- Department of Neurosurgery, Anna–Stift Hospital, Löningen, Germany
- Department of Neurosurgery, Eldermerdash Hospital, Cairo, Egypt
- Department of Neurosurgery, Gazi University Faculty of Medicine, Ankara, Turkey
Correspondence Address:
Aydemir Kale, Department of Neurosurgery, Gazi University Faculty of Medicine, Ankara, Turkey.
DOI:10.25259/SNI_144_2025
Copyright: © 2025 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Thomas Luebbers1, Albatol Ali2, Rainer Baalmann1, Aydemir Kale3. Percutaneous endoscopic lumbar discectomy for extreme lateral lumbar disc herniation. 25-Apr-2025;16:150
How to cite this URL: Thomas Luebbers1, Albatol Ali2, Rainer Baalmann1, Aydemir Kale3. Percutaneous endoscopic lumbar discectomy for extreme lateral lumbar disc herniation. 25-Apr-2025;16:150. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=13522
Abstract
BackgroundFar lateral disc herniation (FLDH) constitutes a minor portion of the total discectomy workload for spine surgeons. So far, there is still a debate about the term “extreme lateral,” and in general, it describes the intra - and extraforaminal position of the disc herniation. We present a surgical treated case series in which the disc herniation on the lumbar spine was still ventral of the exiting nerve root far outside of the foramen.
MethodsStudy Design and Patient Characteristics: retrospective analysis of 14 surgical treated patients. Surgical Technique: In all patients, the so-called foraminal retreat maneuver (percutaneous endoscopic lumbar discectomy) was performed. A foraminoscope with a 15° optic orientation and a nonbeveled working sleeve were used in all cases. The aforementioned technique represents a modification of the “inside-out” endoscopic surgery on the lumbar spine.
ResultsWe treated 11 male and 3 female patients with an average age of 67 years and 66 years, respectively. Except for one, 13 patients presented with clear monoradicular symptoms accompanied by mild-to-moderate neurological deficits. In 11 cases, the disc herniation exhibited cranial migration; two were at the disc level, and in another case, caudal migration was observed. Immediate pain relief and significant improvement of neurological symptoms occurred in all patients. Two patients developed neuropathic pain, which improved after conservative treatment within 6 weeks following the procedure. No recurrence was observed in this case series.
ConclusionPatients suffering from extreme lateral lumbar disc herniation were found to be significantly older. Furthermore, there is a higher tendency toward male patients and cranial migration of the herniation. The described and modified inside-out technique, along with a 15° optic, allows for clear identification of the exiting nerve root and safe removal of the displaced disc herniation far outside of the spinal canal and foramen. No complications occurred in this small series, and the development of neuropathic pain appears to be relatively common.
Keywords: Endoscope, Extreme lateral, Lumbar disc herniation, Transforaminal
INTRODUCTION
In 1974, Abdullah et al. were the first to describe an extreme lateral lumbar disc herniation.[
At present, there are no case series or research articles in the common and recent literature addressing this specific type of lumbar disc herniation. Far lateral disc herniation (FLDH) constitutes a minor portion of the total discectomy workload for spine surgeons. The overall incidence ranged from 3% to 12% of all lateral disc herniation (LDH).[
Far lateral LDH presents with some unique clinical features. First, it often occurs in older patients, with a peak age in the sixth decade.[
MATERIALS AND METHODS
Study design and patient characteristics
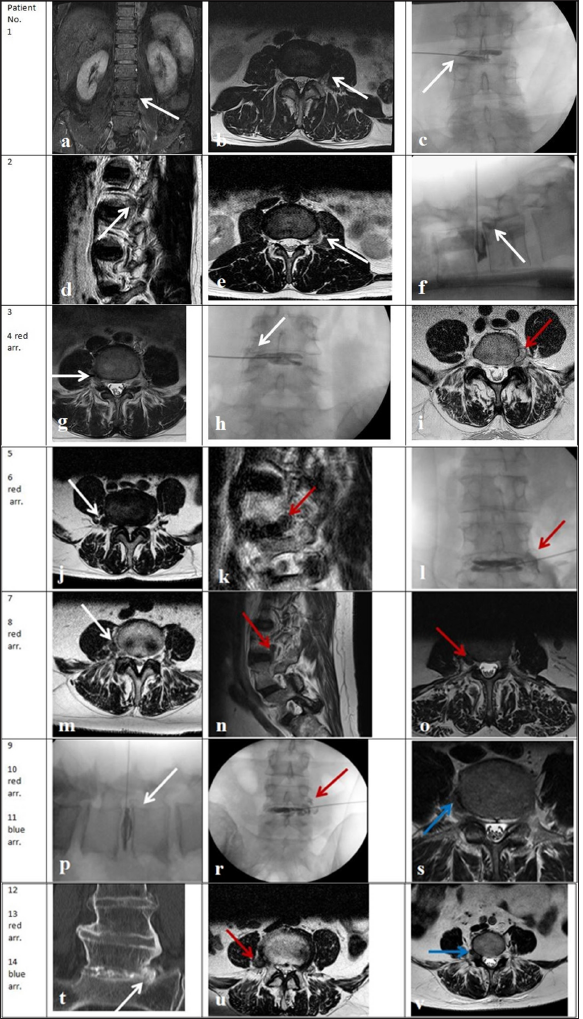
Retrospective analysis of 14 surgical treated patients (from May 2016 to April 2024). All patients provided informed consent to be included in this case series, and all of them, the same surgical technique was applied. Imaging findings of all patients and the diagnosis of an extreme lateral disc herniation are documented in
Surgical technique
The surgical intervention employed percutaneous endoscopic lumbar discectomy. In all patients, the so-called foraminal retreat maneuver was performed.[
Surgical technique steps:
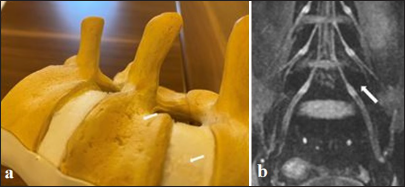
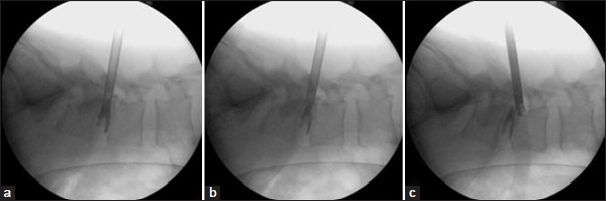
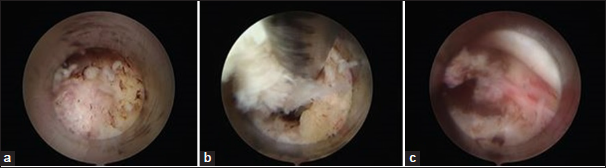
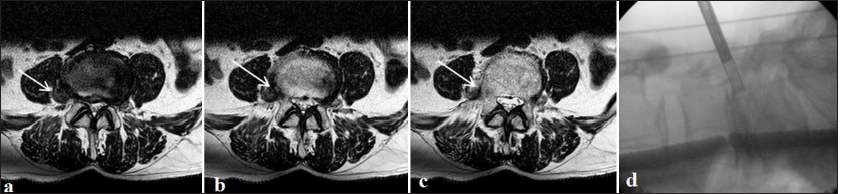
The procedures were performed with the patients under general anesthesia in the prone position with slightly flexed hips and knees on the Wilson frame. Nerve root monitoring through free-run electromyography (EMG) or stimulated EMG was done sometimes but not routinely.[ Guided by the C-arm in two planes, the puncture of the intervertebral disc with a discography needle targeting the central part through Kambin’s triangle was performed. After the insertion of the needle, discography was conducted A guide wire was inserted through the needle channel into the disc, and a small stab incision was made at the entry site of the needle After withdrawing the needle, a conical dilatator was slid over the guide wire and advanced into the disc space After insertion of the working sleeve and endoscope, internal decompression of the disc was performed After the internal decompression, the working cannula was pulled out from the central disc space to the foramen. The nonbeveled tip of the working cannula was positioned in the cephalad and lateral direction close to the posterior wall of the vertebra (“foraminal retreat”), serving as a retractor to the more ventral mobilized exiting nerve root also.[ In the case of cranial migration of the sequester, the edge of the lateral caudal endplate was exposed to enter the lateral concavity of the vertebral body and to visualize the herniation [
RESULTS
The distribution along the lumbar spine was as follows: two patients at L5/S1, eight patients at L4/5, three patients at L3/4, and finally, one patient at L2/3. We treated 11 male and 3 female patients with an average age of 67 years and 66 years, respectively. Except for one,[
Immediate pain relief and significant improvement of neurological symptoms occurred in all patients. Two patients developed neuropathic pain, which improved after conservative treatment within 6 weeks following the procedure. No recurrence was observed in this case series [
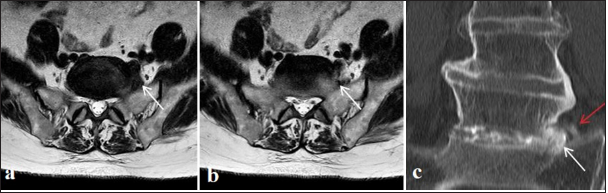
Patient No. 12 was suffering from acute left leg pain and L5 radiculopathy, followed by mild neurological deficits. MRI in the disc level L4/5 was inconspicuous, and in axial T2 weight images, a presacral luxation was supposed. The diagnosis was confirmed by discography with connected CT of the lumbosacral level, followed by multiplanar reconstruction in the selected bone window [
DISCUSSION
FLDH is defined as a disc herniation located on the sagittal plane laterally to the medial wall of the pedicle.[
Nowadays, the transforaminal endoscopic, percutaneous discectomy method is becoming increasingly widespread. Successful results are reported with this minimally invasive technique.[
In a summary of surgical treated far lateral lumbar disc herniation reported as suspicious for nerve sheath tumors, Uy BR et al. presented two own cases and five separate published case reports. In three of them, the dorsal approach was chosen, and a hemilaminectomy paired with a complete facetectomy was performed. In two cases, transposase access in a lateral decubitus position was elected, and finally, in two patients, an anterior transperitoneal or retroperitoneal approach was selected.[
Paramedian lumbar disc herniations are generally reported in the 30–50 age range.[
Limitations of this study include its retrospective nature. In addition, later examinations and a clinical follow-up of the patients were not carried out.
However, the technology described here allows different alignments of the working sleeves outside the foramen to secure the safe identification of the nerve roots and the unusually far lateral migrated sequester. In contrast to the very heterogeneous open surgical approaches, this presented percutaneous endoscopic technique is, to our knowledge, the first minimal invasive access dealing with very demanding and complex disc pathologies on the lumbar spine.
CONCLUSION
Patients suffering from extreme lateral lumbar disc herniation were found to be significantly older compared to the general occurrence in the population of symptomatic lumbar disc herniation. Furthermore, there is a higher tendency toward male patients and cranial migration of the herniation. The modified inside-out technique, described as the foraminal retreat maneuver, along with a 15° optic, allows for clear identification of the exiting nerve root and safe removal of the displaced disc herniation far outside of the spinal canal and foramen. No complications occurred in this small series, and the development of neuropathic pain appears to be relatively common. The distribution along the lumbar spine shows no major deviations.
Authors’ contributions
Luebbers and Baalmann performed the surgeries and collected data. They also discussed the technique. Ali and Kale summarized and discussed the clinical data.
Ethical approval
The Institutional Review Board approval is not required as it is retrospective study.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Abdullah AF, Ditto EW, Byrd EB, Williams R. Extreme-lateral lumbar disc herniations. Clinical syndrome and special problems of diagnosis. J Neurosurg. 1974. 41: 229-34
2. Al-Khawaja DO, Mahasneh T, Li JC. Surgical treatment of far lateral lumbar disc herniation: A safe and simple approach. J Spine Surg. 2016. 2: 21-4
3. Chang SB, Lee SH, Ahn Y, Kim JM. Risk factor for unsatisfactory outcome after lumbar foraminal and far lateral microdecompression. Spine (Phila Pa 1976). 2006. 31: 1163-7
4. Epstein NE, Epstein JA, Carras R, Hyman RA. Far lateral lumbar disc herniations and associated structural abnormalities. An evaluation in 60 patients of the comparative value of CT, MRI, and myelo-CT in diagnosis and management. Spine (Phila Pa 1976). 1990. 15: 534-9
5. Fiorenza V, Ascanio F. Percutaneous endoscopic transforaminal outside-in outside technique for foraminal and extraforaminal lumbar disc herniations-operative technique. World Neurosurg. 2019. 130: 244-53
6. Foley KT, Smith MM, Rampersaud YR. Microendoscopic approach to far-lateral lumbar disc herniation. Neurosurg Focus. 1999. 7: e5
7. Hincapié CA, Kroismayr D, Hofstetter L, Kurmann A, Cancelliere C, Raja Rampersaud Y. Incidence of and risk factors for lumbar disc herniation with radiculopathy in adults: A systematic review. Eur Spine J. 2025. 34: 263-94
8. Jiang SD, Jiang LS, Dai LY. Extreme lateral lumbar disc herniation in a 12-year child: Case report and review of the literature. Eur Spine J. 2010. 19: S197-9
9. Karassawa-Zanoni D, Shekhrajka N, Kademian JC, FurtadoFreitas L. Giant extruded discal hernia mimicking an abscess within the psoas muscle: A very unusual presentation of a common disease. Rev Neurol. 2024. 78: 117-8
10. Kaya M, Keskin E, Ceylan D, Kacira T, Kitiki Kacira Ö. Surgical treatment of far lateral lumbar disc herniation: Outcomes of the safe and simple midline approach. Cureus. 2022. 11: e27907
11. Levene HB, Nimmagadda A, Levi AD. An unusual case of footdrop: Anterior disc herniation mimicking a nerve sheath tumor. Neurosurgery. 2010. 66: E19-20 discussion E420
12. Lübbers T, Abuamona R, Elsharkawy AE. Percutaneous endoscopic treatment of foraminal and extraforaminal disc herniation at the L5-S1 level. Acta Neurochir (Wien). 2012. 154: 1789-95
13. Lübbers T, Börm W, Meyer F, Bullmann V. Posterolateraler und transforaminaler zugang zur endoskopischen bandscheibenchirurgie. Wirbelsäule Interdiszip Schattauer Verlag. 2017. 1: 417-9
14. Lübbers T, Baalmann R, Sandvoss G. A rare case of extreme lateral disc herniation L4/5. Die Wirbelsäule. 2021. 5: 259-62
15. Moon KP, Suh KT, Lee JS. Reliability of MRI findings for symptomatic extraforaminal disc herniation in lumbar spine. Asian Spine J. 2009. 3: 16-20
16. Musa G, Abakirov MD, Arzoumi N, Mamyrbaev ST, Castillo RE, Chmutin GE. Is transforaminal endoscopic discectomy the best option for recurrent lumbar disc herniation? A systematic review. Int J Spine Surg. 2025. 6: 49-56
17. Musharbash FN, Lee SH. A modified endoscopic access for lumbar foraminal pathologies; Posterolateral “intertransverse” endoscopic approach to minimize postoperative dysesthesia following transforaminal approach. Neurospine. 2023. 20: 150-7
18. Nazwar TA, Bal’afif F, Wardhana DW, Panjaitan C. A comparative study of transforaminal and interlaminar approaches in percutaneous endoscopic lumbar discectomy for L5-S1 disc herniation: Systematic review. J Clin Neurosci. 2025. 133: 111022
19. Odent JB, Castel X, Vieira TD, Brahim EB, Fière V, D’Astorg H. Beyond traditional surgery for far lateral lumbar herniation: Transforaminal full endoscopic discectomy. Neurochirurgie. 2025. 71: 101620
20. Park HW, Park KS, Park MS, Kim SM, Chung SY, Lee DS. The comparisons of surgical outcomes and clinical characteristics between the far lateral lumbar disc herniations and the paramedian lumbar disc herniations. Korean J Spine. 2013. 10: 155-9
21. Pavlović T, Štefančić K, Rožanković M, Boban L, Borić I, Molnar V. Ventrolateral disc herniation causes psoas muscle compression: A case report. Radiol Case Rep. 2019. 15: 136-40
22. Pojskic M, Bisson E, Oertel J, Takami T, Zygourakis C, Costa F. Lumbar disc herniation: Epidemiology, clinical and radiologic diagnosis WFNS spine committee recommendations. World Neurosurg X. 2024. 22: 100279
23. Porchet F, Chollet-Bornand A, De Tribolet N. Long-term follow up of patients surgically treated by the far-lateral approach for foraminal and extraforaminal lumbar disc herniations. J Neurosurg. 1999. 90: 59-66
24. Suess O, Brock M, Kombos T. Motor nerve root monitoring during percutaneous transforaminal endoscopic sequestrectomy under general anesthesia for intra-and extraforaminal lumbar disc herniation. Zentralbl Neurochir. 2005. 66: 190-201
25. Tschugg A, Tschugg S, Hartmann S, Rhomberg P, Thomé C. Far caudally migrated extraforaminal lumbosacral disc herniation treated by a microsurgical lateral extraforaminal transmuscular approach: Case report. J Neurosurg Spine. 2016. 24: 385-8
26. Uy BR, Sun MZ, Muftuoglu Y, Cheng M, Kim WJ, Magaki S. Upper lumbar spine far lateral disc herniations masquerading as peripheral nerve sheath tumors: Illustrative cases. J Neurosurg Case Lessons. 2023. 5: CASE22552
27. Wallace EC. Extreme lateral lumbar disc herniation. Ulster Med J. 1989. 58: 91-3
28. Yokosuka J, Oshima Y, Kaneko T, Takano Y, Inanami H, Koga H. Advantages and disadvantages of posterolateral approach for percutaneous endoscopic lumbar discectomy. J Spine Surg. 2016. 2: 158-66