- Department of Medicine, Federal University of Sergipe, Aracaju, Brazil
- Department of Neurosurgery, Hospital de Cirurgia, Aracaju, Brazil
- Graduate Program in Health Sciences (PPGCS), Federal University of Sergipe, Aracaju, Brazil
Correspondence Address:
Arthur Maynart Pereira Oliveira, Department of Neurosurgery, Hospital de Cirurgia, Aracaju, Brazil.
DOI:10.25259/SNI_724_2024
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Lucas Costa Almeida1, Alice Caroline Alves da Silva1, Matheus Assis de Almeida2, Paulo Eduardo Gonçalves1, Arthur Maynart Pereira Oliveira1,2,3. Pons herniation after skull base chondrosarcoma surgery: A rare complication after transclival endoscopic endonasal approach. 06-Dec-2024;15:451
How to cite this URL: Lucas Costa Almeida1, Alice Caroline Alves da Silva1, Matheus Assis de Almeida2, Paulo Eduardo Gonçalves1, Arthur Maynart Pereira Oliveira1,2,3. Pons herniation after skull base chondrosarcoma surgery: A rare complication after transclival endoscopic endonasal approach. 06-Dec-2024;15:451. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=13270
Abstract
Background: Intracranial chondrosarcomas are malignant tumors that most commonly affect the clivus region. For tumors in this location, the extended endoscopic endonasal approach could offer an alternative route. We present a case of pons herniation after this technique.
Case Description: A 55-year-old female presented with a 6-month history of difficulty walking. The neurological evaluation showed asymmetric tetra paresis and involvement of the IX cranial nerve on the right side. Imaging exams showed a lesion at the upper clivus, with a possible diagnosis of chondrosarcoma. An extended transclival approach with partial resection and a multilayer closure were performed. The patient had a slight immediate improvement in muscle strength, and she was discharged home 5 days after surgery. Four weeks later, she evolved with worsening strength on the left side. A new image examination revealed an atypical protrusion of the pontine tissue through the bone defect at the opening of the clivus; a surgical revision was proposed, but the patient chose conservative management.
Conclusion: Pontine herniation is a rare complication with no defined cause. The use of a rigid material for closure could reduce the chances of this complication, but futher studies are necessary to reinforce that hypothesis.
Keywords: Case report, Chondrosarcoma, Complications, Endoscopic endonasal approach, Skull base tumors
INTRODUCTION
Intracranial chondrosarcomas are malignant tumors originating from chondroid cells that generally affect the clivus region and, specifically, the temporo-occipital region.[
The Endonasal endoscopic approach (EEA) for skull base surgeries has advanced with the evolution of the technique and the expansion of anatomical knowledge.[
In this paper, we present our only case of pons herniation. This complication happened following surgery for chondrosarcoma through a transclival endonasal endoscopic route conducted in a philanthropic hospital in the state of Sergipe, Brazil.
CASE REPORT
We present a 55-year-old female patient with class I obesity, no other comorbidities, no prescribed medication in use, and difficulty walking for approximately 6 months. A neurologist initially consulted her because of tetraparesis symptoms. The patient had a cranial computed tomography (CT) and magnetic resonance imaging (MRI) done. After examinations, the neurologist referred her to the neurosurgery service. In the initial neurological examination, the patient presented with asymmetric tetraparesis. Strength measured grade 3 on the right and grade 4 on the left, associated with global exalted deep reflexes. In addition, she had episodes of dysphagia with liquids showing signs of mild paresis of the IX cranial nerve on the right.
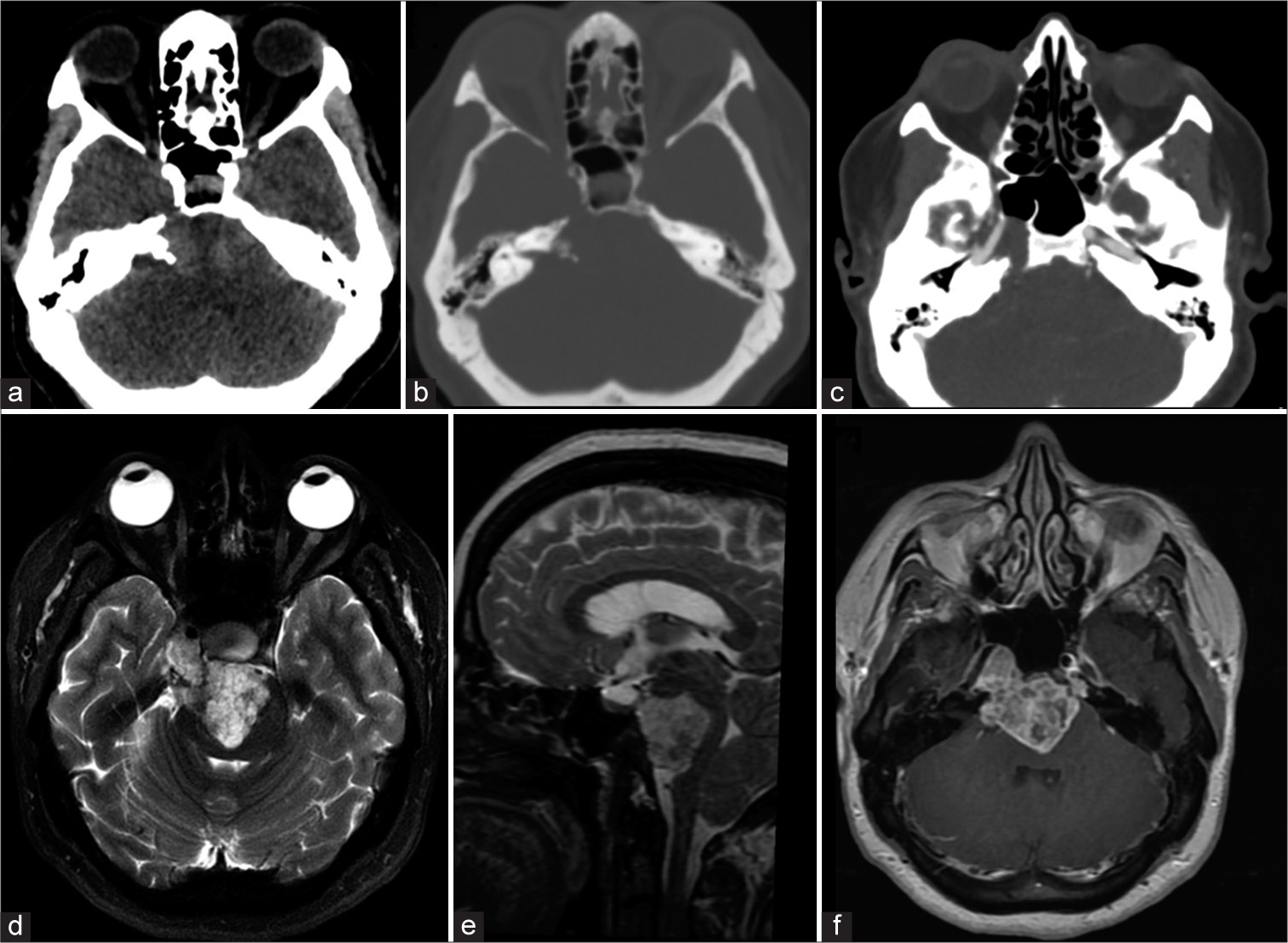
The CT showed a lesion located medially behind the clivus, occupying the middle and lower third of it, with a similar density to the brain parenchyma [
Figure 1:
Preoperative images showing in (a) the preoperative axial brain computed tomography (CT) with an isodense prepontine lesion, with (b) indications of extension and destruction of the anterior petrous bone. In (c), a brain angiography CT demonstrates the relationship of the tumor with the right internal carotid, with lateral and superior displacement of the artery in the petrous and para clival segment. In (d and e), an axial and sagittal T2-weighted magnetic resonance imaging (MRI) shows a heterogeneous mass with hypo signal lesion, huge displacement of the pons, and invasion of the petrous apex. In (f), a T1-weighted postgadolinium axial MRI shows a heterogenous contrast enhancement and a possible route for the endoscopic endonasal approach with the displacement of the right internal carotid.
After general anesthesia, we positioned the patient in a horizontal supine position with a 3 points-Mayfield fixation and neurophysiological monitoring of cranial nerves and motor and somatosensitive potentials. The position is like that used in pituitary surgery, except for a greater flexion of the head to allow a better view of the clivus region. In addition, we exposed the lateral aspect of the right thigh to remove a free fascia lata graft and fat. After that, the otorhinolaryngology team exposed the entire sphenoid floor and also drilled the superior and middle clivus to allow exposure of the dura mater from the dorsum sellar region to the lower limit of the tumor. Greater right lateral exposure was possible due to the displacement of the para-clival carotid laterally and the petrous carotid on that side being more lateralized and displaced superiorly. We opened the dura mater medially in the craniocaudal direction, followed by central debulking of the lesion.
After resecting the center of the lesion, we performed a circumferential dissection allowing resection of the entire lesion from the petrous apex and the medial and left portions of the tumor. We were able to visualize and preserve all neurovascular structures as the basilar artery and VI nerve bilaterally by this access. However, the most superior portion of the tumor, at the transition between the para-clival carotid artery and cavernous sinus posterior segment, was not well visualized, and we decided not to remove it. We performed the closure of the skull base using the multilayers technique as in the following sequence: a layer of fat inside the cavity; free fascia lata graft internally to the dura mater; right pedicled nasoseptal flap, patches of gel foam, and a gauze pad moistened with antibiotic ointment. We removed the gauze pad 5 days after surgery. The patient presented no complications after surgery and a slight improvement in muscle strength on the right side of the body in the immediate postoperative period. We were able to discharge her after 5 days of surgery and continue to monitor her as an outpatient.
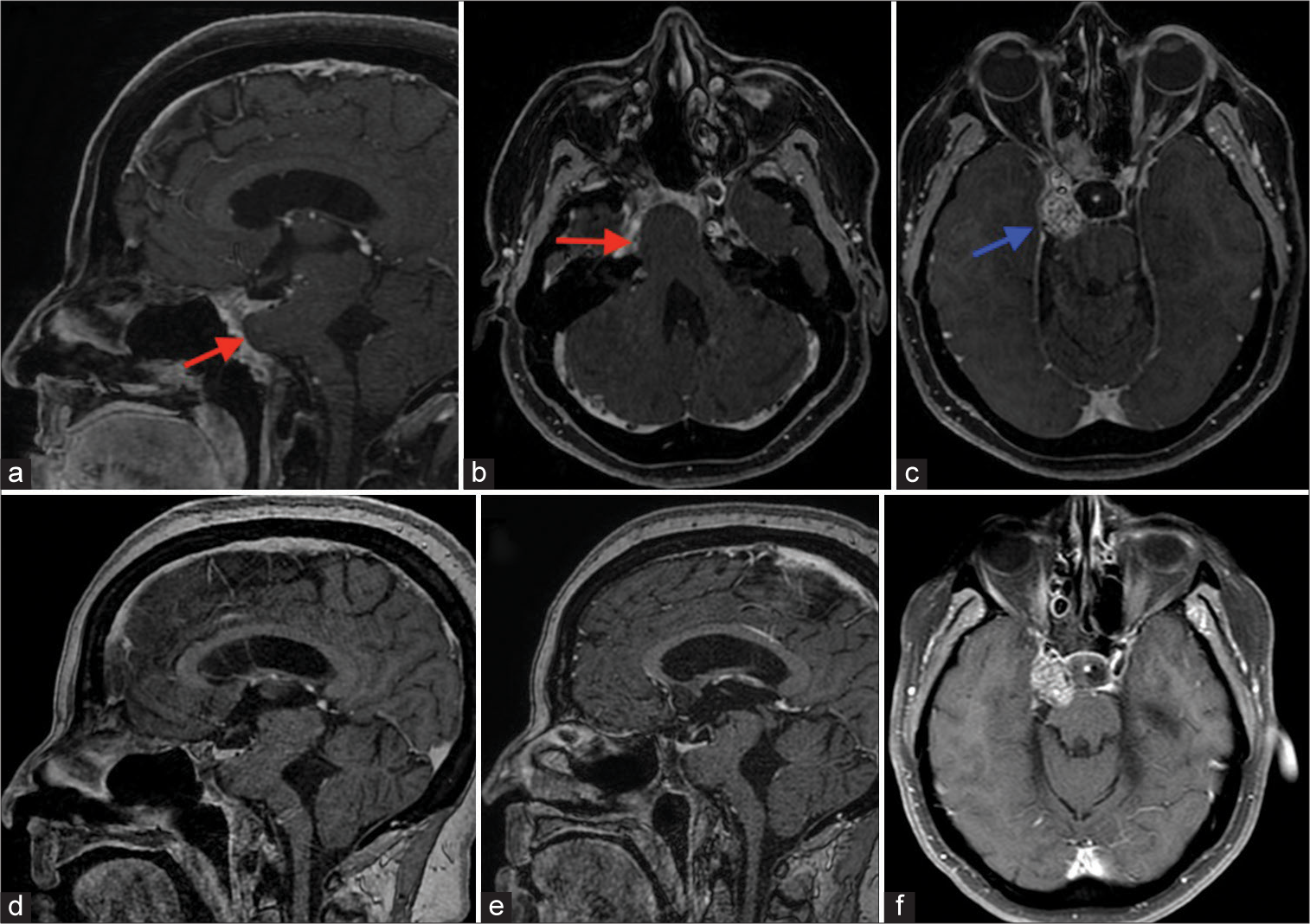
In the postoperative evaluation, 14 days after surgery, the patient began to report worsening strength on the left side in relation to the improvement obtained in the immediate postoperative period. We recommended intensifying physiotherapy sessions and advised that in case of worsening, return for evaluation. Four weeks after surgery, the patient returned to the clinic, presenting grade 3 tetraparesis, unable to walk. She had a new brain MRI done, and it showed an atypical protrusion of the pontine tissue through the bone defect at the opening of the clivus [
Figure 2:
Postoperative images. In (a and b), a T1-weighted postgadolinium sagittal and axial magnetic resonance imaging (MRI) shows the displacement of the pons into the clivus bone defect (red arrow). In (c), a more superior MRI slice shows a residual tumor inside the posterior compartment of the right cavernous sinus (blue arrow). In (d and e), follow-up MRI images of 1 and 2 years, respectively, show the same changes as the first postoperative MRI. In (f), it is possible to see after 2 years no growth of the residual tumor.
DISCUSSION
Endoscopic endonasal surgery has been introduced as a treatment option for anterior skull base tumors with favorable results. Sometimes, it is necessary to perform an extensive clival resection to obtain favorable margins for tumor resection and wide brainstem decompression in the EEA treatment for chondrosarcoma, chordomas, and meningiomas.[
Endonasal endoscopic approach closure techniques have improved significantly with the advent of vascularized flaps reducing complication rates.[
Transclival pons herniation is a rare complication and has no defined cause. As in meningoceles or encephaloceles, a transient increase in ICP may be a causal factor. Postsurgical encephaloceles have been associated with decompressive craniectomies and dural openings.[
As in other specialties, in anterior skull base surgery, there is a clear relationship between the surgeon’s level of experience and achieved results, often described as a “learning curve.”[
CONCLUSION
A pontine herniation is a rare complication of transclival endoscopic surgeries and has no defined cause. A rigid material closure could reduce the chances of this complication; nevertheless, it would be associated with other risks. We hope that future innovations in EEA and alternative techniques in endoscopic reconstruction of the anterior skull base will avoid such a complication.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Culebras D, Torales J, Reyes LA, Zapata L, García S, Roldán P. Extended endoscopic endonasal surgery for clival chordoma and chondrosarcoma: Our experience in 14 cases. Neurocirugia (Astur: Engl Ed). 2018. 29: 201-8
2. Honeybul S, Ho KM. Long-term complications of decompressive craniectomy for head injury. J Neurotrauma. 2011. 28: 929-35
3. Hopper AN, Jamison MH, Lewis WG. Learning curves in surgical practice. Postgrad Med J. 2007. 83: 777-9
4. Kasemsiri P, Prevedello DM, Otto BA, Old M, Ditzel Filho L, Kassam AB. Endoscopic endonasal technique: Treatment of paranasal and anterior skull base malignancies. Braz J Otorhinolaryngol. 2013. 79: 760-79
5. Koutourousiou M, Filho FV, Costacou T, Fernandez-Miranda JC, Wang EW, Snyderman CH. Pontine encephalocele and abnormalities of the posterior fossa following transclival endoscopic endonasal surgery. J Neurosurg. 2014. 121: 359-66
6. Koutourousiou M, Gardner PA, Tormenti MJ, Henry SL, Stefko ST, Kassam AB. Endoscopic endonasal approach for resection of cranial base chordomas: Outcomes and learning curve. Neurosurgery. 2012. 71: 614-24 discussion 624-5
7. Kuge A, Sato S, Sakurada K, Takemura S, Kikuchi Z, Saito Y. Technical notes on endoscopic transnasal transsphenoidal approach for clival chondrosarcoma. Sarcoma. 2011. 2011: 953047
8. Leng LZ, Brown S, Anand VK, Schwartz TH. “Gasket-seal” watertight closure in minimal-access endoscopic cranial base surgery. Neurosurgery. 2008. 62: ONSE342-3 discussion ONSE343
9. Palmisciano P, Haider AS, Sabahi M, Nwagwu CD, Bin Alamer O, Scalia G. Primary skull base chondrosarcomas: A systematic review. Cancers (Basel). 2021. 13: 5960
10. Ravnik J, Hribernik B, Lanišnik B. Endoscopic endonasal approaches to the clival region. Acta Med Acad. 2020. 49: 45-53
11. Shikary T, Andaluz N, Meinzen-Derr J, Edwards C, Theodosopoulos P, Zimmer LA. Operative learning curve after transition to endoscopic transsphenoidal pituitary surgery. World Neurosurg. 2017. 102: 608-12
12. Wong AK, Raviv J, Wong RH. Sellar trough technique for endoscopic endonasal transclival repair. Surg Neurol Int. 2020. 11: 99
13. Zanation AM, Carrau RL, Snyderman CH, Germanwala AV, Gardner PA, Prevedello DM. Nasoseptal flap reconstruction of high flow intraoperative cerebral spinal fluid leaks during endoscopic skull base surgery. Am J Rhinol Allergy. 2009. 23: 518-21