- Department of Surgery, Hawler Medical University, College of Medicine, Erbil, Iraq
- Department of Surgery, University of Baghdad, College of Medicine, Baghdad, Iraq
- Department of Surgery, Iraqi Medical Association, Baghdad, Iraq
- Department of Surgery, Babylon University, College of Medicine, Babylon, Iraq
- Faculty of Medicine, Zagazig University, Sharqia Governorate, Egypt, Iraq
- Department of Surgery, Baghdad Teaching Hospital, Baghdad, Iraq
Correspondence Address:
Injam Ibrahim Sulaiman, Department of Surgery, Hawler Medical University, College of Medicine, Erbil, Iraq.
DOI:10.25259/SNI_632_2024
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Injam Ibrahim Sulaiman1, Ahmed Shakir Ali Al-Wassiti2, Mohammed Bani Saad3, Mohammed Tareq Mutar2, Rokaya H. Abdalridha4, Sajjad G. Al-Badri2, Toka Elboraay5, Mustafa Ismail6. Penetrating orbital trauma: Comprehensive review and meta-analysis of bullet injuries. 20-Dec-2024;15:465
How to cite this URL: Injam Ibrahim Sulaiman1, Ahmed Shakir Ali Al-Wassiti2, Mohammed Bani Saad3, Mohammed Tareq Mutar2, Rokaya H. Abdalridha4, Sajjad G. Al-Badri2, Toka Elboraay5, Mustafa Ismail6. Penetrating orbital trauma: Comprehensive review and meta-analysis of bullet injuries. 20-Dec-2024;15:465. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=13300
Abstract
Background: Orbital bullet injuries resulting from high-velocity trauma pose significant clinical challenges due to the potential for severe ocular and systemic complications. This meta-analysis consolidates the existing body of knowledge on direct orbital bullet injuries with respect to clinical outcomes, management strategies, and long-term effects.
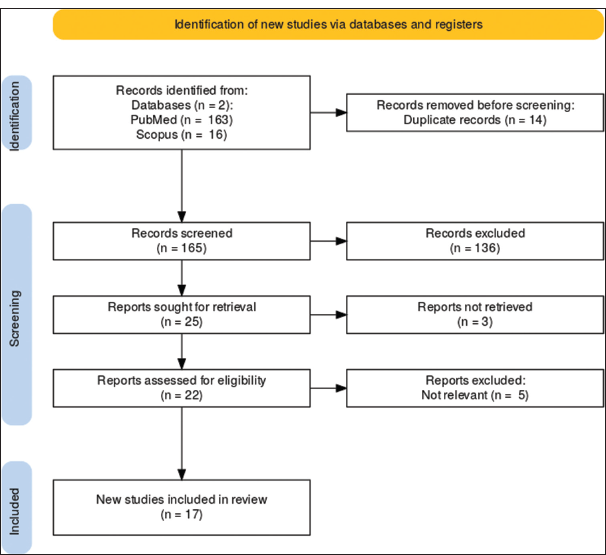
Methods: The literature search was conducted by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses, using databases such as PubMed and Scopus. Seventeen articles were reviewed, out of which six studies met the inclusion criteria. Extracted data included details on study design, sample size, patient demographics, projectile type, clinical presentation, imaging modalities used in establishing the diagnosis, surgical interventions performed, duration of follow-up, and the outcomes achieved. Data synthesis was done using fixed and random effects models; heterogeneity testing was assessed using the I2 statistic.
Results: A total of 688 patients with orbital bullet injuries were analyzed. The average age years ranged from 7 to 58, with a predilection for the male gender, about 70%. These injuries caused marked visual impairment, which included optic nerve injuries, legal blindness, cornea injuries, hyphema, orbital fractures, vitreous hemorrhage, lid lacerations, cataracts, and retinal injuries. Optic nerve injuries exhibited substantial variability (I2 = 100%, H2 = 1.254 × 108). Legal blindness was common (I2 = 100%, H2 = 1.628 × 107), with high rates reported in conflict zones. Corneal injuries and hyphema were also prevalent, with significant heterogeneity observed (I2 = 100%, H2 = 8.183 × 106 for corneal injuries and I2 = 99.861%, H2 = 721.638 for hyphema). Only orbital fractures, vitreous hemorrhage, lid lacerations, cataracts, and retinal injuries showed very high heterogeneity with varying clinical presentation. Early surgical intervention and advanced imaging techniques played a very vital role in the management of these injuries and those which improved the prognosis of outcome.
Conclusion: Orbital bullet injuries remain a great clinical challenge and are very variable in nature. This huge variability of injury patterns and outcomes enjoins that treatment must be individualized, with very early intervention, evolved imaging modalities, and thorough surgical management for the best possible improvement in the patient’s outcomes and prevention of long-term sequelae. Further studies should be done to come up with unified guidelines regarding the evaluation and treatment of such complex injuries.
Keywords: Bullet injury, Meta-analysis, Ocular trauma, Orbital trauma, Surgical management, Visual outcomes
INTRODUCTION
Orbital bullet injuries are a type of high-velocity trauma that creates the most challenging clinical situations because it is associated with a very poor prognosis in ocular and systemic complications. In an overall sense, such injuries would depend on factors such as projectile velocity, entry point, and relation to vital orbital structures. For example, Pacio et al.[
Nonlethal missiles, rubber, and plastic bullets utilized during riot control also considerably cause orbital trauma. According to some studies, these projectiles range from lid lacerations to globe ruptures and, even further on, orbital fractures in conflict zones.[
Management of these injuries often requires prompt surgical intervention, especially in cases involving intraorbital foreign bodies. The decision to remove or observe these foreign bodies depends on their size, location, and associated risks.[
We aim to consolidate existing knowledge on direct orbital bullet injuries, evaluating clinical outcomes, management strategies, and long-term effects. By synthesizing data from various studies, we aim to provide a clearer understanding of best practices and areas for further research in managing these complex injuries.
METHODS
Literature search
A comprehensive literature search was performed following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines[
Inclusion and exclusion criteria
Inclusion and exclusion criteria were established to select the relevant studies. Studies were included if they reported cases of direct orbital bullet injuries, provided detailed clinical outcomes, management strategies, and long-term follow-up, included human subjects, and were published in peer-reviewed journals. Conversely, studies were excluded if they involved deceased and nonhuman subjects, lacked detailed clinical data or outcomes, or were review articles, commentaries, or editorials without original data.
Data extraction
Data extraction was conducted independently by two reviewers using a standardized form. The extracted information encompassed study design, sample size, patient demographics (including age and sex), type of projectile and its velocity, clinical presentation, imaging modalities used, surgical interventions and management strategies, follow-up duration, and outcomes, as well as complications and long-term consequences.
Quality assessment and bias assessment
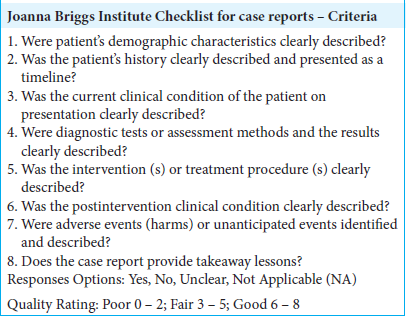
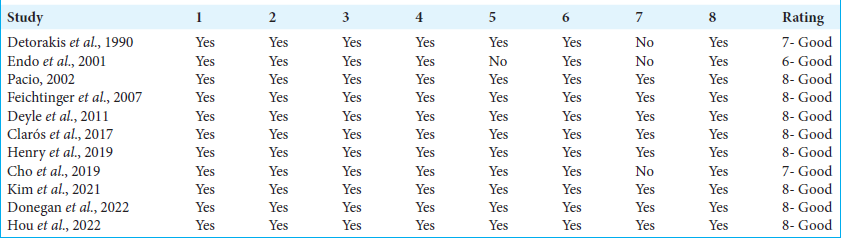
The quality of the included studies was assessed using the Oxford Centre For Evidence-Based Medicine guidelines.[
Data synthesis and statistical analysis
Data were synthesized narratively and quantitatively. A meta-analysis was performed using fixed and random effects models to pool outcomes across studies. Heterogeneity was assessed using the I2 statistic. Subgroup analyses were conducted based on the type of projectile and surgical intervention.
RESULTS
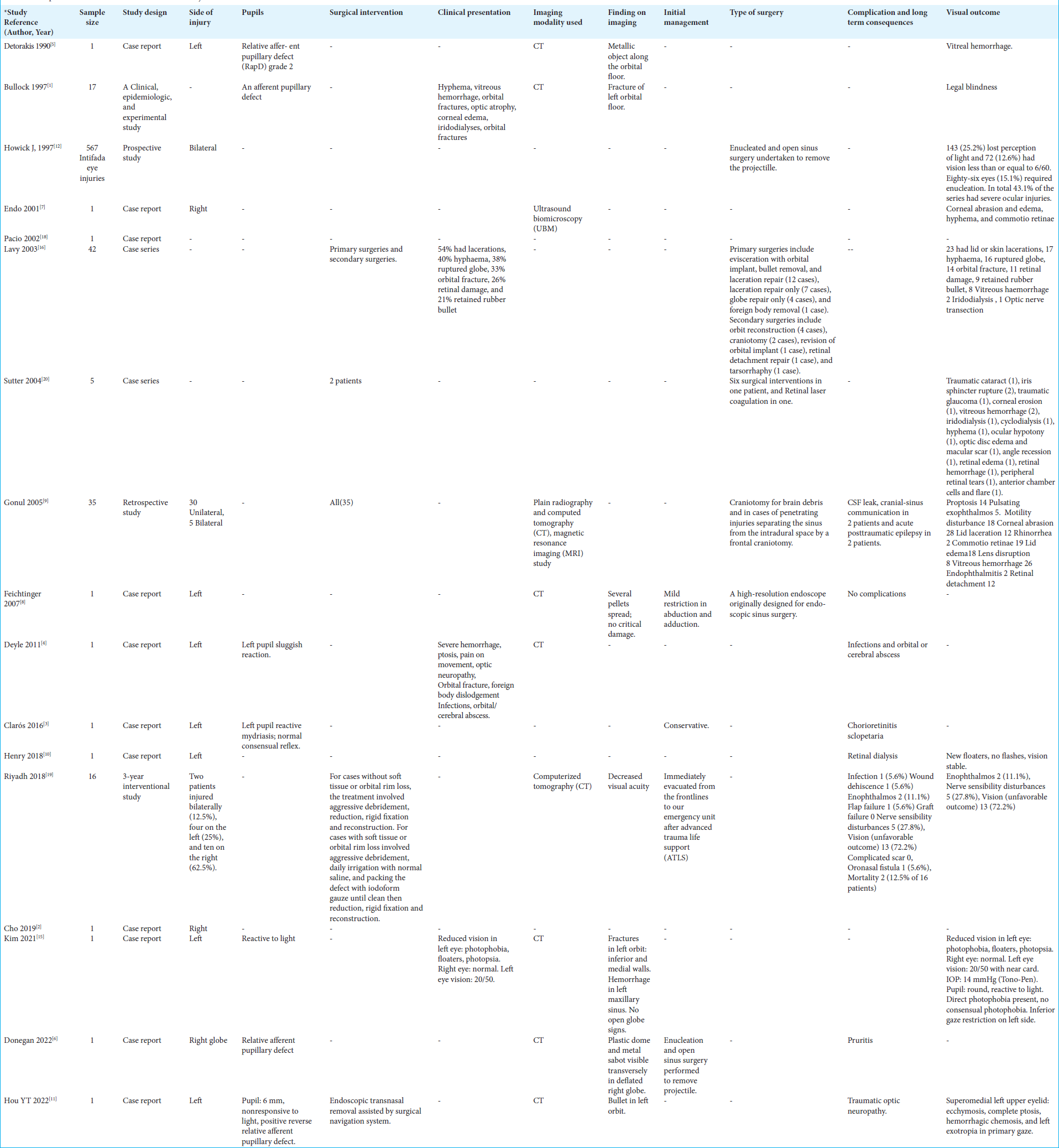
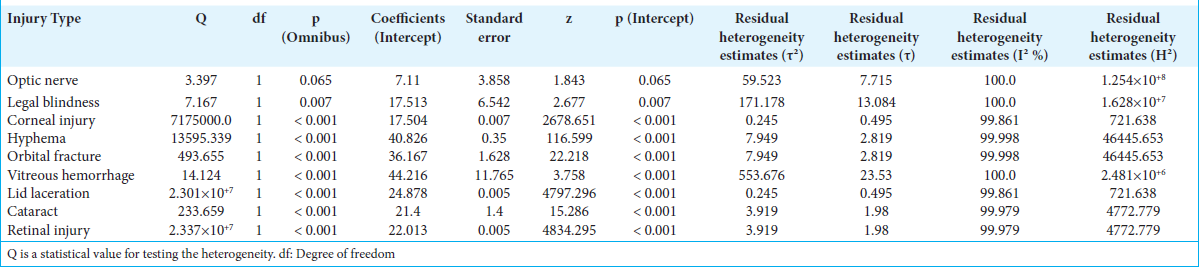
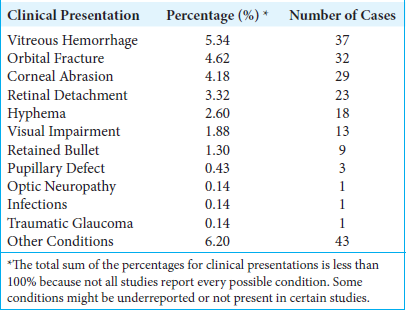
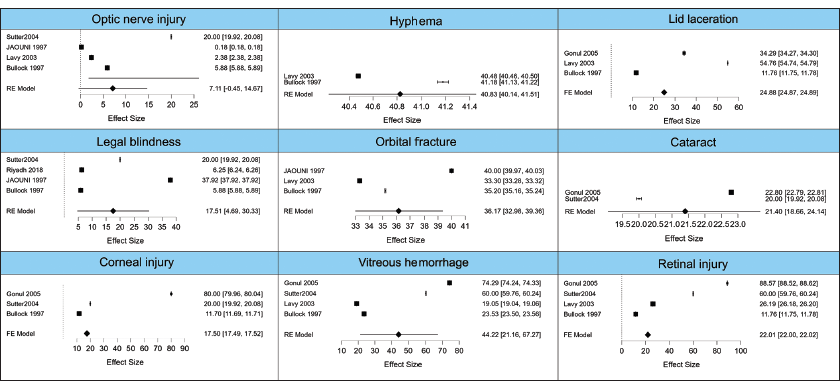
We included 6 articles in this meta-analysis out of 17. The analyses included assessing the prevalence and severity of optic nerve injuries, legal blindness, corneal injuries, hyphema, orbital fractures, vitreous hemorrhage, lid lacerations, cataracts, and retinal injuries. The results are illustrated in
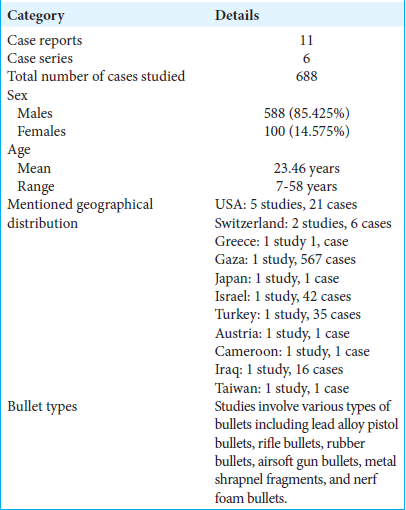
Demographics and clinical presentation
The additional data incorporated from the second file included a total of 693 patients. The average age varied across studies, with specific age ranges from 7 to 58 years. The gender distribution showed a predominance of male patients (85.425%), reflecting a higher incidence of orbital bullet injuries in males. The types of projectiles causing injuries included lead alloy pistol bullets, rubber bullets, plastic bullets, airsoft gun pellets, and metallic shrapnel fragments. These details are well illustrated in
Clinical presentations
The clinical presentation of injuries included a range of ocular and orbital complications. The most common injuries were hyphema, vitreous hemorrhage, orbital fractures, and optic nerve injuries. For example, Bullock et al.[
Optic nerve injuries
The meta-analysis of optic nerve injuries included data from multiple studies. The omnibus test of model coefficients was not statistically significant (Q = 3.397, df = 1, P = 0.065), indicating no significant overall effect. However, the residual heterogeneity was significant (Q = 1.79 × 10^7, df = 3, P < 0.001), suggesting substantial variability among the included studies. The estimate for the intercept was 7.110 with a standard error of 3.858 (z = 1.843, P = 0.065). The I2 value was 100%, indicating high heterogeneity, and the H2 value was 1.254 × 108. The forest plot for optic nerve injuries showed wide confidence intervals for most studies, highlighting the variability in reported outcomes, particularly in studies by Bullock et al.,[
Legal blindness
The meta-analysis for legal blindness demonstrated a significant omnibus test of model coefficients (Q = 7.167, df = 1, P = 0.007). The residual heterogeneity was also significant (Q = 1.421 × 108, df = 3, P < 0.001), reflecting high variability. The estimate for the intercept was 17.513 with a standard error of 6.542 (z = 2.677, P = 0.007). The I2 value was 100%, indicating complete heterogeneity and the H2 value was 1.628 × 107. The forest plot for legal blindness indicated that while some studies reported high rates of blindness, others showed lower incidences, contributing to the overall heterogeneity, particularly in studies by Bullock et al.,[
Corneal injuries
For corneal injuries, the omnibus test of model coefficients was highly significant (Q = 7.175 × 106, df = 1, P < 0.001). The test of residual heterogeneity also showed significant results (Q = 8.183 × 106, df = 2, P < 0.001). The estimate for the intercept was 17.504 with a standard error of 0.007 (z = 2678.651, P < 0.001), indicating a strong effect size. The I2 value was 100%, showing high heterogeneity, and the H2 value was 8.183 × 106. The forest plot for corneal injuries illustrated that nearly all studies reported significant injury rates, although with varying effect sizes, including studies by Endo et al.,[
Hyphema
The hyphema meta-analysis revealed a significant omnibus test of model coefficients (Q = 13595.339, df = 1, P < 0.001) and significant residual heterogeneity (Q = 721.638, df = 1, P < 0.001). The intercept estimate was 40.826 with a standard error of 0.350 (z = 116.599, P < 0.001). The I2 value of 99.861% indicated substantial heterogeneity, and the H2 value was 721.638. The forest plot showed consistently high rates of hyphema across studies, with relatively narrow confidence intervals, particularly in studies by Bullock et al.,[
Orbital fractures
The analysis of orbital fractures indicated a significant omnibus test of model coefficients (Q = 493.655, df = 1, P < 0.001) with significant residual heterogeneity (Q = 186492.005, df = 2, P < 0.001). The intercept estimate was 36.167 with a standard error of 1.628 (z = 22.218, P < 0.001). The I2 value of 99.998% showed high heterogeneity, and the H2 value was 46445.653. The forest plot for orbital fractures highlighted the varying severity and frequency of fractures reported in different studies, including those by Bullock et al.,[
Vitreous hemorrhage
The vitreous hemorrhage analysis showed a significant omnibus test of model coefficients (Q = 14.124, df = 1, P < 0.001) and significant residual heterogeneity (Q = 6.600 × 106, df = 3, P < 0.001). The intercept estimate was 44.216 with a standard error of 11.765 (z = 3.758, P < 0.001). The I2 value was 100%, indicating high heterogeneity, and the H2 value was 2.481 × 106. The forest plot depicted wide confidence intervals for vitreous hemorrhage rates, suggesting varied reporting among studies, including those by Bullock et al.[
Lid lacerations
For lid lacerations, the omnibus test of model coefficients was highly significant (Q = 2.301 × 107, df = 1, P < 0.001), and the test of residual heterogeneity also showed significant results (Q = 9.766 × 106, df = 2, P < 0.001). The intercept estimate was 24.878 with a standard error of 0.005 (z = 4797.296, P < 0.001). The I2 value was 100%, showing high heterogeneity, and the H2 value was 9.766 × 106. The forest plot for lid lacerations showed consistent findings across studies, with high effect sizes reported, including those by Lavy and Abu Asleh,[
Cataracts
The cataract meta-analysis demonstrated a significant omnibus test of model coefficients (Q = 233.659, df = 1, P < 0.001) with significant residual heterogeneity (Q = 4772.779, df = 1, P < 0.001). The intercept estimate was 21.400 with a standard error of 1.400 (z = 15.286, P < 0.001). The I2 value was 99.979%, indicating substantial heterogeneity, and the H2 value was 4772.779. The forest plot indicated variable but generally high rates of cataracts reported in the studies, including those by Sutter[
Retinal injuries
The analysis for retinal injuries showed a highly significant omnibus test of model coefficients (Q = 2.337 × 107, df = 1, P < 0.001) and significant residual heterogeneity (Q = 9.660 × 106, df = 3, P < 0.001). The intercept estimate was 22.013 with a standard error of 0.005 (z = 4834.295, P < 0.001). The I2 value was 100%, showing high heterogeneity, and the H2 value was 9.660 × 106. The forest plot for retinal injuries demonstrated wide confidence intervals and varied effect sizes across studies, including those by Bullock et al.,[
Visual acuity and clinical outcomes
Visual acuity outcomes varied significantly among the patients. For instance, Bullock et al. reported[
Imaging modalities
Imaging modalities such as computed tomography (CT) and ultrasound biomicroscopy were in frequent use for ascertaining the extent of the injuries and planning surgical intervention. CT was especially helpful in picking up fractures and foreign bodies within the orbit. For example, orbital floor fractures and foreign bodies were shown in CT imaging by Bullock et al. study.[
Management strategies and surgical techniques
Most of the management strategies included surgical interventions. Detorakis et al.[
The surgical interventions varied according to the extent and nature of the injury. The most common surgeries undertaken were evisceration with orbital implant, removal of bullet, and laceration repair, according to Lavy and Abu Asleh.[
Complications and long-term outcomes
Such complications were common and included infections, wound dehiscence, enophthalmos, and flap failure. Other long-term consequences included serious visual impairment in some patients, with partial or complete recovery achieved by others. For instance, Riyadh et al.[
These results underline that orbital bullet injuries are a formidable clinical challenge with a very wide range of outcomes. Hence, the importance of early intervention, proper surgical management, and state-of-the-art imaging techniques in improving prognosis and reducing long-term morbidity cannot be overemphasized. The variability in injury types and outcomes underlines the individualization of treatment plans and further research into the optimization of management strategies. The overall bias assessment for the study was determined to be good, indicating a low risk of systematic errors that could impact the validity of the findings [
DISCUSSION
These meta-analysis results underline the comprehensive and diversified effect of orbital bullet injuries. The findings also reflected a significant heterogeneity across different types of injury, reflecting that a huge number of factors, such as projectile type, velocity, and initial medicamentous interventions applied, influence the injuries. Although most of the results ranged from damage to the optic nerve and retinal injuries, high variability in the outcome indicates that treatment should be individualized. Such results underline the fact that orbital bullet injuries can be very complicated and require advanced imaging techniques, surgical interventions, and follow-up care if an improvement in patient outcome is wished to be attained.
Effects of orbital bullet impact on the optic nerve are also highly variable, with significant residual heterogeneity (I2 = 100%, H2 = 1.254 × 108). Such kinds of injury are really related to high-velocity missile injuries that usually result in very serious consequences, including optic neuropathy and blindness. Bullock et al.,[
Legal blindness, I2 = 100%, H2 = 1.628 × 107 – the heterogeneity here is very large – implies very severe vision loss due to orbital-bullet-induced causes. Bullock et al.,[
Corneal injuries were highly prevalent with significant heterogeneity (I2 = 100%, H2 = 8.183 × 106). Endo et al.,[
Hyphema was another common injury with high heterogeneity (I2 = 99.861%, H2 = 721.638). Bullock et al.,[
Orbital fractures indicated significant results (I2 = 99.998%, H2 = 46445.653). Bullock et al.,[
Vitreous hemorrhage showed significant heterogeneity (I2 = 100%, H2 = 2.481 × 106). The reports by Bullock et al.,[
Lid lacerations were highly prevalent with significant heterogeneity (I2 = 100%, H2 = 9.766 × 106). Studies by Lavy and Abu Asleh,[
The cataract meta-analysis demonstrated substantial heterogeneity (I2 = 99.979%, H2 = 4772.779). According to Sutter[
Retinal injuries showed significant results with high heterogeneity (I2 = 100%, H2 = 9.660 × 106). Bullock et al.,[
The gross heterogeneity seen across all types of injury does not suggest that individual patient factors, projectile characteristics, and medical interventions play no role. The findings underscore the need for comprehensive management that includes prompt surgical intervention, advanced imaging techniques, and long-term follow-up to optimize clinical outcomes. For example, high-resolution CT and magnetic resonance imaging aid in the correct diagnosis and planning of surgical intervention, hence improving prognosis in patients with complex orbital injuries.
The present meta-analysis has several limitations. The included studies were of different designs, and sample size and quality differed considerably, as reflected by the significant heterogeneity. Moreover, differences in outcome reporting – in combination with the diversity of applied imaging and surgical techniques – might have had a conceivable influence on the measured outcomes. Future studies should seek standard reporting and exhaust maximum effort to include larger sample sizes for more robust data. In addition, multicenter studies may help generalize the findings to different populations and healthcare settings.
CONCLUSION
The meta-analysis underscores the orbital bullet injuries heterogeneity and seriousness, hereby needing tailored clinical approaches for case management. Therefore, variable outcomes arise because of differences in effective early interventions, advanced imaging modalities, and surgical interventions, which are comprehensive for optimal recovery of the patient and prevention of long-term complications. Future studies should seek to standardize protocols regarding the assessment and management of orbital bullet injuries so that better patient care and outcomes can be attained.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Bullock JD, Ballal DR, Johnson DA, Bullock RJ. Ocular and orbital trauma from water balloon slingshots. A clinical, epidemiologic, and experimental study. Ophthalmology. 1997. 104: 878-87
2. Cho SM, Cho D, Read-Fuller A, Vrcek I. Orbitozygomatic approach for bullet retrieval from the temporal fossa. Proc (Bayl Univ Med Cent). 2019. 32: 435-7
3. Clarós P, Fokouo JV, Clarós A. Intraorbital foreign body: A rifle bullet removed 20 years after the accident. Eur Ann Otorhinolaryngol Head Neck Dis. 2017. 134: 63-65
4. Deyle S, Exadaktylos AK, Kneubuehl BP, Buck U, Thali MJ, Voisard MX. Collateral damage--penetrating head injury and orbital injury: A case report. Am J Forensic Med Pathol. 2011. 32: 215-8
5. Detorakis ET, Symvoulakis EK, Drakonaki E, Halkia E, Tsilimbaris MK. Unexpected finding in ocular surface trauma: A large intraorbital foreign body (bullet). Acta Medica (Hradec Kralove). 2012. 55: 100-3
6. Donegan PJ, Niear MA, Law JC, Barahimi B. Military marking round injury to the globe. J Emerg Trauma Shock. 2022. 15: 108-10
7. Endo S, Ishida N, Yamaguchi T. Tear in the trabecular meshwork caused by an airsoft gun. Am J Ophthalmol. 2001. 131: 656-7
8. Feichtinger M, Zemann W, Kärcher H. Removal of a pellet from the left orbital cavity by image-guided endoscopic navigation. Int J Oral Maxillofac Surg. 2007. 36: 358-61
9. Gönül E, Erdoğan E, Taşar M, Yetişer S, Akay KM, Düz B. Penetrating orbitocranial gunshot injuries. Surg Neurol. 2005. 63: 24-30 discussion 31
10. Henry T, Palakkamanil M, Rubin U, Tennant M. Traumatic retinal dialysis resulting from Nerf foam bullet. Can J Ophthalmol. 2019. 54: e100-2
11. Hou YT, Wei YH, Liao CK, Lin CF. Personalized multidisciplinary approach of orbital apex foreign body: A case report and literature review. Taiwan J Ophthalmol. 2022. 12: 374-7
12. Howick JChalmers IGlasziou PGreenhalgh THeneghan CLiberati A. Explanation of the 2011 Oxford centre for evidence-based medicine (OCEBM) levels of evidence (Background Document). Available from: https://www.cebm.ox.ac.uk/resources/levels-of-evidence/ocebm-levels-of-evidence [Last acceessed on 2024 Jul 24].
13. Jaouni ZM, O’Shea JG. Surgical management of ophthalmic trauma due to the Palestinian intifada. Eye (Lond). 1997. 11: 392-7
14. Joanna Briggs Institute. Checklist for case reports. Available from: https://jbi.global/critical-appraisal-tools [Last acceessed on 2024 Jul 24].
15. Kim HJ, Ali S, Kelly LD. Ocular foam round injury: A case report and literature review. Am J Ophthalmol Case Rep. 2021. 23: 101149
16. Lavy T, Asleh SA. Ocular rubber bullet injuries. Eye (Lond). 2003. 17: 821-4
17. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ. 2021. 372: n71
18. Pacio J. Monocular blindness caused by a BB embolus: A case report. Pediatrics. 2002. 110: 776-8
19. Riyadh S, Abdulrazaq SS, Zirjawi AM. Surgical management of the recent orbital war injury. J Craniofac Surg. 2018. 29: 1123-6
20. Sutter FK. Ocular injuries caused by plastic bullet shotguns in Switzerland. Injury. 2004. 35: 963-7