- Department of Neurosurgery, Centro Medico “Lic. Adolfo López Mateos”, Instituto de Salud del Estado de México, Av. Nicolás San Juan s/n Ex Hacienda La Magdalena, Toluca - 50010, Estado de México, México.
DOI:10.25259/SNI_305_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Saúl Solorio-Pineda, César Adán Almendárez-Sánchez, Abrahan Alfonso Tafur-Grandett, Gabriel Arturo Ramos-Martínez, Raúl Huato-Reyes, Milton Inocencio Ruiz-Flores, Antonio Sosa-Najera. Pituitary macroadenoma apoplexy in a severe acute respiratory syndrome-coronavirus-2-positive testing: Causal or casual?. 25-Sep-2020;11:304
How to cite this URL: Saúl Solorio-Pineda, César Adán Almendárez-Sánchez, Abrahan Alfonso Tafur-Grandett, Gabriel Arturo Ramos-Martínez, Raúl Huato-Reyes, Milton Inocencio Ruiz-Flores, Antonio Sosa-Najera. Pituitary macroadenoma apoplexy in a severe acute respiratory syndrome-coronavirus-2-positive testing: Causal or casual?. 25-Sep-2020;11:304. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=10289
Abstract
Background: In December 2019, in Wuhan, a new virus emerged, causing severe acute respiratory syndrome (SARS) secondary to infection by a type of coronavirus, causing coronavirus disease (COVID-19). The pandemic caused by the new coronavirus has had implications in the central nervous system. COVID-19 is known to be characterized by coagulation activation and endothelial dysfunction, causing ischemic and hemorrhagic vascular syndromes.
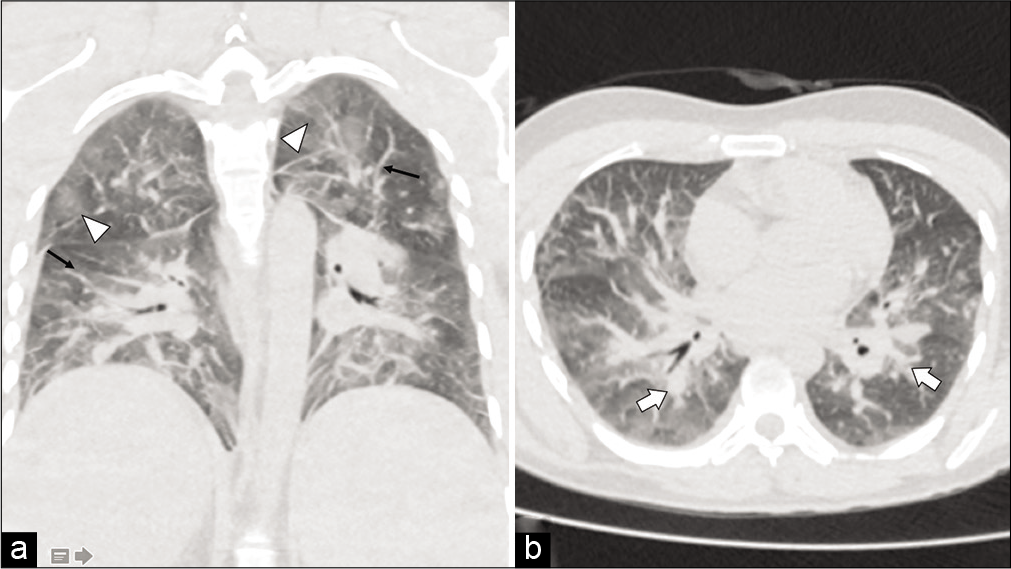
Case Description: A 27-year-old male patient case with progressive decrease in visual acuity, associated with respiratory symptoms and intense headache. Multilobar infiltrate with a reticulonodular pattern is evident on chest CT scan. Brain CT scan with pituitary macroadenoma apoplexy was shown. SARS-Cov2 was confirmed, and respiratory support initiated. However, the patient died shortly afterward, secondary to pulmonary complications.
Conclusion: The angiotensin-converting enzyme (ACE) II receptor is expressed in circumventricular organs and in cerebrovascular endothelial cells, which play a role in vascular autoregulation and cerebral blood flow. For this reason, is rational the hypothesize that brain ACE II could be involved in COVID-19 infection. Underlying mechanisms require further elucidation in the future.
Keywords: Adenoma apoplexy, Case report, Coronavirus disease-19, Severe acute respiratory syndrome
INTRODUCTION
A new virus emerged, causing severe acute respiratory syndrome (SARS) originated in the city of Wuhan, China, in December 2019. The cause of this syndrome was a new coronavirus, and it was subsequently declared a global pandemic.[
Pituitary tumor apoplexy is a rare syndrome characterized by hemorrhage or infarction from a preexisting pituitary adenoma.[
Adenoma size seems to be the most critical factor; therefore, macroadenomas have a higher risk of stroke.[
We decided to present the following remarkable case from a patient with pituitary tumor apoplexy infected with SARS-CoV-2.
CLINICAL CASE
We present the case of a 27-year-old male patient, with unremarkable medical history who started 6 months before admission with a progressive decrease in visual acuity in both eyes and left exotropia without receiving management. Six days before admission, he presented with asthenia, adynamia, and fever, referring self-medication with ibuprofen. Two days before admission, he suddenly presents with a frontal headache and disorientation. Then, drowsiness and respiratory distress are added. On physical examination, we found bilateral lung consolidation syndrome, 80% oxygen saturation with intercostal retraction and nasal flutter. The neurological examination with global aphasia, in Glasgow of 11 points (O3, V2, and M6), the right pupil with a diameter of 6 mm and the left pupil with a diameter of 3 mm, decreased response to light and left eye exotropia.
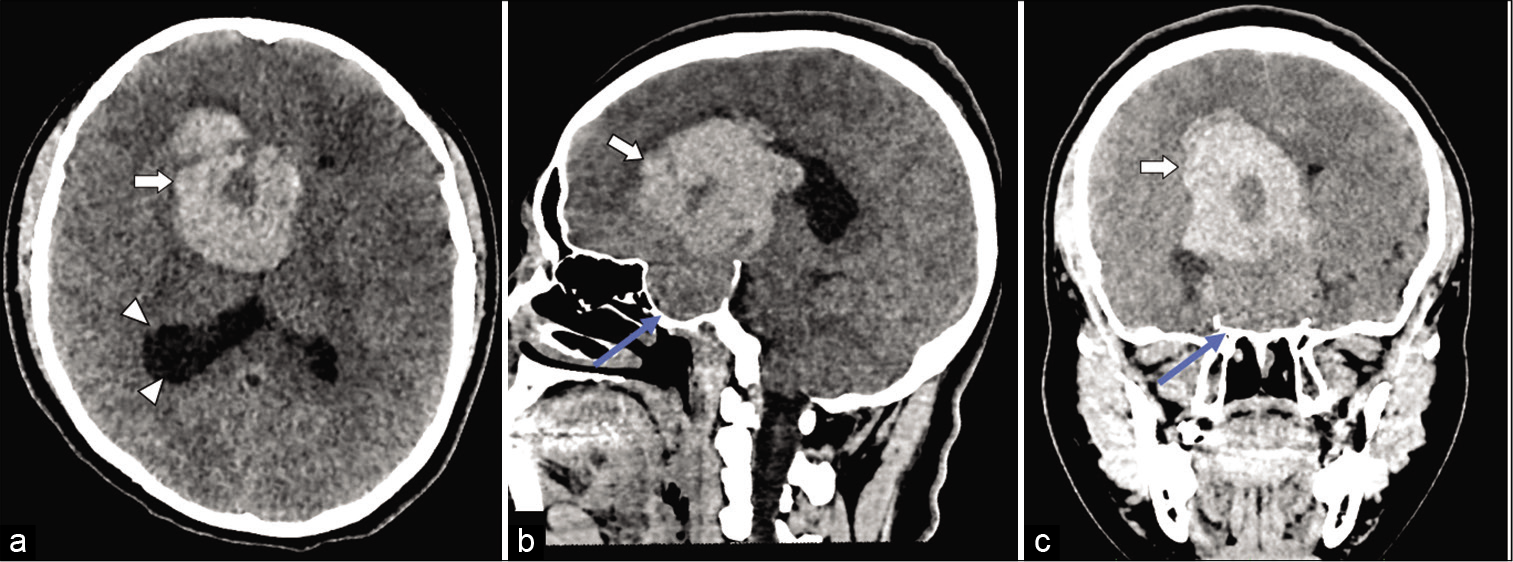
A brain CT scan [
Figure 1:
Simple head CT scan obtained from axial plane (a), sagittal plane (b), and coronal plane (c). Heterogeneous tumor lesion of the sellar region is observed, with maximum dimensions of 59 × 52 × 68 mm (white arrow), causing widening of the sella turcica (blue arrow), with a hyperdense area compatible with tumor hemorrhage, causing collapse of the third ventricle and dilation of the occipital horn of the right lateral ventricle (arrowheads).
He was admitted with the diagnoses of pituitary macroadenoma apoplexy and atypical pneumonia. A PCR test for SARS-CoV-2 was performed, which turned positive. Pulmonary management was prioritized, given the presence of SARS. The patient presented a weak evolution of the respiratory function, requiring invasive mechanical ventilation, presenting with severe hypoxemia refractory to management in the critical care unit, and dying 12 h after hospital admission.
DISCUSSION
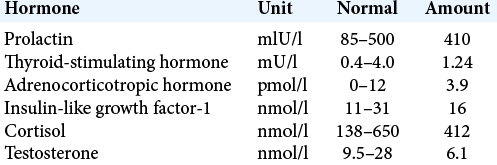
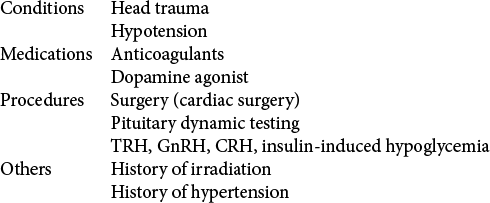
In our case, we talk about pituitary macroadenoma with stroke, and as discussed in the literature, these tumors have a higher risk of tumor stroke compared to other tumors. The main associated factor being their large size, other factors that are associated are those described by Nawar et al.[
Recent evidence suggests that the pathophysiology of COVID-19 may be related to the CNS. A retrospective study was carried out in China in which more than 200 patients participated, which revealed that they presented neurological symptoms, such as altered consciousness and even acute cerebrovascular disease (ACD).[
There is documented evidence about the presence of the SARS-CoV-2 virus in cerebrospinal fluid.[
Some authors report on the possibility of the virus to enter the brain through the nasopharyngeal epithelium. By taking the path of the olfactory nerve, the virus reaches the olfactory bulb and spreads further to other parts.[
It is proven that the SARS-CoV-2 virus infects cells by binding to the receptor for angiotensin-converting enzyme 2 (ACE-2).[
Ibuprofen was found to increase the number of ACE-2 receptors in the cell membrane. The interaction between ibuprofen and ACE-2 receptors increases the infectivity of the virus, increasing the probability of interaction between cells and the virus.[
CONCLUSION
The question that arises is whether COVID-19 infection was the cause of pituitary apoplexy or whether it is a coincidental event. The CNS involvement in COVID-19 infection includes cerebrovascular events due to endothelial dysfunction, with pituitary apoplexy being an unusual presentation, a situation that should be confirmed in the future.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Carod-Artal J. Neurological complications due to coronavirus and COVID-19. Rev Neurol. 2020. 70: 311-22
2. Chigr F, Merzouki M, Najimi M. Autonomic brain centers and pathophysiology of COVID-19. ACS Chem Neurosci. 2020. 11: 1520-2
3. Fang L, Karakiulakis G, Roth M. Are patients with hypertension and diabetes mellitus at increased risk for COVID-19 infection?. Lancet Respir Med. 2020. 8: e21
4. Li Y, Wang M, Zhou Y, Chang J, Xian Y, Mao L. Acute cerebrovascular disease following COVID-19: A single center, retrospective, observational study. Stroke Vasc Neurol. 2020:
5. Mao L, Jin H, Wang M, Hu Y, Chen S, He Q. Neurologic manifestations of hospitalized patients with Coronavirus disease 2019 in Wuhan, China. JAMA Neurol. 2020. 77: 1-9
6. Mohanty S, Tandon PN, Banerji AK, Prakash B. Haemorrhage into pituitary adenomas. J Neurol Neurosurg Psychiatry. 1977. 40: 987-91
7. Moriguchi T, Harii N, Goto J, Harada D, Sugawara H, Takamino J. A first case of meningitis/encephalitis associated with SARS-Coronavirus-2. Int J Infect Dis. 2020. 94: 55-8
8. Nawar RN, AbdelMannan D, Selman WR, Arafah BM. Pituitary tumor apoplexy: A review. J Intensive Care Med. 2008. 23: 75-90
9. Rolih CA, Ober KP. Pituitary apoplexy. Endocrinol Metab Clin North Am. 1993. 22: 291-302
10. Zhou Z, Kang H, Li S, Zhao X. Understanding the neurotropic characteristics of SARS-CoV-2: From neurological manifestations of COVID-19 to potential neurotropic mechanisms. J Neurol. 2020. 267: 2179-84
11. Zhu N, Zhang D, Wang W, Li X, Yang B, Song J. A novel coronavirus from patients with pneumonia in China 2019. N Engl J Med. 2020. 382: 727-33