- Department of Neurosurgery, Mohammed V Faculty of Medicine and Pharmacy of Rabat, Military Teaching Hospital Mohammed V of Rabat, Morocco.
Correspondence Address:
Fresnel Lutèce Ontsi Obame, Department of Neurosurgery, Mohammed V Faculty of Medicine and Pharmacy of Rabat, Military Teaching Hospital Mohammed V of Rabat, Morocco.
DOI:10.25259/SNI_1030_2022
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Fresnel Lutèce Ontsi Obame, Yao Christian Hugues Dokponou, Jawad Laaguili, Mohamed Mouhssani, Moussa Elmi Saad, Abad Chérif El Asri, Miloudi Gazzaz. Positive outcome of nonoperative management of spinal cord compression by multiple myeloma: A case report. 13-Jan-2023;14:10
How to cite this URL: Fresnel Lutèce Ontsi Obame, Yao Christian Hugues Dokponou, Jawad Laaguili, Mohamed Mouhssani, Moussa Elmi Saad, Abad Chérif El Asri, Miloudi Gazzaz. Positive outcome of nonoperative management of spinal cord compression by multiple myeloma: A case report. 13-Jan-2023;14:10. Available from: https://surgicalneurologyint.com/surgicalint-articles/12103/
Abstract
Background: Spinal cord compression (SCC) is a severe consequence of multiple myeloma (MM). Surgical management is appropriate when there are spinal instability and neurological function compromise. The reversibility of peripheral neuropathy during treatment of MM has been reported in some studies after a cycle of Bortezomib (Velcade), Thalidomide, and Dexamethasone (VTD), but very rare in myeloma patients with SCC.
Case Description: We report a case of a 58-year-old male tetraplegic secondary to cervical SCC by MM who completely recovered after 5 cycles of VTD chemotherapy without surgery.
Conclusion: Surgical spinal cord decompression by laminectomy is known as the gold standard for treating this condition. Nevertheless, some patients can completely recover from nervous insult without surgery.
Keywords: Chemotherapy, Multiple myeloma, Spinal cord compression
INTRODUCTION
Spinal cord compression (SCC) is a devastating complication of multiple myeloma (MM). In a large population-based study, the incidence of SCC in newly diagnosed MM was 7.8%.[
The surgery may be necessary to correct instability and reduce movement-induced pain. If there is spinal instability, spinal surgery is the best way to relieve acute SCC.[
Even after surgery, a tetraplegic patient with important craniovertebral SCC is unlikely to recover from neurologic impairments and regain daily activities. Reversibility of peripheral neuropathy during the treatment of myeloma had been reported after cycles of Bortezomib (Velcade), Thalidomide, and Dexamethasone (VTD).[
We report the case of a MM patient with spinal instability and SCC, who was successfully treated by nonoperative means.
CASE REPORT
Patient information
A 58-year-old male was admitted on February 19, 2022, for a 3-week history of progressive upper and lower extremities weakness. Five months earlier, the patient described increasing pain in the neck. His medical history is unremarkable.
Clinical findings
Physical examination revealed a neurological deficit rated ASIA B. He had no dyspnea, and no bowel or bladder dysfunction. The patient had a Karnofsky Performance Score (KPS) estimated at 30%.
Diagnostic assessment
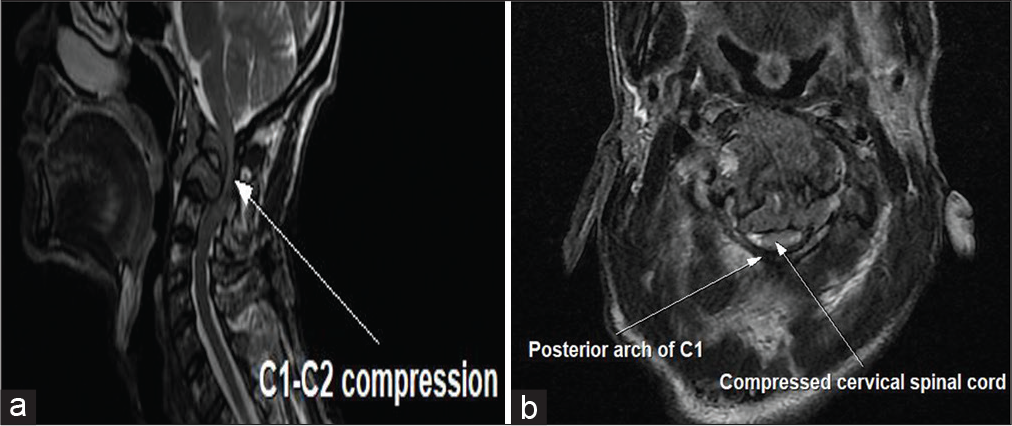
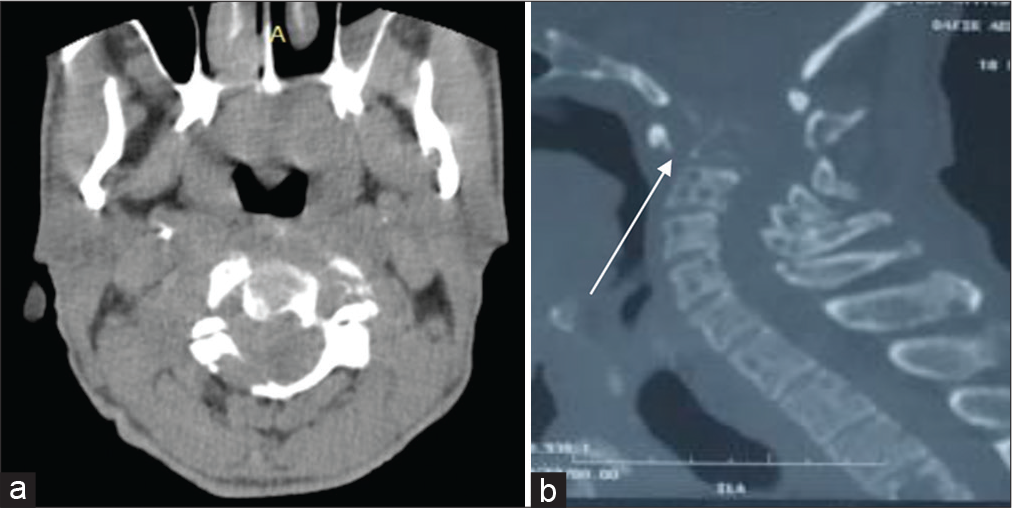
Magnetic resonance imaging (MRI) of the cervical spine showed a hypointense signal on the T1- and T2-weighted image, corresponding to a C1–C2 lesion process with lysis and dislocation exerting a mass effect on the medullary cord [
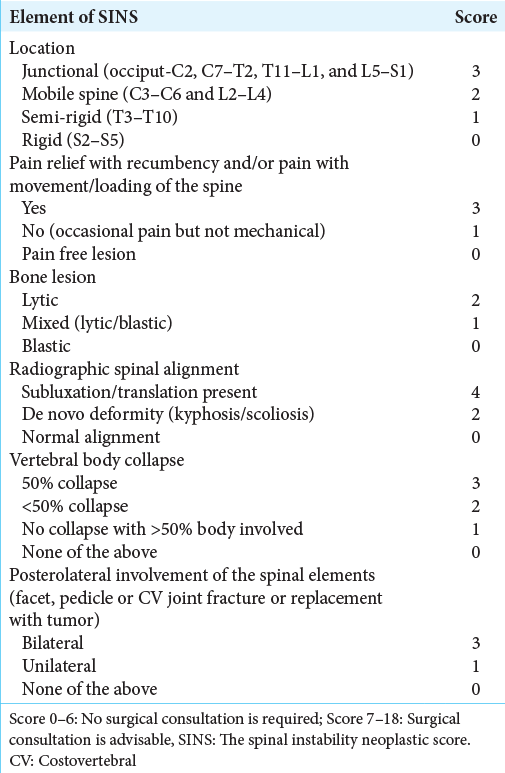
Table 1:
The spinal instability neoplastic score.[
Therapeutic intervention
After a multidisciplinary consultation meeting between neurosurgeons, anesthesiologists, and clinical hematologists, the patient was managed with a rigid adjustable cervical collar for a planned 6-month period and chemotherapy. With a 30% of KPS, this patient is less likely to support surgery.
From the February 15, to the July 17, 2022, five courses of VTD chemotherapy induction were performed. The dosage and duration were Velcade 1.8 mg per os discontinuous, Myrin 100 mg per os continuous, and dexamethasone 40 mg per os discontinuous and then repeated every 3 weeks. This medication was supplemented with antimicrobial prophylaxis such as cotrimoxazole, levofloxacin and valacyclovir, Low-molecular-weight heparin, and folic acid.
Follow-up and outcome
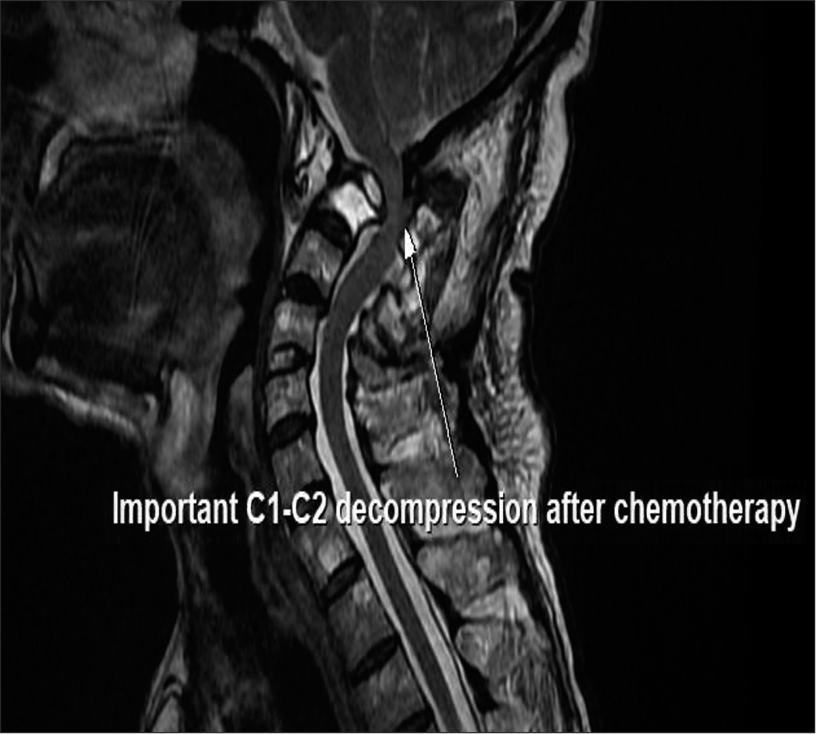
The patient was followed with regular clinical and biological assessments. After five courses of VTD chemotherapy, the Very Good Partial Response rate obtained was 98%. The size of the osteolytic process on C1 and C2 was decreased by 64% on a control MRI of the cervical spine [
The indication of an autograft was decided in the presence of an excellent response to chemotherapy induction courses. The patient underwent the autograft on August 2, 2022. He was discharged with complete resolution of neurologic deficit ASIA E. The rigid adjustable collar has been replaced by the foam cervical collar. The maintenance treatment with Velcade was continued every 2 weeks.
The patient was seen in outpatient consultation 3 months later. Physical examination found a patient in apparent good health with no neurological deficit and was pain-free [
DISCUSSION
The present case described a complete recovery of SCC tetraplegic patient secondary to cervical MM without surgical laminectomy decompression.
Cervical SCC is associated with significant morbidity and mortality. It occurs at a rate of around 22.6% of cervical spine conditions. SCC appears more frequently and early in patients with MM.[
Furthermore, patients with a KPS of <50% usually have decreased life expectancy and are not candidates for surgical treatment.[
When the spinal is unstable, surgery is the best option to restore stability. Management with osteosynthesis is not always practical due to bone deterioration in MM.[
The lack of signs of myelopathy and the decrease of the inflammatory phenomenon responsible for SCC could explain our patient’s neurological improvement. Immobilization with a neck brace helped relieve pain while also reducing the risk of further displacement.
Given our case and that reported by Gokaraju et al.,[
CONCLUSION
The management of MM with SCC is multidisciplinary. This study shows that neck brace immobilization may have a role in the treatment of myeloma patients with mechanically unstable spines, acute SCC, and neurologic disorders. Our nonoperative management in combination with chemotherapy has proven to be safe and successful, avoiding surgery and its complications.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Chen B, Cai L, Zhou F. Management of acute spinal cord compression in multiple myeloma. Crit Rev Oncol Hematol. 2021. 160: 103205
2. Gokaraju K, Butler JS, Benton A, Suarez-Huerta ML, Selvadurai S, Molloy S. Multiple myeloma presenting with acute bony spinal cord compression and mechanical instability successfully managed nonoperatively. Spine J. 2016. 16: e567-70
3. Kwok S, Pang J, Salvo N, Chow E, editors. Prognostic assessment of the cancer patient. Supportive Oncology. Philadelphia: WB Saunders; 2011. p. 472-84
4. Milavec H, Ravikumar N, Syn NL, Soekojo CY, Chng WJ, Kumar N. Surgical management of multiple myeloma with symptomatic involvement of the spine. Int J Spine Surg. 2020. 14: 785-94
5. Molloy S, Lai M, Pratt G, Ramasamy K, Wilson D, Quraishi N. Optimizing the management of patients with spinal myeloma disease. Br J Haematol. 2015. 171: 332-43
6. Patchell RA, Tibbs PA, Regine WF, Payne R, Saris S, Kryscio RJ. Direct decompressive surgical resection in the treatment of spinal cord compression caused by metastatic cancer: A randomised control trial. Lancet. 2005. 366: 643-8
7. Richardson PG, Briemberg H, Jagannath S, Wen PY, Barlogie B, Berenson J. Frequency, characteristics, and reversibility of peripheral neuropathy during treatment of advanced multiple myeloma with bortezomib. J Clin Oncol. 2006. 24: 3113-20
8. Sharma AM, Sackett M, Bueddefeld D, Lambert P, Wadhwa V, Kotb R. Spinal involvement in myeloma: Incidence, survival, and impact of radiotherapy. Int J Radiat Oncol. 2017. 99: E434
9. Versteeg AL, van der Velden JM, Verkooijen HM, van Vulpen M, Oner FC, Fisher CG. The effect of introducing the spinal instability neoplastic score in routine clinical practice for patients with spinal metastases. Oncologist. 2016. 21: 95-101