- Neurosurgical Department, King's College Hospital Foundation Trust, London, United Kingdom
- Institute of Psychiatry, Psychology and Neuroscience, King's College London, London, United Kingdom
Correspondence Address:
Christian Brogna
Neurosurgical Department, King's College Hospital Foundation Trust, London, United Kingdom
DOI:10.4103/sni.sni_29_18
Copyright: © 2018 Surgical Neurology International This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.How to cite this article: Christian Brogna, José Pedro Lavrador, Sabina Patel, Francesco Vergani, Sanjeev Bassi, Gordan Grahovac, Ranjeev Bhangoo, Keyoumars Ashkan. Posterior longitudinal ligament and its implications in intradural cervical disc herniation: Case report and review of the literature. Surg Neurol Int 18-Jun-2018;9:119
How to cite this URL: Christian Brogna, José Pedro Lavrador, Sabina Patel, Francesco Vergani, Sanjeev Bassi, Gordan Grahovac, Ranjeev Bhangoo, Keyoumars Ashkan. Posterior longitudinal ligament and its implications in intradural cervical disc herniation: Case report and review of the literature. Surg Neurol Int 18-Jun-2018;9:119. Available from: http://surgicalneurologyint.com/surgicalint-articles/posterior-longitudinal-ligament-and-its-implications-in-intradural-cervical-disc-herniation-case-report-and-review-of-the-literature/
Abstract
Background:Intradural disc herniations (IDH) are rare, particularly in the cervical spine, where they account for less than 5% of all discs. Adhesions between the ossified/calcified posterior longitudinal ligament (OPLL), dura, and ossified/calcified disc herniations increase the complexity of resecting these cervical lesions.
Case Description:A 42-year-old male presented with a rapidly progressive cervical myelopathy over a 2-month period. This was attributed to an ossified/calcified intradural cervical disc herniation in conjunction with OPLL. The anterior cervical discectomy and fusion (ACDF) resulted in a dural defect but there was no cerebrospinal fluid (CSF) fistula as the arachnoid membrane remained intact. Had there been a CSF leak, it would have warranted both wound-peritoneal (WP) and lumbo-peritoneal shunts (LP). The surgeons should have anticipated that a CSF leak would likely occur prior to performing the ACDF, and should have prophylactically prepared and draped the abdomen for a potential WP, followed by a LP shunt. Three months postoperatively, the patient's proprioceptive deficit improved, and he almost completely recovered motor function.
Conclusion:Performing an ACDF for resection of an intradural calcified/ossified disc with OPLL often results in both a dural defect and CSF fistula. As the arachnoid membrane rarely remains intact, the spine surgeon should be prepared to immediately perform both a WP shunt, and subsequently, an LP. In this case, following an ACDF, resection of an intradural ossified disc with OPLL resulted in an isolated dural defect without a CSF fistula and did not require no dural repair or shunting procedures.
Keywords: CSF leak, intradural cervical disc herniation, posterior longitudinal ligament
INTRODUCTION
Intradural herniations (IDH) are rare and most commonly present in the lumbar (92%), followed by the thoracic (5%) and cervical spine (3%).[
Here, a patient with an ossified/calcified cervical IDH with OPLL underwent an ACDF with durotomy but without an accompanying cerebrospinal fluid (CSF) fistula that did not warrant any shunting procedures.
CASE REPORT
Clinical findings
A 42-year-old male presented with a 2-month history of a cervical myelopathy that had rapidly progressed over the past 2 weeks. He exhibited a left hemiparesis (2/5 motor) but normal function on the right side, which was accompanied by hypoesthesia in both lower extremities. Interestingly, reflexes remained intact bilaterally, and he retained normal sphincter function.
Radiographic evaluation
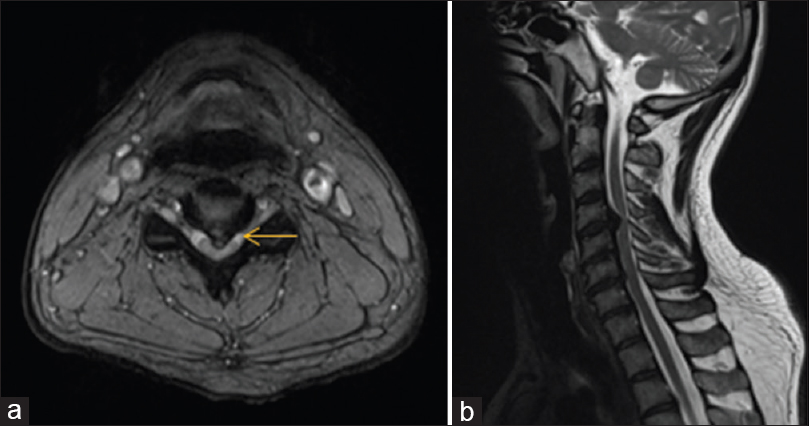
The cervical spine magnetic resonance imaging (MRI) showed a large ossified/calcified central disc herniation at the C4/5 level with OPLL contributing to marked ventral cord compression [
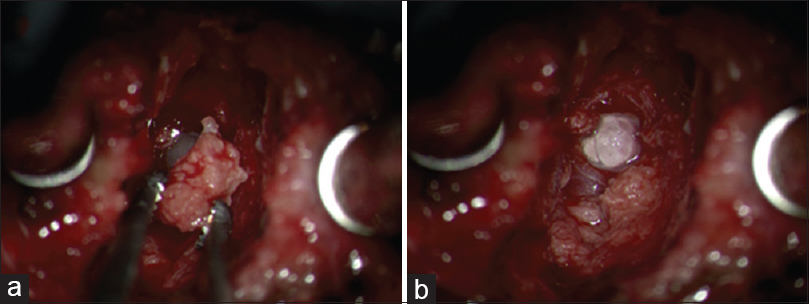
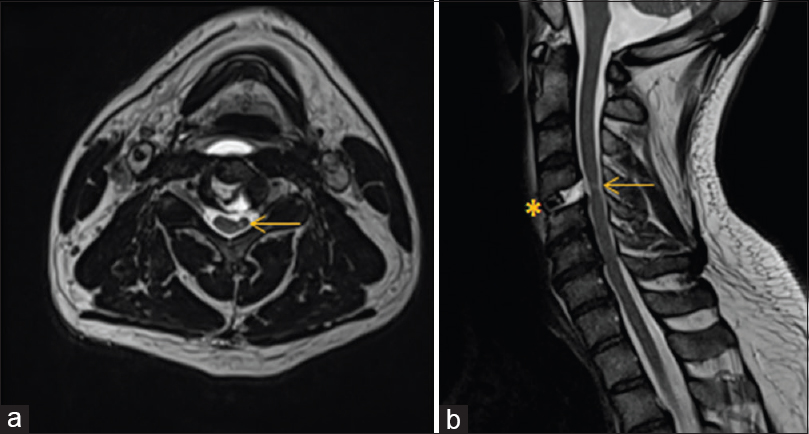
When an ACDF was performed, they encountered a large calcified disc fragment with OPLL that was removed en bloc. Although there was a tear in the dura, the arachnoid remained intact; there was no accompanying cerebrospinal fluid (CSF) fistula [
DISCUSSION
The pathogenesis of IDH include congenital narrowing of the spinal canal, chronic compression of a highly mobile segment of the spinal canal, and adhesions between the calcified/ossified ligaments, OPLL, and dura.[
IDH with OPLL can be intra-arachnoidal (e.g. due to adhesions/calcification between the PLL and the dura) or extra-arachnoidal. Therefore, high CSF leak rates are reported for anterior OPLL surgery (e.g. 4.3–32%).[
CONCLUSION
Here, a patient with a calcified/ossified cervical IDH/OPLL sustained a durotomy without a CSF fistula during an ACDF. No shunting procedures (WP and LP shunts) were required as the arachnoid remained intact. In the future, the spinal surgeon should obtain a preoperative CT to supplement MRI as this would best identify the classical single or double-layer signs indicating OPLL dural penetrance. This would have warned the surgeon of a potential anterior dural/arachnoidal fistula, and would have enabled them to prophylactically prepare and drape for and anticipate a CSF fistula requiring both an immediate WP, followed by an LP shunt.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Baudracco I, Grahovac G, Russo VM. Spontaneous cervical intradural disc herniation presenting with Brown-Séquard and Horner's syndrome: Lesson learned from a very unique case. Eur Spine J. 2017. 26: 218-21
2. Epstein NE. Wound-peritoneal shunts: Part of the complex management of anterior dural lacerations in patients with ossification of the posterior longitudinal ligament. Surg Neurol. 2009. 72: 630-4
3. Harrison J, Goldstein CL, Shamji MF. Acute spontaneous cervical disc herniation causing rapidly progressive myelopathy in a patient with comorbid ossified posterior longitudinal ligament: Case report and literature review. Surg Neurol Int. 2014. 5: 68-72
4. Marega T. Ernia del disco cervicale espulsa nel sacco durale. Arch Putti Chir Organi Mov. 1959. 12: 425-30
5. Pan J, Li Lijun, Qian L, Teng H, Shen B, Tan J. Intradural cervical disc herniation. Spine. 2011. 36: 1033-7
6. Wang X, Chen D, Yuan W, Zhang Y, Xiao J, Zhao J. Anterior surgery in selective patients with massive ossification of posterior longitudinal ligament of cervical spine: Technical note. Eur Spine J. 2012. 121: 314-21
7. Wang Z, Sunna T. Intradural lumbar disc herniation associated with degenerative spine disease. Int J Neurorehabil. 2015. 2: 2376-0281
8. Warade AG, Misra BK. Spontaneous cervical intradural disc herniation. J Clin Neurosci. 2014. 21: 872-3
9. Yang HS, Oh YM, Eun JP. Cervical intradural disc herniation causing progressive quadriparesis after spinal manipulation therapy: A case report and literature review. Medicine (Baltimore). 2016. 95: e2797-