- Department of Neurosurgery, Santa Maria delle Grazie Hospital, Pozzuoli, Italy
- Department of Neuroscience and Reproductive and Dental Sciences, Division of Neurosurgery A.O.U. Federico II, Napoli, Italy,
- Plastic Surgery Unit, A.O.U. Federico II, Napoli, Italy.
Correspondence Address:
Ciro Mastantuoni
Plastic Surgery Unit, A.O.U. Federico II, Napoli, Italy.
DOI:10.25259/SNI_351_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Claudio Schonauer1, Ciro Mastantuoni2, Oreste de Divitiis2, Francesco D’Andrea3, Raffaele de Falco1, Fabrizio Schonauer3. Pericranial and scalp rotation flaps for occipitocervical hardware exposure with CSF leak in rheumatoid arthritis patient: A case report and review of the literature. 17-May-2021;12:229
How to cite this URL: Claudio Schonauer1, Ciro Mastantuoni2, Oreste de Divitiis2, Francesco D’Andrea3, Raffaele de Falco1, Fabrizio Schonauer3. Pericranial and scalp rotation flaps for occipitocervical hardware exposure with CSF leak in rheumatoid arthritis patient: A case report and review of the literature. 17-May-2021;12:229. Available from: https://surgicalneurologyint.com/surgicalint-articles/10810/
Abstract
Background: There are several etiologies of craniocervical junction instability (CCJI); trauma, rheumatoid arthritis (RA), infections, tumors, congenital deformity, and degenerative processes. These conditions often require surgery and craniocervical fixation. In rare cases, breakdown of such CCJI fusions (i.e., due to cerebrospinal fluid [CSF] leaks, infection, and wound necrosis) may warrant the utilization of occipital periosteal rescue flaps and scalp rotation flaps to achieve adequate closure.
Case Description: A 33-year-old female with RA, cranial settling, and high cervical cord compression underwent an occipitocervical instrumented C0–C3/C4 fusion. Two months later, revision surgery was required due to articular screws pull out, CSF leakage, and infection. At the second surgery, the patient required screws removal, the application of laminar clamps, and sealing the leak with fibrin glue. However, the CSF leak persisted, and the skin edges necrosed leaving the hardware exposed. The third surgery was performed in conjunction with a plastic surgeon. It included operative debridement and covering the instrumentation with a pericranial flap. The resulting cutaneous defect was then additionally reconstructed with a scalp rotation flap. Postoperatively, the patient adequately recovered without sequelae.
Conclusion: A 33-year-old female undergoing an occipitocervical fusion developed a postoperative persistent CSF leak, infection, and wound necrosis. This complication warranted the assistance of plastic surgery to attain closure. This required an occipital periosteal rescue flap with an added scalp rotation flap.
Keywords: Craniocervical junction, Occipitocervical fusion, Pericranial flap, Rheumatoid arthritis, Skin rotation flap
INTRODUCTION
Rheumatoid arthritis (RA) involves the cervical spine in 59–88% of cases and can result in cranial settling (CS)/basilar invagination (BI), retro-odontoid pannus formation, atlantoaxial instability, and atlantoaxial subluxation. The typical treatment for RA-related CS is a posterior occipitocervical fusion.[
CASE REPORT
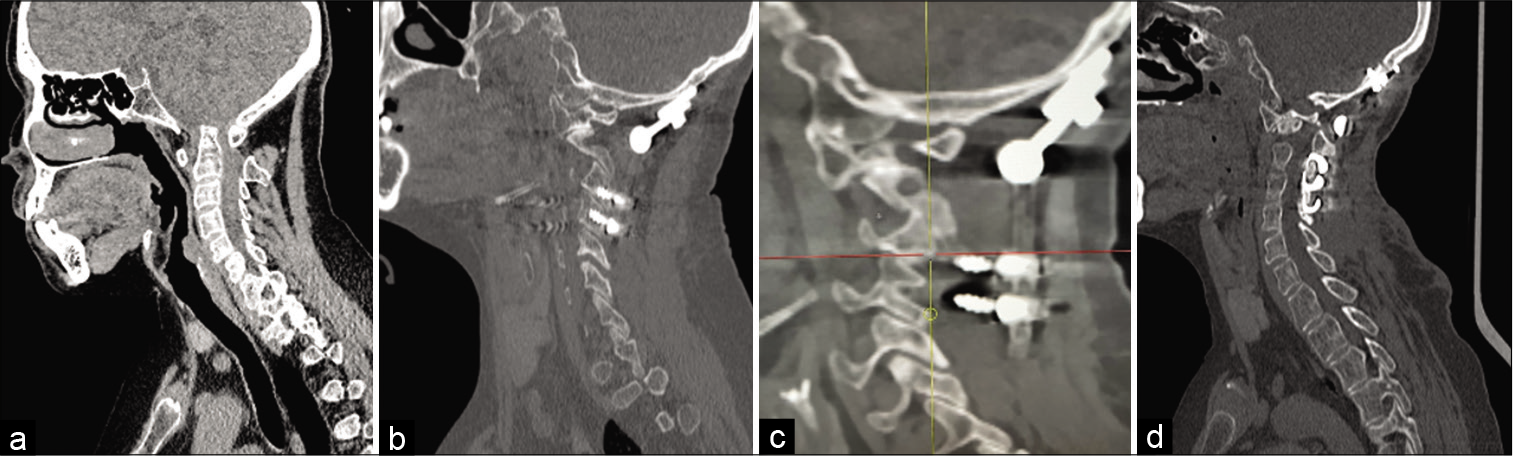
A 33-year-old female with RA presented with myelopathy. MR and CT studies documented BI, CCJI, and spinal cord compression [
Figure 1:
(a) Preoperative CT scan showing basilar invagination. (b) CT scan showing occipitocervical fusion with occipital plate screwed to the occipital bone and four screws inserted bilaterally in dysmorphic articular masses of C3 and C4. (c) C3 and C4 screws pull out. (d) CT scan performed after the second surgery: cervical articular screws were taken out and laminar clamps added to C3 and C4 laminae bilaterally.
However, 2 months later, she returned with paresthesias in both hands. The CT scan now showed pull-out of the cervical articular screws [
The second surgery included removal of the articular screws and the application of bilateral C0–C3/C4 laminar clamps [
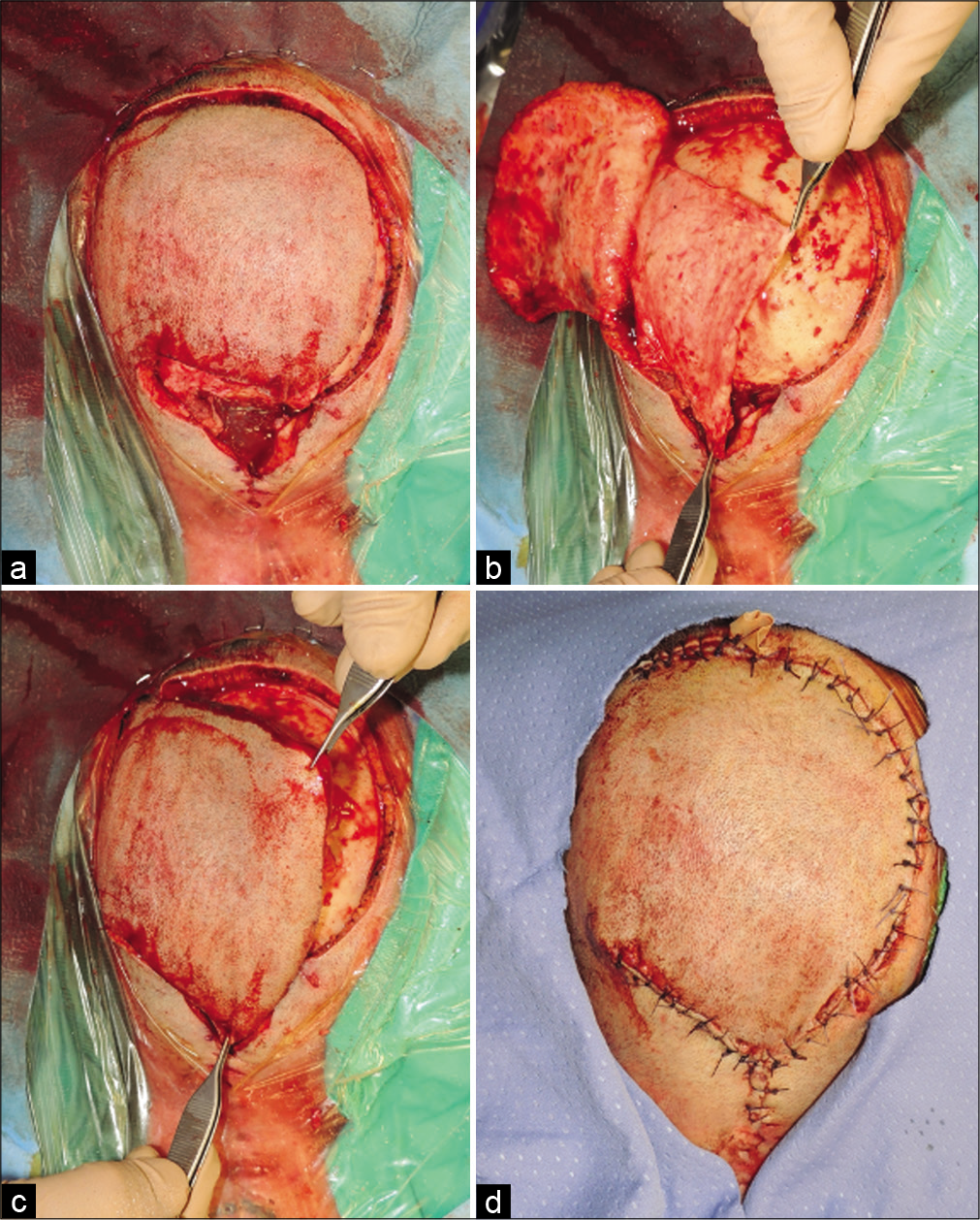
Figure 3:
(a) A left pedicled, rotation scalp flap was performed adjacent to the expected defect, large enough to allow its edges to comfortably inset into the skin defect. The margins of the flap were incised down to the pericranium. (b) The flap was raised in the avascular subgaleal plane and the pericranial rotation flap was elevated and rotated over the hardware. (c) The flap, including skin and galea, was elevated over the pericranium and rotated to reach the defect without tension. (d) Penrose drain was placed exiting at the cranial extremity of the wound.
DISCUSSION
RA patients have cervical spine involvement in up to 85% of cases, and CS/BI is one of the most frequent complications. Its treatment typically involves occipitocervical fusions, complications of which may include dural tears/CSF leakage, improper screw placement/instrumentation failure, and infections.[
Further, RA patients have an underlying compromised inflammatory autoimmune status, leaving them more susceptible to postsurgical infections, delayed healing, wound dehiscence, fusion failure, and CSF leaks/DT.[
If such complications arise, they may require complex occipitocervical wound/fusion revisions.
Rotation of complex occipitocervical flaps with plastic surgery
Coverage of exposed occipitocervical wound dehiscence may warrant the rotation of complex flaps in conjunction with plastic surgery.
Koop et al. proposed using a periosteal turndown flap and subsequent fixation through the flap with wires, screws, hooks, or plates to aid fusion; this technique has been successfully used over the years.[
Our modification was to rotate both skin and pericranial flaps down, and to drape these over the instrumentation. This offered a double-layer barrier for preventing recurrent CSF leakage, separated the occipital plate from the skin, reduced the wound pressure, and improved vascularization to the surrounding tissues.[
CONCLUSION
Occipitocervical instrumented fusion dehiscence can be successfully treated with a combination of scalp and pericranial rotation flaps utilized to cover the exposed instrumentation.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Casey AT, Crockard HA, Dickman CA, Spetzler RF, Sonntag VK.editors. Rheumatoid arthritis. Surgery of the Craniovertebral Junction. New York: Thieme; 1998. p. 151-74
2. Das KK, Pandey S, Gupta S, Behari S, Tessitore E, Dehdashti AR, Schonauer C, Thome C.editors. Rheumatoid cervical myelopathy. Surgery of the Cranio-Vertebral Junction. Berlin: Springer; 2020. p.
3. Fields MW, Lee NJ, Hong DY, Para A, Boddapati V, Mathew J. Cervical spinal fusion in adult patients with rheumatoid arthritis: A national analysis of complications and 90-day readmissions. Spine (Phila Pa 1976). 2021. 46: E23-30
4. Fleury G, Mania S, Hannouche D, Gabay C. The perioperative use of synthetic and biological disease-modifying antirheumatic drugs in patients with rheumatoid arthritis. Swiss Med Wkly. 2017. 147: w14563
5. Koop SE, Winter RB, Lonstein JE. The surgical treatment of instability of the upper part of the cervical spine in children and adolescents. J Bone Joint Surg Am. 1984. 66: 403-11
6. Schonauer F, Abbate V, Orabona GD, Salzano G, Sbordone C, Bonavolontà P. Hand Doppler flowmetry for surgical planning of pedicled flap in extensive full-thickness scalp reconstruction. Surg Oncol. 2020. 32: 49-56
7. Yasmeh S, Quinn A, Harris L, Sanders AE, Sousa T, Skaggs DL. Periosteal turndown flap for posterior occipitocervical fusion: A technique review. Eur Spine J. 2017. 26: 2303-7