- Department of Neurosurgery, The Aga Khan University, Karachi, Sindh, Pakistan.
Correspondence Address:
Muhammad Ehsan Bari, Department of Neurosurgery, The Aga Khan University, Karachi, Sindh, Pakistan.
DOI:10.25259/SNI_473_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Mohammad Hamza Bajwa, Nasr Hussain, Muhammad Ehsan Bari. Prepontine intracerebral cyst with spontaneous resolution. 09-Aug-2021;12:402
How to cite this URL: Mohammad Hamza Bajwa, Nasr Hussain, Muhammad Ehsan Bari. Prepontine intracerebral cyst with spontaneous resolution. 09-Aug-2021;12:402. Available from: https://surgicalneurologyint.com/surgicalint-articles/11026/
Abstract
Background: Intracranial cysts in the prepontine region are rare and can lead to various complications if not managed appropriately. Symptomatic prepontine cysts may require surgical intervention. However, spontaneous resolution of such cysts is rarely reported in literature.
Case Description: We describe the case of a middle-aged lady who presented with headaches and imbalance, with no focal neurological deficits on examination. Magnetic resonance imaging (MRI) of the brain showed a prepontine cyst compressing the brainstem with craniocaudal extension through the foramen magnum. The patient was given symptomatic treatment and followed closely with repeat MRI scans. These scans showed regression and eventual disappearance of the lesion, with complete resolution of symptoms.
Conclusion: In light of the few reported cases of spontaneous resolution of prepontine cysts, we highlight the possibility of these lesions to self-resolve.
Keywords: Adult brain cyst, Prepontine cyst, Spontaneous resolution
INTRODUCTION
Intracerebral cysts, by and large, create various differentials: arachnoid, epidermoid, neuroenteric, and so on.[
Most intracranial cysts are asymptomatic, with few presenting with nonspecific symptoms such as headaches and visual symptoms, and rarely, neurological deficits. As clinicians opt for brain imaging, often the question arises when to intervene. Prepontine cysts may result in obstructive hydrocephalus, mass effect, spontaneous rupture, leakage of cyst contents leading to aseptic meningitis, and rarely, malignant transformation.[
The prepontine space exists as a potential space for many pathologies. While rare, the finding of a cystic lesion means deciding between surgical intervention and conservative treatment. Due to the rarity of reported prepontine cysts, there is no consensus regarding management. We present a case where such considerations played a role in clinical decision-making.
CASE REPORT
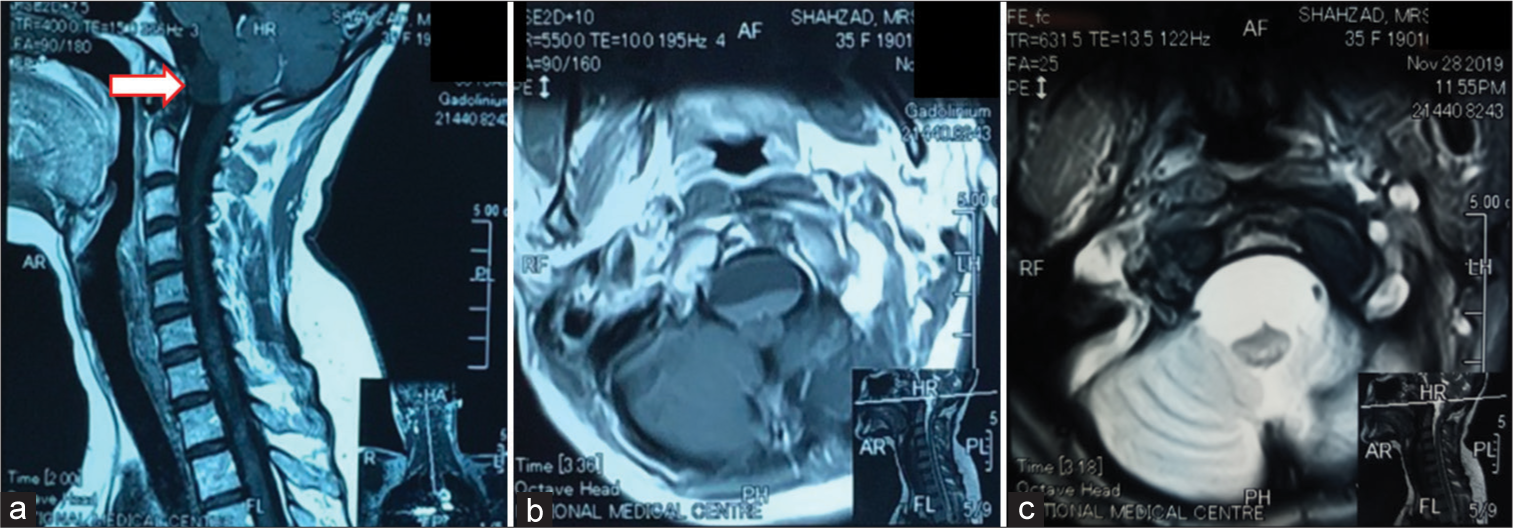
A 40-year-old, right-handed, lady, with no prior comorbidities, presented to us in the clinic with complaints of headache and imbalance for the past 20 days. She described her headache as being most severe in the morning, with no associated nausea, vomiting, or visual complaints. Her vertigo was also most prominent on waking up. The patient reported pain in her neck which radiated down her whole spine. On examination, she was awake, alert, and oriented. Her pupils were 3 mm bilaterally equal and reactive to light. There was mild papilledema noted bilaterally. However, there were no other focal neurological deficits. She did not exhibit any cerebellar signs or gait disturbance at the time of examination. There was no neck stiffness. The magnetic resonance imaging (MRI) scan [
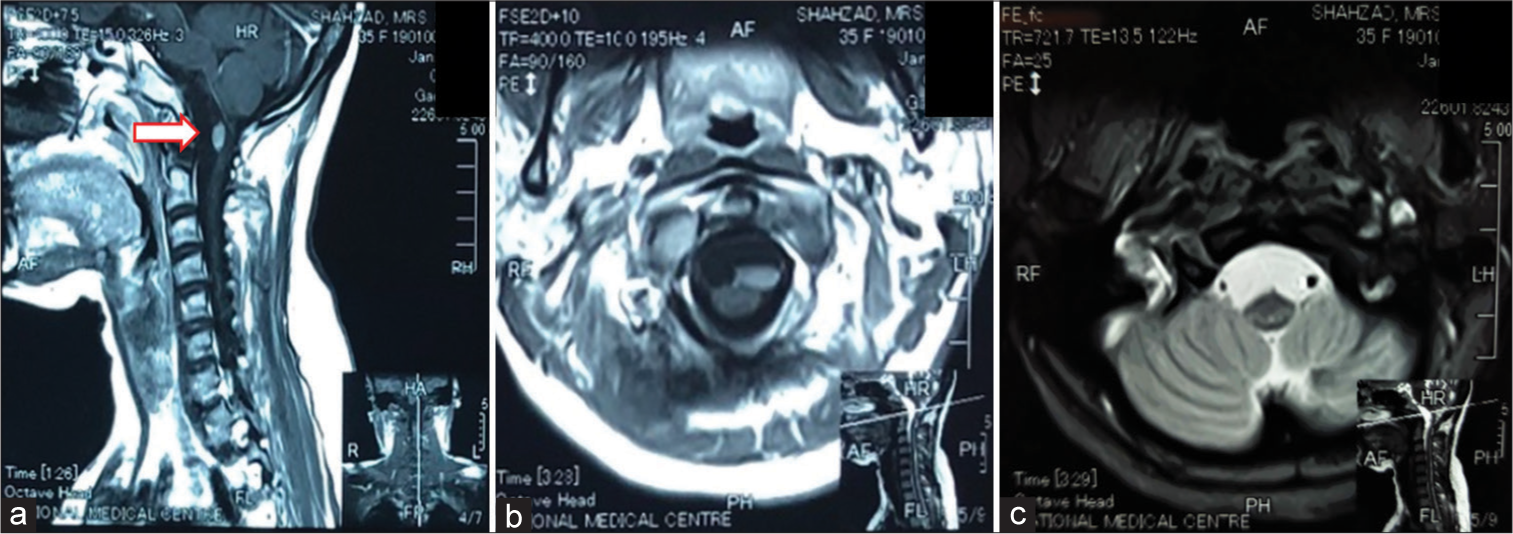
Since the neurological symptoms were not severe, she was advised to get a repeat MRI scan and come for an early follow-up. Depending on the progression of the symptoms, and increase in size of the cyst, the need for surgery would be determined. On her next follow-up visit 3 months later, her symptoms had significantly improved, with the vertigo controlled on use of prochlorperazine and headaches settled with over the counter analgesics. The repeat MRI scans [
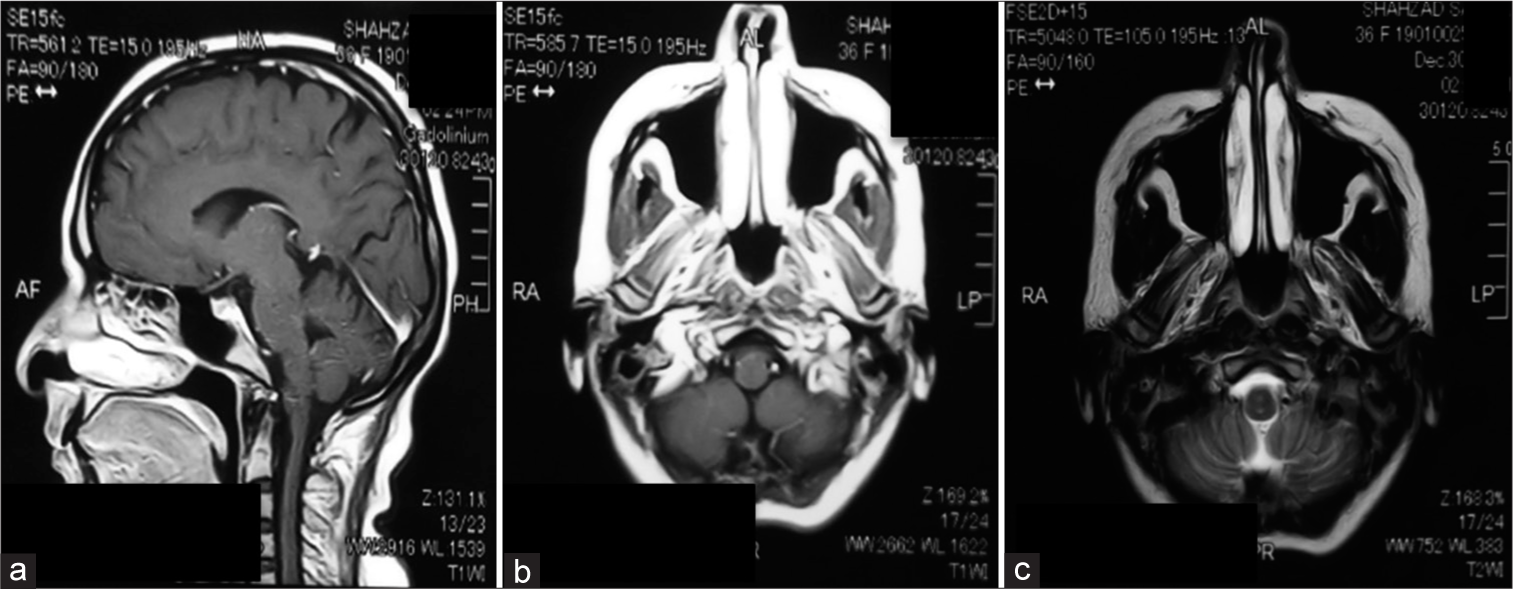
On her most recent follow-up, her MRI scan [
DISCUSSION
A case of self-resolving prepontine cyst was previously encountered at our institution in 2017.[
In our literature search, we were only able to find three reported cases of spontaneous resolution of prepontine cystic lesions. Two were pediatric patients[
Expanding our literature search to include all occurrences of prepontine cysts, we were able to find greater reporting for pediatric patients. This is understandable as these lesions are often derived from the remnants of embryological tissue. Adult population cases are rarely reported as we have seen.
The mainstays of surgical intervention for prepontine cysts are stereotactic aspiration, microsurgical excision, and shunting.[
In adult patients diagnosed with such pathology, decision-making often rests on a few key factors: the onset and severity of the symptoms, particularly with regard to neurological status, radiological evidence of warning signs (obstructive hydrocephalus and mass effect), and the timeliness of radiological and clinical follow-ups in such patients.[
As mentioned above, although mostly the cases reported in literature have been dealt with surgically, our experience suggests that there is a potential for natural resolution, and an expectant management can be deemed a reasonable alternative if the patient is clinically stable and followed closely.
CONCLUSION
This case highlights the possibility of close observation as a management option in a subset of patients with symptomatic prepontine cysts. These patients need close observation and follow-up to watch for worsening of the disease. We need to corroborate this viewpoint with further case reports and a case series to elaborate the natural history of the pathology in such patients.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Basheer N, Kasliwal MK, Suri A, Sharma MC, Arora A, Sharma BS. Lateral extradural, supratentorial neurenteric cyst. J Clin Neurosci. 2010. 17: 639-41
2. Bejjani GK, Wright DC, Schessel D, Sekhar LN. Endodermal cysts of the posterior fossa: Report of three cases and review of the literature. J Neurosurg. 1998. 89: 326-35
3. Berger MS, Wilson CB. Epidermoid cysts of the posterior fossa. J Neurosurg. 1985. 62: 214-9
4. Chen CY, Wong JS, Hsieh SC, Chu JS, Chan WP. Intracranial epidermoid cyst with hemorrhage: MR imaging findings. Am J Neuroradiol. 2006. 27: 427-9
5. Chowdhury FH, Haque MR, Sarker MH. Intracranial epidermoid tumor; microneurosurgical management: an experience of 23 cases. Asian J Neurosurg. 2013. 8: 21
6. Dodd RL, Barnes PD, Huhn SL. Spontaneous resolution of a prepontine arachnoid cyst. Pediatr Neurosurg. 2002. 37: 152-7
7. Fitzpatrick M, Barlow P. Endoscopic treatment of prepontine arachnoid cysts. Br J Neurosurg. 2001. 15: 234-8
8. Hao S, Tang J, Wu Z, Zhang L, Zhang J, Wang Z. Natural malignant transformation of an intracranial epidermoid cyst. J Form Med Assoc. 2010. 109: 390-6
9. Kachhara R, Bhattacharya R, Radhakrishnan V. Epidermoid cyst involving the brain stem. Acta Neurochir. 2000. 142: 97-100
10. Oprişan A, Popescu BO. Intracranial cysts: An imagery diagnostic challenge. Sci World J. 2013. 2013: 172154
11. Sugata J, Ueda T, Tanoue N, Hirahara K, Kamimura K, Arita K. A midline prepontine cyst: Serial magnetic resonance imaging over 20 years shows very slow growth after its rapid shrinkage. Neuroradiol J. 2019. 32: 98-102
12. Vinchon M, Pertuzon B, Lejeune JP, Assaker R, Pruvo JP, Christiaens JL. Intradural epidermoid cysts of the cerebellopontine angle: Diagnosis and surgery. Neurosurgery. 1995. 36: 52-7
13. Waqas M, Khan I, Khawaja R, Quddusi A, Enam A. Selfresolving prepontine cyst. Surg Neurol Int. 2017. 215: 1
14. Weber F.editors. The Prevalence of Intracranial Arachnoid Cysts: Arachnoid Cysts. Amsterdam, Netherlands: Elsevier; 2018. p. 95-100
15. Yaşargil MG, Abernathey CD, Sarioglu AÇ. Microneurosurgical treatment of intracranial dermoid and epidermoid tumors. Neurosurgery. 1989. 24: 561-7
16. Zhou LF. Intracranial epidermoid tumours: Thirty-seven years of diagnosis and treatment. Br J Neurosurg. 1990. 4: 211-6