- Clinic of Infectious and Tropical Diseases, Spedali Civili Hospital, Brescia, Italy
- Department of Neurosurgery, ASST – Ovest Milanese, Legnano, Italy
- Department of Neurosurgery, Spedali Civili Hospital, Brescia, Italy
- Department of Anesthesia, Critical Care and Emergency, Spedali Civili Hospital, Brescia, Italy
Correspondence Address:
Liana Signorini
Clinic of Infectious and Tropical Diseases, Spedali Civili Hospital, Brescia, Italy
DOI:10.4103/2152-7806.195228
Copyright: © 2016 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Laura Soavi, Manuela Rosina, Roberto Stefini, Alessia Fratianni, Barbara Cadeo, Silvia Magri, Nicola Latronico, Marco Fontanella, Liana Signorini. Post-neurosurgical meningitis: Management of cerebrospinal fluid drainage catheters influences the evolution of infection. 05-Dec-2016;7:
How to cite this URL: Laura Soavi, Manuela Rosina, Roberto Stefini, Alessia Fratianni, Barbara Cadeo, Silvia Magri, Nicola Latronico, Marco Fontanella, Liana Signorini. Post-neurosurgical meningitis: Management of cerebrospinal fluid drainage catheters influences the evolution of infection. 05-Dec-2016;7:. Available from: http://surgicalneurologyint.com/surgicalint_articles/post%e2%80%91neurosurgical-meningitis-management-of-cerebrospinal-fluid-drainage-catheters-influences-the-evolution-of-infection/
Abstract
Background:In order to better define the pathogenic role of cerebrospinal fluid (CSF) drainage catheters in postoperative patients, we comparatively analyze the clinical course of device and non-device-related meningitis.
Methods:This is an observational, partially prospective, study on consecutive adult patients who developed meningitis after undergoing neurosurgical procedures at the Neurosurgery and Neurointensive care Departments, Spedali Civili, Brescia, Italy, between January 1999 and August 2007.
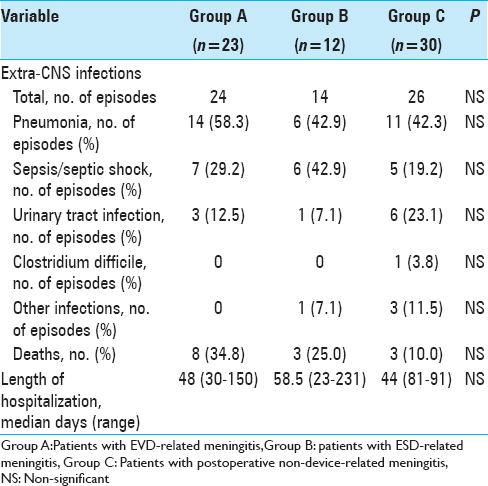
Results:All 77 consecutive post-neurosurgical meningitis events in 65 patients were included in the analysis. Most were classified as external ventricular drainage (EVD)-related meningitis (23 cases, group A), external spinal drainage (ESD)-related meningitis (12 cases, group B), and non-device-related post-neurosurgical meningitis (30 cases, group C). Proven meningitis was identified in 78.3%, 91.7% and 56.7% of the events, respectively. ESD-related meningitis had a shorter onset time vs EVD and non-device-associated meningitis (3 days versus 6 and 7 days, respectively). Median antibiotic treatment duration was 20, 17, and 22.5 days in groups A, B, and C, respectively. Overall, 8 patients (34.8%) in group A, 3 (25.0%) in group B, and 3 (10.0%) in group C died. Median time to become afebrile was shorter in group C than in group A (10 days versus 12 days, P = 0.04). Removal of the device later than 48 hours after meningitis onset, as well as implantation of a second device were associated with a slower time of meningitis resolution.
Conclusions:Early device removal and avoiding implantation of a second device were associated with short illness duration. Larger studies are warranted to confirm the conclusions of this study.
Keywords: Cerebrospinal fluid drainage catheters, meningitis, neurosurgery
INTRODUCTION
Postoperative meningitis is a rare but serious complication of neurosurgery. In clean neurosurgery, the rate of postoperative bacterial meningitis is low (1–2%).[
There is a large body of evidence regarding postoperative meningitis in terms of risk factors, pathogenesis, and microbiological aspects.[
We performed an observational study of all consecutive cases of postoperative meningitis observed in adults at a tertiary hospital in Northern Italy to compare outcome and clinical evolution, including laboratory and microbiological parameters, of device (EVD and ESD-related) and non-device-related meningitis.
MATERIALS AND METHODS
Hospital setting
The study was conducted at the Department of Neurosurgery and Neurointensive care of Spedali Civili, Brescia, Italy. An intensive infectious diseases consultation program, with ≥3 consultations per week, has been ongoing since 1999.
Study population and data collection
We included all consecutive cases of postoperative meningitis observed between January 1999 and August 2007 in patients over 18 years of age. Data were collected retrospectively until June 2004 and prospectively thereafter. During the retrospective phase, episodes of meningitis were identified using the electronic register, identifying cases of meningitis from the discharge diagnosis and/or from the infectious diseases consultation records, and relevant medical charts were reviewed. The protocol for perioperative antibiotic prophylaxis consisted of cephazoline 2 g intravenously half an hour before surgery followed by 1 g after 3 hours, if the duration of the intervention exceeded 3 hours.
During the prospective phase, each episode was evaluated by infectious diseases consultants according to the predefined criteria (see below), and data was actively collected on ad-hoc charts. To evaluate the influence of neurosurgical devices on meningitis evolution and outcome, statistical analysis was performed to compare patients with EVD, with ESD, and without any device.
Case definitions
Proven meningitis was defined as a positive CSF culture and laboratory CSF findings of a neutrophilic CSF pleocytosis (>5 cells/µL) and a CSF/blood glucose ratio of <0.5 along with meningitis signs and/or symptoms [fever, headache, neck stiffness, cranial nerve signs, or Glasgow coma scale (GCS) worsening].
Possible meningitis was defined by laboratory CSF findings of a neutrophilic CSF pleocytosis (>5 cells/µL) and a CSF/blood glucose ratio of <0.5 along with meningitis signs and/or symptoms with a negative CSF culture.
Patients with postoperative, non-device-related meningitis were included if neurosurgery had been performed 3 months or less prior to meningitis onset. Patients with postoperative device-related meningitis were included if the neurosurgical device was in place at meningitis onset.
Fever clearance (T ≤ 37°C) was utilized to evaluate clinical response to therapy. Blood and CSF samples were periodically collected to evaluate improvement time (time from onset to the second consecutive improved measurement) and normalization of the following parameters: Blood/CSF leucocyte count and CSF glucose level.
Statistical analysis
Student's t-test was used to compare means and a Chi-square test was used to compare proportions. Continuous variables were compared using the Wilcoxon rank-sum test. A P value of 0.05 was considered to be statistically significant. A multivariate logistic regression model was fitted to the data to identify potential factors related to the outcome. All calculations were performed using the Stata version 13 software (StataCorp. 2013. Stata Statistical Software: Release 13. College Station, TX: StataCorp LP)..
RESULTS
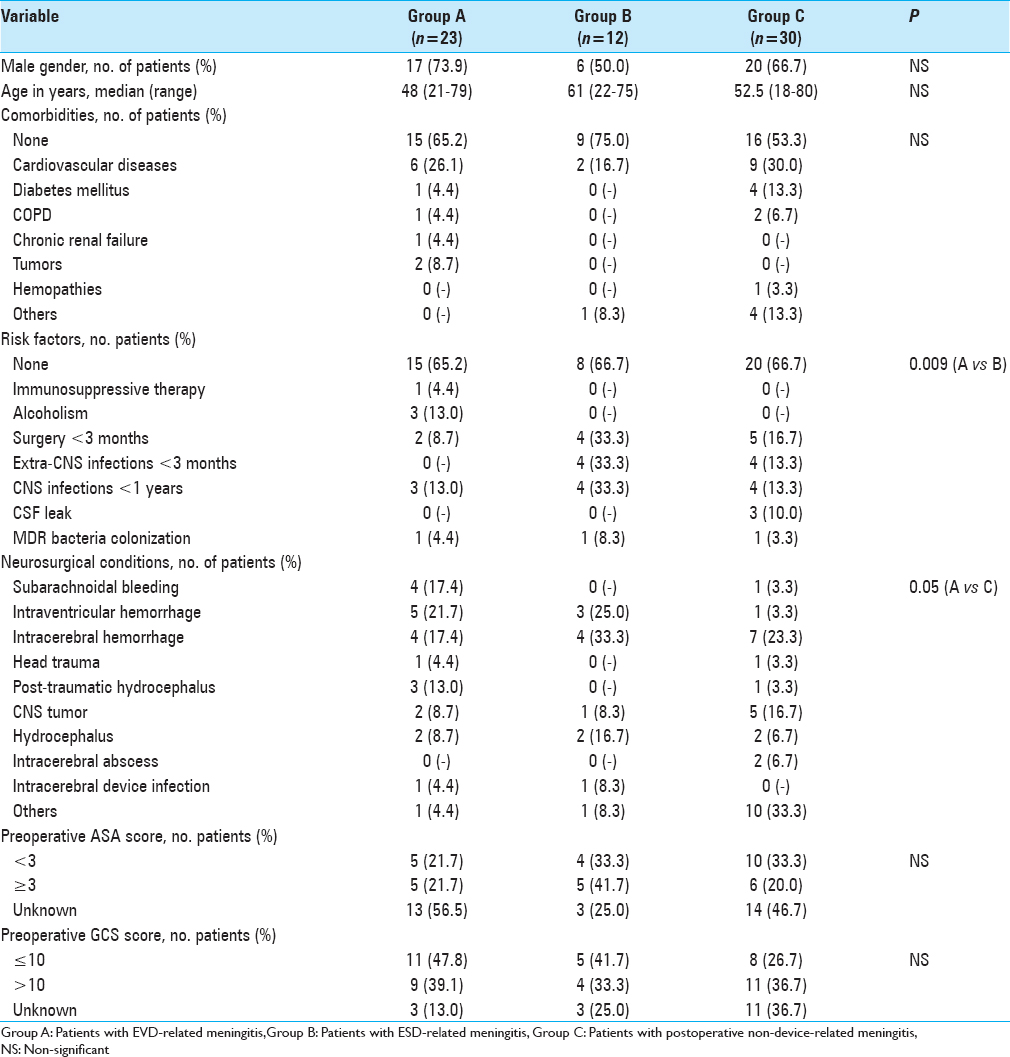
During the study period, 77 events of postoperative meningitis were identified among 65 patients. Description of the study population is shown in
Emergency surgery was performed in 14 patients (60.9%) in group A, 3 (25.0%) in group B, and 8 (26.7%) in group C (P = 0.03 for A vs C). Median duration of surgery in groups A, B, and C was, respectively, 85 (range: 15–360), 180 (range: 20–300), and 180 minutes (range: 60–990). Among patients who were not receiving antibiotic therapy at the time of neurosurgery, antibiotic prophylaxis was appropriately prescribed in, respectively, 6/16 (37.5%), 3/9 (33.3%), and 10/27 patients (37.0%). Eleven patients (47.8%) in group A, 5 (41.7%) in group B, and 12 (40%) in group C experienced postoperative complications (mainly CSF leakage and relapse of intraventricular hemorrhage). No statistically significant differences were found in length of surgery, appropriateness of prophylaxis, and frequency of postoperative complications among the three groups.
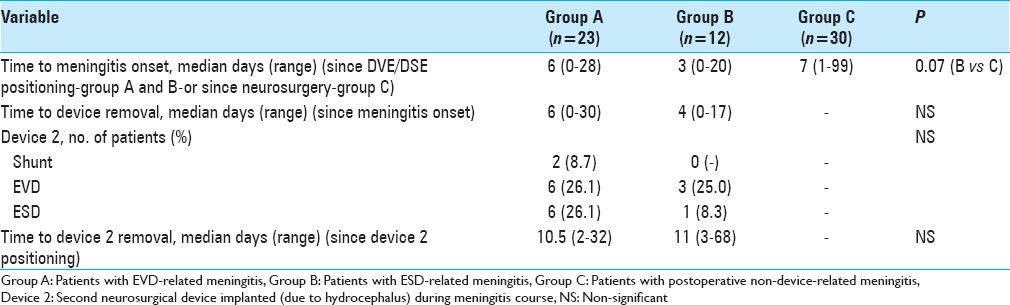
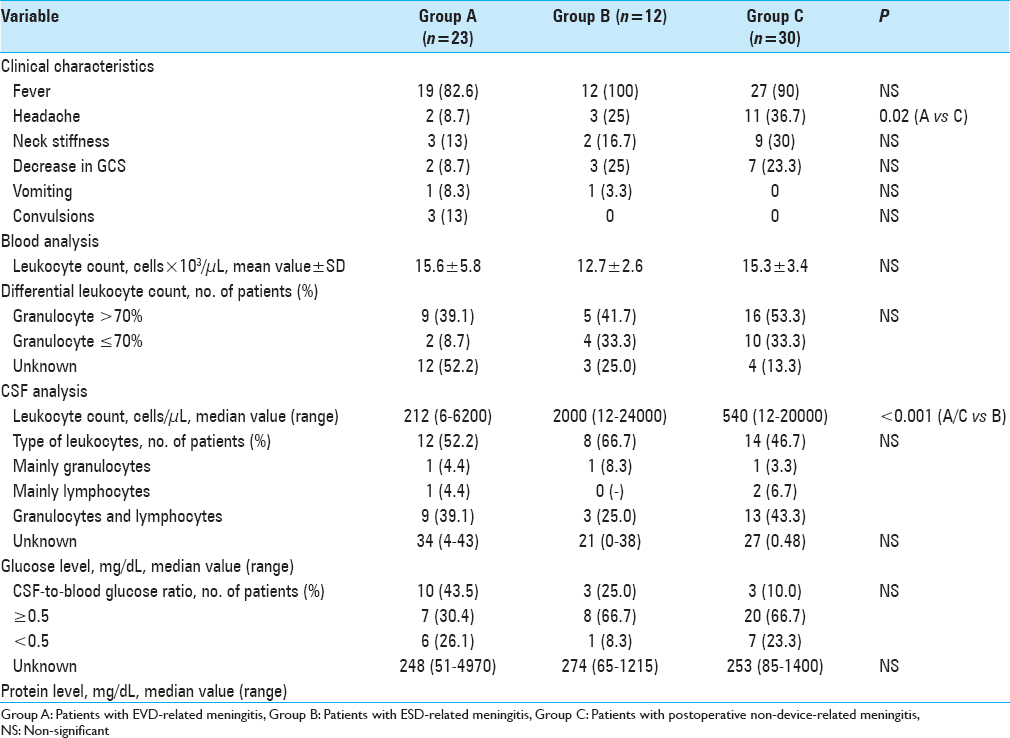
Variables related to meningitis clinical presentation and blood/CSF chemistry at meningitis onset are summarized in
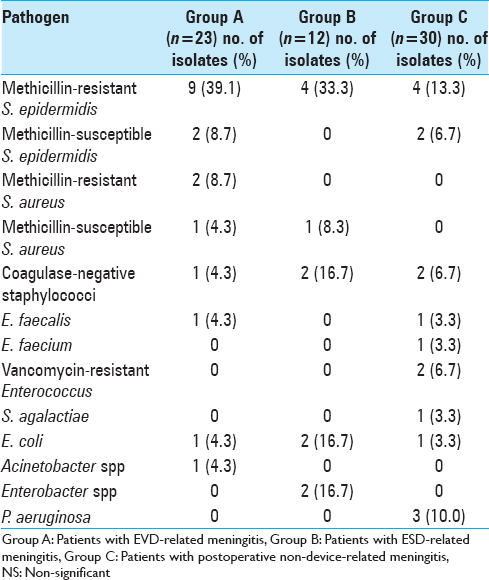
Meningitis was proven in 18 (78.3%), 11 (91.7%), and 17 (56.7%) in groups A, B, and C, respectively. Among patients for whom CSF culture yielded negative results (5 patients in group A, 1 in group B, and 13 in group C), 2 patients in group A and 4 in group C were on antibiotic therapy when the CSF culture was performed. Microorganisms responsible for meningitis are presented in
All patients received intravenous antibiotic therapy. In addition, 3 patients (13%) in group A, 2 (16.7%) in group B, and 1 (3.3%) in group C received intrathecal antibiotics. Median intravenous antibiotic treatment duration was 20 days (range: 5–57 days) in group A, 17 days (range: 4–60 days) in group B, and 22.5 days (range: 3–41 days) in group C. There was no significant difference in the length of therapy between the three groups.
Clinical, biochemical, and microbiological course of meningitis
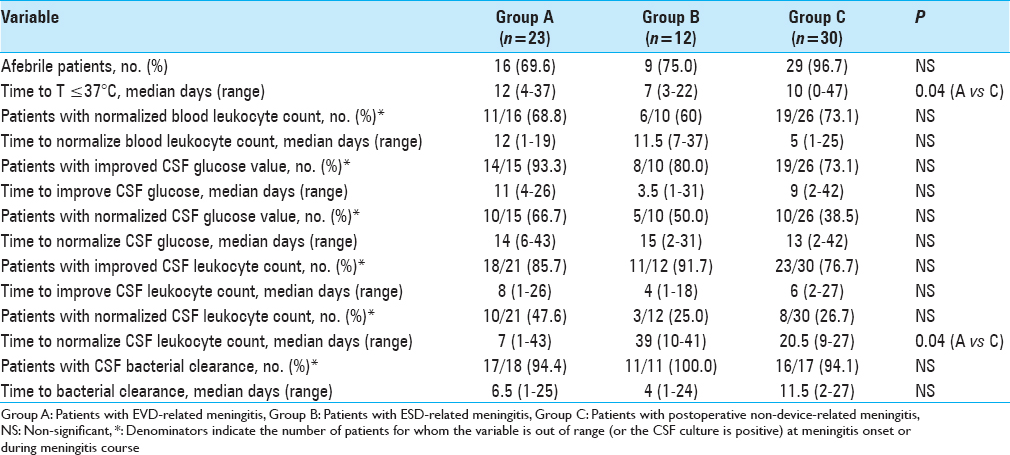
Description of the clinical, biochemical, and microbiological course of meningitis is shown in
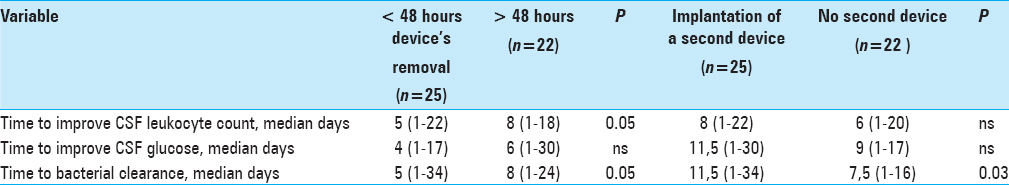
Removing devices (both EVD and ESD) in the first 48 hours after meningitis onset was associated with shorter time to CSF leukocyte reduction (median 5 days versus 8 days, P = 0.05), and shorter time to CSF bacterial clearance (median of 5 days versus 8 days, P = 0.05) [
In patients with EVD and ESD-related meningitis, positioning of a second device was associated with longer median time to bacterial clearance (11.5 days versus 7.5 days, P = 0.03).
DISCUSSION
Our single-center study of 77 consecutive events of postoperative meningitis is, to our knowledge, the first study aimed to compare the clinical, biochemical, and microbiological course, as well as the outcome of device and non-device-related meningitis.
Our results show an overall post-neurosurgical meningitis rate of 4.9%, which is well within the range observe in other studies,[
Of note, the presence of a ventricular drainage influenced the time to meningitis resolution. Time to bacterial clearance and improved CSF leukocyte count were significantly shorter in patients with early device removal; moreover, implantation of a second device was associated with longer time to bacterial clearance in CSF. This observation is consistent with the knowledge that any device and related biofilm facilitates bacterial survival and hampers the effect of antibiotic treatment. These findings support attempts to remove devices as early as possible and to avoid positioning of a second CSF drainage catheter whenever possible.
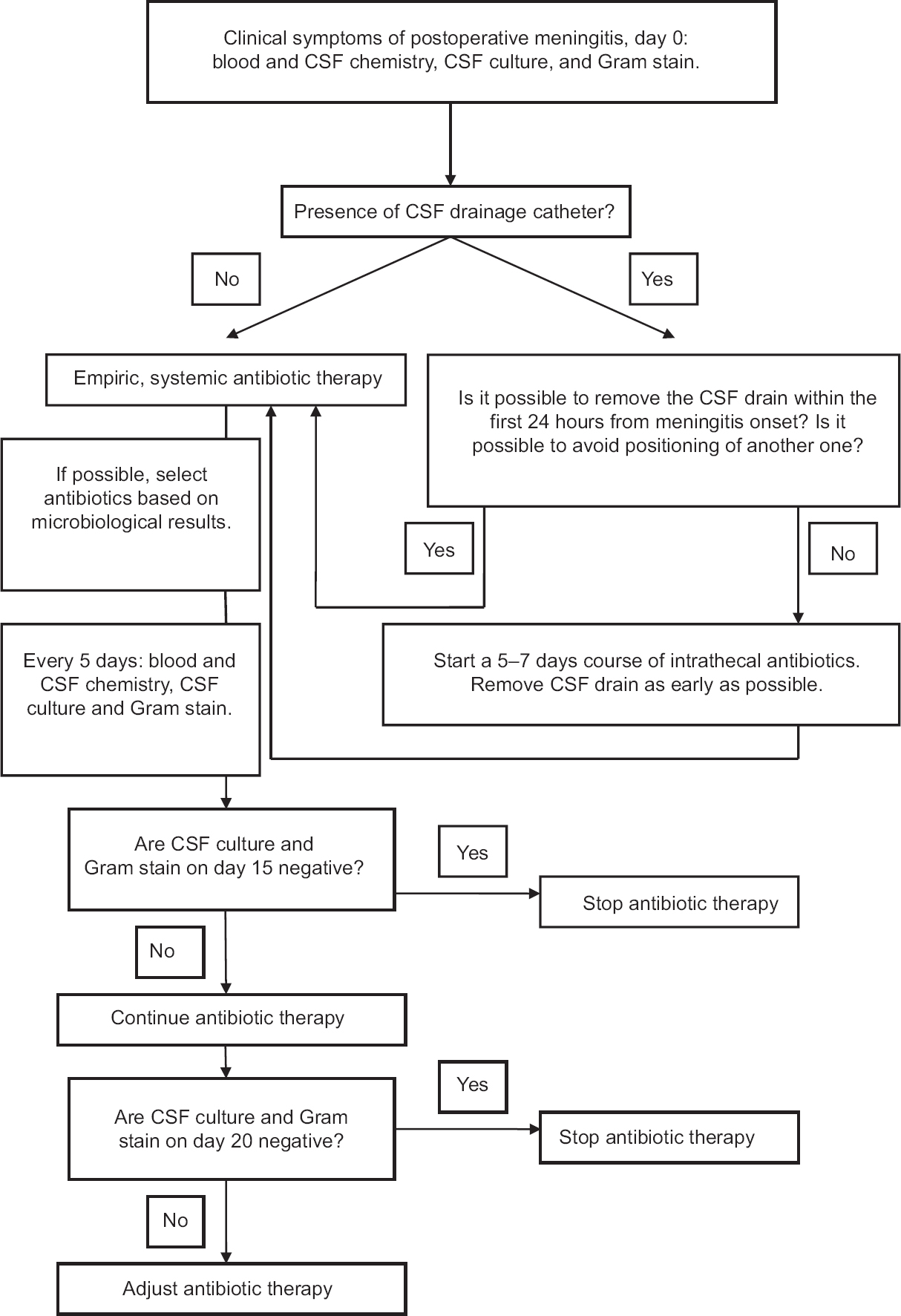
Based on the study results, we updated the algorithm for the management of patients with proven or possible postoperative meningitis [
Our study has several limitations. Due to its partially retrospective design, diagnostic and therapeutic procedures were not systematically standardized. Furthermore, patients’ subgroups were small and with limited ability to identify significant associations of one or a group of variables. However, we analyzed a large number of ESD-related meningitis, which have rarely been investigated to date.[
CONCLUSION
In summary, early device removal was associated with shorter illness duration, whereas implantation of a second device during the course of meningitis was associated with a longer resolution time. These observations will need to be validated in a prospective study in order to better define the timing of device removal, its eventual repositioning, as well as the best antibiotic regimen.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Arabi Y, Memish ZA, Balkhy HH, Francis C, Ferayan A, Al Shimemeri A. Ventriculostomy-associated infections: Incidence and risk factors. AJIC. 2005. 33: 137-43
2. Bogdahn U, Lau W, Hassel W, Gunreben G, Mertens HG, Brawanski A. Continuous-pressure controlled, external ventricular drainage for treatment of acute hydrocephalus – Evaluation of risk factors. Neurosurgery. 1992. 31: 898-904
3. Citerio G, Signorini L, Bronco A, Vargiolu A, Rota M, Latronico N. Infezioni LIquorali Catetere Correlate Study Investigators. External Ventricular and Lumbar Drain Device Infections in ICU Patients: A Prospective Multicenter Italian Study. Crit Care Med. 2015. 43: 1630-7
4. Conen A, Walti LN, Merlo A, Fluckiger U, Battegay M, Trampuz A. Characteristics and treatment outcome of cerebrospinal fluid shunt-associated infections in adults: A retrospective analysis over an 11-year period. Clin Infect Dis. 2008. 47: 73-82
5. Coplin WM, Avellino AM, Kim DK, Winn HR, Grady MS. Bacterial meningitis associated with lumbar drains: A retrospective cohort study. J Neurol Neurosurg Psychiatry. 1996. 67: 468-73
6. Governale LS, Fein N, Logsdon J, Black PM. Techniques and complications of external lumbar drainage for normal pressure hydrocephalus. Neurosurgery. 2008. 63: 379-84
7. Holloway KL, Barnes T, Choi S, Bullock R, Marshall LF, Eisenberg HM. Ventriculostomy infections: The effect of monitoring duration and catheter exchange in 584 patients. J Neurosurg. 1996. 85: 419-24
8. Korinek AM, Reina M, Boch AL, Rivera AO, De Bels D, Puybasset L. Prevention of external ventricular drain-related ventriculitis. Acta Neurochir. 2005. 147: 39-46
9. Lozier AP, Sciacca RR, Romagnoli MF, Sander Connolly E. Ventriculostomy-related infections: A critical review of the literature. Neurosurgery. 2002. 51: 170-82
10. Lyke KE, Obasanjo OO, Williams MA, O’Brien M, Chotani R, Perl TM. Ventriculitis complicating use of intraventricular catheters in adult neurosurgical patients. Clin Infect Dis. 2001. 33: 2028-33
11. Mayhall CG, Archer NH, Lamb VA, Spadora AC, Baggett JW, Ward JD. Ventriculostomy-related infections. A prospective epidemiologic study. N Engl J Med. 1984. 310: 553-9
12. Park P, Garton HJ, Kocan MJ, Thompson BG. Risk of infection with prolonged ventricular catheterization. Neurosurgery. 2004. 55: 594-601
13. Pfisterer W, Muehlbauer M, Czech T, Reinprecht A. Early diagnosis of external ventricular drainage infection: Results of a prospective study. J Neurol Neurosurg Psychiatry. 2003. 74: 929-32
14. van de Beek D, Drake JM, Tunkel AR. Nosocomial bacterial meningitis. N Engl J Med. 2010. 362: 146-54