- Department of Spinal Surgery, Leeds General Infirmary, Leeds, United Kingdom
Correspondence Address:
Jack Van-Loo, Department of Spinal Surgery, Leeds General Infirmary, Leeds, United Kingdom.
DOI:10.25259/SNI_823_2024
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Jack Van-Loo, Nitin Adsul, Peter Loughenbury, Nigel William Gummerson. Postoperative left-sided chylothorax following posterior approach in late-onset idiopathic scoliosis surgery. 08-Nov-2024;15:408
How to cite this URL: Jack Van-Loo, Nitin Adsul, Peter Loughenbury, Nigel William Gummerson. Postoperative left-sided chylothorax following posterior approach in late-onset idiopathic scoliosis surgery. 08-Nov-2024;15:408. Available from: https://surgicalneurologyint.com/surgicalint-articles/13207/
Abstract
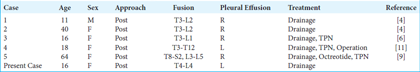
Background: Chylothorax is an extremely rare complication of spinal surgery. We were only able to identify 15 previous cases overall, with only 5 involving a posterior approach.
Case Description: A 16-year-old female presented with a chylothorax following a T4–L4 posterior spinal fusion for scoliosis. Postoperatively, the patient developed respiratory distress due to a left-sided pleural effusion. Laboratory tests (i.e., both gross and laboratory analysis) documented the fluid to be chyle. The patient required the placement of a chest drain and a low triglyceride diet to manage and resolve the chylothorax successfully.
Conclusion: Chylothorax is a rare complication of spinal surgery and should be considered among the differential diagnoses involving postoperative respiratory compromise attributed to pleural effusions.
Keywords: Adolescent idiopathic scoliosis, Chylothorax, Complication, Corrective surgery, Scoliosis
INTRODUCTION
Chylothorax is a rare but potentially life-threatening complication more commonly found in anterior versus posterior thoracic spine surgery.
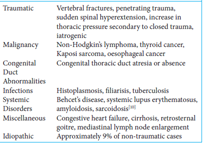
Chylothorax is attributed to the accumulation of chyle from the thoracic duct or its tributaries that drain into the thoracic cavity. Complications of chylothorax may include dyspnea, immune suppression, heart failure, and even death.[
CASE REPORT
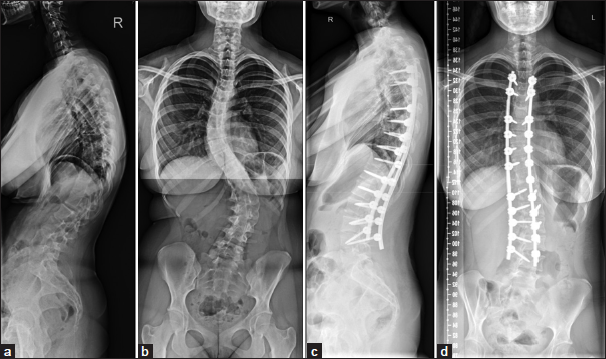
A 16-year-old female with idiopathic scoliosis (Lenke 6) underwent a posterior spinal instrumented fusion (T4–L4) [
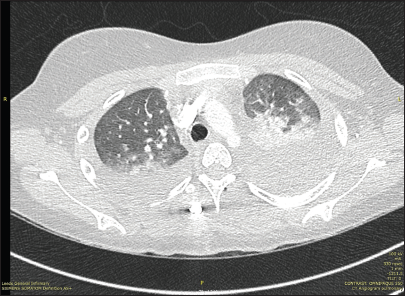
When a chest tube was placed, it revealed a milky fluid and laboratory studies confirmed that it was a chylothorax (triglycerides 5.0 mmoL/L, glucose 6.1 mmoL/L, lactate dehydrogenase 204 IU/L, and protein <20 g/L) [
DISCUSSION
Incidence and diagnostic confirmation of chylothorax
Chylothorax, usually unilateral, accounts for between 2% and 3% of all pleural effusions. Approximately half of cases are due to trauma versus malignancy [
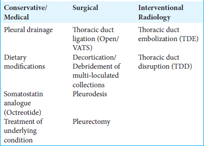
Conservative management
Early dietary intervention (i.e., to reduce the volume of chyle produced in the lymphatic system) is often sufficient to resolve traumatic chylothorax.[
Medical therapy for chylothorax
Medical therapy such as octreotide, a somatostatin analog, has been used both as a continuous infusion and as a bolus to reduce the production of lymph; it reduces the splanchnic circulation and the secretions from the gastrointestinal tract.[
Surgery for chylothorax
Surgery for evacuation of chyle should be considered when drainage exceeds 500 mL/day for 5 days. Surgical options to treat chylothorax include thoracic duct ligation, pleurodesis, and pleurectomy.[
CONCLUSION
While extremely rare, chylothorax constitutes a serious complication of instrumented typically thoracic or lower cervical/thoracic spinal fusion surgery. To confirm the diagnosis, laboratory analysis should be performed, and conservative medical, and/or surgical management instituted.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Browse NL, Allen DR, Wilson NM. Management of chylothorax. Br J Surg. 1997. 84: 1711-6
2. Lai FC, Chen L, Tu YR, Lin M, Li X. Prevention of chylothorax complicating extensive esophageal resection by mass ligation of thoracic duct: A random control study. Ann Thorac Surg. 2011. 91: 1770-74
3. Maldonado F, Cartin-Ceba R, Hawkins FJ, Ryu JH. Medical and surgical management of chylothorax and associated outcomes. Am J Med Sci. 2010. 339: 314-8
4. Nakai S, Zielke K. Chylothorax–a rare complication after anterior and posterior spinal correction. Report on six cases. Spine. 1986. 11: 830-3
5. Pakula AM, Phillips W, Skinner RA. A case of a traumatic chyle leak following an acute thoracic spine injury: Successful resolution with strict dietary manipulation. World J Emerg Surg. 2011. 6: 10
6. Rames RD, Schoenecker PL, Bridwell KH. Chylothorax after posterior spinal instrumentation and fusion. Clin Orthop Relat Res. 1990. 261: 229-32
7. Ryu JH, Tomassetti S, Maldonado F. Update on uncommon pleural effusions. Respirology. 2011. 16: 238-43
8. Schild HH, Strassburg CP, Welz A, Kalff J. Treatment options in patients with chylothorax. Dtsch Arztebl Int. 2013. 110: 819-26
9. Toriyama K, Kokuho N, Yajima C, Kawagoe J, Togashi Y, Tsuji T. Chylothorax after spinal fusion surgery: A case report and literature review. Respir Med Case Rep. 2019. 26: 260-64
10. Ur Rehman K, Sivakumar P. Non-traumatic chylothorax: Diagnostic and therapeutic strategies. Breathe (Sheff). 2022. 18: 210163
11. Weening AA, Schurink B, Ruurda JP, van Hillegersberg R, Bleys R, Kruyt MC. Chyluria and chylothorax after posterior selective fusion for adolescent idiopathic scoliosis. Eur Spine J. 2018. 27: 2088-92