe J, Sobottke R. Spondylodiscitis: Diagnosis and treatment options. Deutsch Arztebl Int. 2017. 114: 51-2
8. Hoshino A, Sato Y, Matsuhash K, Suzuki T, Yamaguchi K, Kitanaka Y, Sato Y. Two cases of spinal infection in children. J Japanese Soc Pediatr Radiol (in Japanese). 2011. 27: 71-6
9. Houston R, Gagliardo C, Vassallo S, Wynne PJ, Mazzola CA. Spinal epidural abscess in children: Case report and review of the literature. World Neurosurg. 2019. 126: 453-60
10. Iida T, Takahashi H, Katori S, Tsuchiya K, Suguro T, Harata T. Study of childhood purulent spondylitis. J Japanese Pediatr Orthop Assoc (in Japanese). 2008. 17: 54-7
11. Ishigami S, Yoshida M, Kawakami M, Hashizume H, Nakagawa Y, Kioka M. Vertebral osteomyelitis caused by Salmonella Agona. Clin Orthop Surg (in Japanese). 2007. 42: 167-70
12. Kawasaki T, Matsumoto S, Minomo H, Iwamatsu Y. A case of childhood purulent spondylitis. Orthop Surg (in Japanese). 2000. 51: 415-8
13. Khan IA, Vaccaro AR, Zlotolow DA. Management of vertebral diskitis and osteomyelitis. Orthopedics. 1999. 22: 758-65
14. Kunishige M, Ito N, Ukae S, Takebayashi T. A Case of pyogenic spondylitis who was at first diagnosed as pyelonephritis because of fever and back. J Jpn Pediatr Soc (in Japanese). 2004. 52: 119-22
15. Matsumoto M, Mori R, Kinoshita G, Maruoka R, Maruo S. A case of purulent spondylitis due to Salmonella. J Japanese Soc Lumbar Spine Disord (in Japanese). 2000. 6: 39-45
16. Moritani T, Kim J, Capizzano AA, Kirby P, Kademian J, Sato Y. Pyogenic and non-pyogenic spinal infections: Emphasis on diffusion-weighted imaging for the detection of abscesses and pus collections. Br Inst Radiol. 2014. 87: 1041
17. Morozumi M, Ideguchi M. A case report of pygenic spondylodiscitis in 9 years-old boy treated with consevative therapy. Central Jpn J Orthop Surg Traumatol (in Japanese). 2009. 52: 379-80
18. Sato T, Yasuda M, Hiraki A, Suwabe N, Koyake H, Kikuchi M. Two cases of pyogenic spinal infection in children. Japanese J Pediatr (in Japanese). 2015. 68: 1182
19. Varma R, Lander P, Assaf A. Imaging of pyogenic infectious spondylodiskitis. Radiol Clin North Am. 2001. 39: 203-13
20. Wake S, Eto M, Tomonaga T, Takahara K, Kushida M, Inadomi K, Akase K, Yamaguchi T, Sindo H. Pyogenic lumber facet joint lnfection: A case report. Orthop Traumatol (in Japanese). 2003. 52: 73-6
21. Wang Q, Babyn P, Branson H, Tran D, Davila J, Mueller EL. Utility of MRI in the follow-up of pyogenic spinal infection in children. Pediatr Radiol. 2010. 40: 118-30
22. Zimmerli W. Clinical practice. Vertebral osteomyelitis. N Engl J Med. 2010. 362: 1022-9