- Department of Neurosurgery, Ina Central Hospital, Nagano, Japan
Correspondence Address:
Toshihiro Ogiwara, Department of Neurosurgery, Ina Central Hospital, Nagano, Japan.
DOI:10.25259/SNI_856_2024
Copyright: © 2025 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Toshihiro Ogiwara, Atsushi Sato, Kotaro Nakamura, Mana Wakabayashi, Tetsuo Sasaki, Yoshiki Hanaoka, Kazuhiro Hongo. Perioperative management of craniopharyngioma resection through endoscopic endonasal approach in a super-super obese patient: A technical case report. 10-Jan-2025;16:11
How to cite this URL: Toshihiro Ogiwara, Atsushi Sato, Kotaro Nakamura, Mana Wakabayashi, Tetsuo Sasaki, Yoshiki Hanaoka, Kazuhiro Hongo. Perioperative management of craniopharyngioma resection through endoscopic endonasal approach in a super-super obese patient: A technical case report. 10-Jan-2025;16:11. Available from: https://surgicalneurologyint.com/surgicalint-articles/13322/
Abstract
Background: The endoscopic endonasal approach (EEA) is increasingly used in minimally invasive surgeries for skull base lesions such as pituitary tumors. Although experienced facilities and neurosurgeons familiar with this technique can typically perform these surgeries routinely without special techniques or instruments, challenging cases can occasionally arise due to patient factors such as obesity. Here, we describe challenges encountered during neurosurgery in a patient with super-super obesity and introduce our unique technical nuances for management during tumor resection.
Case Description: We report about a 47-year-old man with a body mass index of 62.24 kg/m2 who presented for neurosurgery with a diagnosis of craniopharyngioma, for which tumor resection using the EEA under general anesthesia was performed. While planning tumor resection using the EEA, several limitations due to extreme obesity were encountered as follows: (1) management of the respiratory and circulatory systems under general anesthesia, (2) non-feasible positioning on a standard operating table, and (3) complications with lumbar drain (LD) replacement to prevent post-operative cerebrospinal fluid leakage. These challenges were overcome through (1) multidisciplinary collaboration with anesthesiologists and cardiologists, (2) the set-up of two operating tables side by side, and (3) LD placement under awake status in the sitting position, respectively. With these innovations, total tumor resection was achieved using the EEA.
Conclusion: This case highlights the successful use of the EEA along with unique technical adaptations in a super-super obese patient with craniopharyngioma, demonstrating the importance of innovation and problem-solving in overcoming surgical challenges.
Keywords: Craniopharyngioma, Endoscopic endonasal approach, Lumbar drainage, Obese patient, Surgical setting
INTRODUCTION
The endoscopic endonasal approach (EEA) to the skull base is essential for comprehensive surgery of skull base lesions, including pituitary tumors, craniopharyngiomas, and meningiomas.[
Obesity is associated with increased morbidity and mortality, and its increasing incidence has significant implications for healthcare, with super-super obese (body mass index [BMI] >60 kg/m2) patients having an even greater risk.[
Lifestyle changes and associated endocrine dysfunction, including acromegaly and Cushing’s disease, have led to increased numbers of super/super-super obese patients requiring neurosurgery. Extending the EEA in extremely obese patients in daily clinical practice requires technical innovations. Therefore, neurosurgeons should consider the technical nuances of endoscopic endonasal surgery in such patients. Herein, we describe the challenges encountered during neurosurgery in a patient with super-super obesity and introduce our unique technical nuances for management during tumor resection.
CASE DESCRIPTION
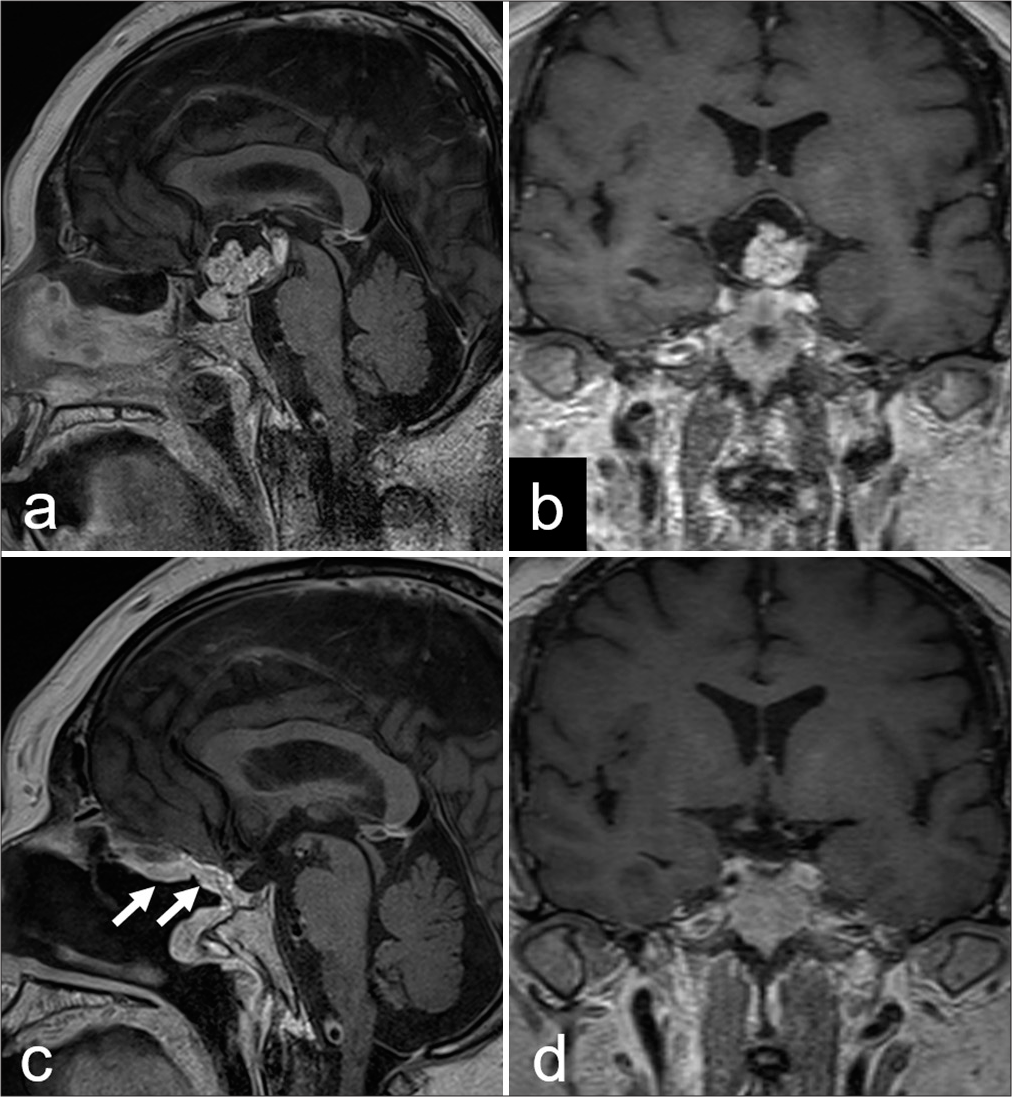
This study was approved by the Ina Central Hospital Ethics Committee (approval number: 24-2), and informed consent was obtained from the patient. A 47-year-old man with super-super obesity (height, 176.0 cm; body weight, 192.8 kg; BMI, 62.24 kg/m2) experienced headaches and progressive blurred vision. Neuroimaging revealed a suprasellar tumor (maximum diameter, 35 mm) compressing the optic chiasma, suggestive of craniopharyngioma [
Figure 1:
(a) Contrast-enhanced sagittaland (b) coronal magnetic resonance imaging (MRI) scans obtained before the endoscopic endonasal approach (EEA), showing the heterogeneously enhancing suprasellar mass with optic chiasma compression. The post-EEA MRI scan shows (c and d) gross total tumour resection with decompression of the optic apparatus and complete reconstruction of the skull base using a well-enhanced pedicled nasoseptal flap (arrow).
Positioning is challenging in patients with morbid obesity due to gravity-induced overhanging of the subcutaneous fat on the operating table with the usual positioning for the EEA. To resolve this issue, two operating tables were joined, with one table equipped with a four-pin head fixation system (Sugita Head Holder; Mizuho, Tokyo, Japan) [
Figure 4:
Operating room photographs showing (a and b) the use of the four-pin head fixation system to tilt the head to the left and rotate it to the right to allow a convenient position and direct good view through the nostrils for the surgeon standing on the right side of the patient looking cranially.
Some factors, including cardiovascular strain, respiratory issues, medication dosing, and thrombosis risk, collectively contribute to increased postoperative risk in obese patients, necessitating diligent postoperative care. Therefore, anesthesiologists and cardiologists provided postoperative respiratory and circulatory management in the intensive care unit, and no complications or adverse events were observed during emergence from anesthesia and extubation. Postoperatively, the patient’s visual function improved significantly. An LD was inserted for 3 days after surgery, and no postoperative CSF leaks occurred. Hormone replacement therapy was administered for hypopituitarism. Precise multidisciplinary perioperative management allowed for successful surgery. The patient consented to the publication of his image.
DISCUSSION
The World Health Organization defines adult obesity as a BMI ≥30 kg/m2, and additional classifications include severe, super, and super-super obesity (BMI ≥40, ≥50, and ≥60 kg/m2, respectively).[
Respiratory and circulatory system management during anesthesia
General anesthesia induction in patients with extreme obesity requires careful planning owing to the unique physiological challenges. The primary anesthetic concern in preoperative assessment is the patient’s airway. The excess neck tissue limits the range of motion, complicating proper and safe intubation. Direct laryngoscopy is associated with increased risks of intubation failure in patients with extreme obesity; these patients also desaturate quickly, which is a crucial and dangerous consideration.[
Operating table positioning
Optimal patient positioning is crucial in any surgical workflow, particularly endoscopic endonasal surgery.[
LD placement
Various skull base reconstruction techniques have been developed for using the EEA in skull base lesions to prevent postoperative CSF leakage, which may lead to meningitis and tension pneumocephalus.[
CONCLUSION
We present the technical nuances of the EEA for patients with super-super-obesity and highlight our experience in successfully performing endoscopic endonasal surgery in a patient with craniopharyngioma, demonstrating the importance of innovation and problem-solving in overcoming surgical challenges. Adequate multidisciplinary preoperative preparation, anticipation of problems, and preparedness to circumvent complications are mandatory for successful neurosurgery in patients with extreme obesity.
Ethical approval
The Institutional Review Board approved the research/study at the Ina Central Hospital Ethics Committee, number approval number 24-2, dated April 11, 2024.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Bahar M, Chanimov M, Cohen ML, Friedland M, Shul I, Gofman V. The lateral recumbent head-down position decreases the incidence of epidural venous puncture during catheter insertion in obese parturients. Can J Anaesth. 2004. 51: 577-80
2. Bray GA. Pathophysiology of obesity. Am J Clin Nutr. 1992. 55: 488S-94
3. Cohen S, Jones SH, Dhandapani S, Negm HM, Anand VK, Schwartz TH. Lumbar drains decrease the risk of postoperative cerebrospinal fluid leak following endonasal endoscopic surgery for suprasellar meningiomas in patients with high body mass index. Oper Neurosurg (Hagerstown). 2018. 14: 66-71
4. CRANIAL Consortium. The impact of obesity on rates of postoperative CSF leak following endoscopic skull base surgery: Results from a prospective international multi-centre cohort study. Front Endocrinol (Lausanne). 2024. 15: 1353494
5. Ekanayake J, Baudracco I, Quereshi A, Vercauteren T, Dorward NL. The conversational position in endoscopic pituitary surgery. Br J Neurosurg. 2018. 32: 44-6
6. Jamshidi AM, Shah A, Eichberg DG, Komotar RJ, Ivan M. Conservative management of post-operative cerebrospinal fluid leak following skull base surgery: A pilot study. Brain Sci. 2022. 12: 152
7. Kaye AD, Lingle BD, Brothers JC, Rodriguez JR, Morris AG, Greeson EM. The patient with obesity and super-super obesity: Perioperative anesthetic considerations. Saudi J Anaesth. 2022. 16: 332-8
8. Kilgallon JL, Thorne A, Laws ER. The hitchhiker position in endoscopic pituitary surgery. Oper Neurosurg (Hagerstown). 2022. 23: 427-30
9. Lavigne P, Wang EW, Gardner PA, Snyderman CH. From research to clinical practice: Long-term impact of randomized clinical trial examining the effect of lumbar drains on cerebrospinal fluid leak rates following endonasal skull base surgery. J Neurol Surg B Skull Base. 2021. 83: 339-42
10. Ogiwara T, Kitamura S, Goto T, Fujii Y, Yamazaki K, Kuwabara H. The efficacy of a visiting surgical service versus that of a hospital-based surgical service in providing endoscopic endonasal surgery to remove nonfunctioning pituitary adenomas in rural communities. Pituitary. 2023. 26: 521-8
11. Ogiwara T, Nagm A, Hasegawa T, Hanaoka Y, Ichinose S, Goto T. Pitfalls of skull base reconstruction in endoscopic endonasal approach. Neurosurg Rev. 2019. 42: 683-9
12. Suresh S, Hrishi AP, Arumadi A, Praveen R. Challenges of super-super obese patient presenting for neurosurgery: A case-based review. J Neuroanaesth Crit Care. 2024. 11: 126-9
13. Xu JC, Hanna G, Fong BM, Hsu FP, Cadena G, Kuan EC. Ergonomics of endoscopic skull base surgery: A systematic review. World Neurosurg. 2021. 146: 150-5