- Medical College of Georgia at Augusta University, Augusta, Georgia, United States
- Department of Neurosurgery, Medical College of Georgia at Augusta University, Augusta, Georgia, United States
- Department of Endocrinology, Medical College of Georgia at Augusta University, Augusta, Georgia, United States
- Department of Neurology, Medical College of Georgia at Augusta University, Augusta, Georgia, United States
- Department of Hematology/Oncology, Medical College of Georgia at Augusta University, Augusta, Georgia, United States
- Department of Pathology, Medical College of Georgia at Augusta University, Augusta, Georgia, United States
- Department of Neurology and Oncology, Medical College of Georgia at Augusta University, Augusta, Georgia, United States
Correspondence Address:
Molly Butler, Medical College of Georgia at Augusta University, Augusta, Georgia, United States.
DOI:10.25259/SNI_956_2024
Copyright: © 2025 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Molly Butler1, Christopher Carr2, Mehul Mehra2, Anne Marie Barnett3, Jacey Salley4, Ayushi Chauhan5, Sami Belakhlef6, Gerald C. Wallace IV7, Martin Rutkowski2, John Vender2, Fernando L. Vale2. Presentation of extranodal NK/T-cell lymphoma as a pituitary mass: A case report and review of the literature. 11-Apr-2025;16:136
How to cite this URL: Molly Butler1, Christopher Carr2, Mehul Mehra2, Anne Marie Barnett3, Jacey Salley4, Ayushi Chauhan5, Sami Belakhlef6, Gerald C. Wallace IV7, Martin Rutkowski2, John Vender2, Fernando L. Vale2. Presentation of extranodal NK/T-cell lymphoma as a pituitary mass: A case report and review of the literature. 11-Apr-2025;16:136. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=13491
Abstract
BackgroundPrimary pituitary lymphomas are uncommon neoplasms that are typically derived from a B-cell lineage. Extranodal natural killer (NK)/T-cell lymphoma is distinct from B- and T-cell lymphomas and is associated with Epstein–Barr virus infection. Primary central nervous system (CNS) presentations of this neoplasm are exceptionally rare. Here, we report the case of extranodal NK/T-cell lymphoma presenting as a pituitary mass and review the literature related to this rare clinical entity.
Case DescriptionA 31-year-old previously healthy male presented with 2 weeks of progressive headaches and ophthalmoplegia. Imaging revealed a large intrasellar mass with retroclival extension and involvement of the sphenoid and cavernous sinuses. An endoscopic biopsy of the sphenoidal mucosa was performed, and pathological examination was consistent with extranodal NK/T-cell lymphoma. Despite treatment with chemo- and radiotherapy, the patient died approximately 8 months after initial presentation due to systemic disease progression with multiorgan failure.
ConclusionThe presentation of extranodal NK/T-cell lymphoma as a pituitary lesion is very rare, having been reported only twice in the previous literature. Patients with primary CNS extranodal NK/T-cell lymphoma typically experience an aggressive clinical course with a poor prognosis, as in our case.
Keywords: Biopsy, Headache, Neoplasms, Ophthalmoplegia, T-lymphocytes
INTRODUCTION
Extranodal natural killer (NK)/T-cell lymphomas are rare, aggressive neoplasms related to Epstein–Barr virus (EBV) infection.[
CASE DESCRIPTION
A 31-year-old Filipino male with no significant past medical history presented to us with approximately 10 days of diplopia, progressive headache, and nausea. The patient sought medical attention at an outside hospital when his diplopia began, endorsing a sudden onset of impaired left eye movement. He was reportedly found to have a pituitary mass at that time and was subsequently discharged with a scheduled outpatient ophthalmology appointment. During this appointment, he was noted to have bilateral cranial nerve IV palsies and was directed to the emergency department at our institution. Further history from the patient was notable for 1 year of gradually escalating headaches and night sweats. He also endorsed approximately 2 weeks of decreased libido, absence of morning erections, and fatigue. On physical examination, he had moderate left ptosis with impaired left abduction and adduction consistent with third and sixth cranial nerve palsies, in addition to a right sixth cranial nerve palsy.
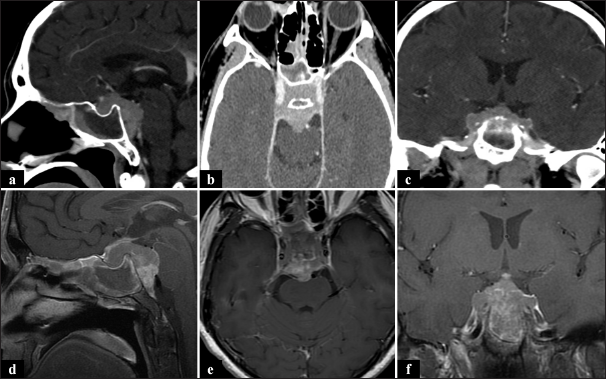
The patient’s prolactin level was normal, but laboratory analysis revealed low luteinizing hormone and thyroid-stimulating hormone, consistent with hypopituitarism. A head computed tomography scan was obtained, which demonstrated a complex and partially erosive mass involving the sphenoid sinus, sella, and clivus [
Figure 1:
(a-c) Head computed tomography with contrast demonstrating an enhancing mass in the sellar/suprasellar region and additional multifocal areas of mucosal thickening and enhancement along the walls of the sphenoid sinus. (d-f) T1-weighted contrast-enhanced magnetic resonance imaging demonstrating a contrast-enhancing mass centered on the sella and cavernous sinuses.
The patient underwent an endoscopic transnasal transsphenoidal biopsy, and an extremely abnormal appearing sphenoid mucosa was noted intraoperatively. Multiple biopsies of the intrasphenoidal tissue were obtained and sent for the frozen section. Upon review of the frozen specimens, it was clear that this was an invasive tumor highly consistent with lymphoma. Additional intrasphenoidal specimens were obtained for further analyses. We elected not to obtain biopsies from the intrasellar space as our collected specimens were felt to be adequate for tissue diagnosis. The exposure was closed, and the patient tolerated the procedure without complications. Histologic sections demonstrated sinonasal mucosa involved by a diffuse lymphocytic infiltrate consisting of medium-to-large monomorphic cells with round to irregular nuclei with numerous apoptotic bodies and foci of necrosis. As shown in
Oncologic treatment with the modified steroid, methotrexate, ifosfamide, L-asparaginase, and etoposide (SMILE) protocol was initiated, consisting of dexamethasone, methotrexate, ifosfamide, peg-asparaginase, and etoposide given every 3 weeks.[
DISCUSSION
Pituitary neoplasms are highly prevalent and commonly benign, with adenomas accounting for approximately 90% of all pituitary tumors.[
In our review of the literature, we identified only two cases of extranodal NK/T-cell lymphoma manifesting as a primary pituitary tumor. The first case, published in 2007, reports a 26-year-old male who presented with headache, diplopia, nausea, vomiting, and fever. Laboratory analysis revealed hypocortisolism, hypothyroidism, and hypotestosteronemia.[
In the present article, we report the third published case of extranodal NK/T-cell pituitary lymphoma. Our patient similarly presented with headache, visual changes, and hypopituitarism and experienced a clinical course much like the first patient reported by Liu et al.[
PPL is regarded as a subtype of PCNSL, but it has been argued that it may be a distinct entity considering the difference in embryologic origins between the pituitary gland and the CNS parenchyma.[
CONCLUSION
Extranodal NK/T-cell lymphoma is an uncommon neoplasm that is distinct from B- and T-cell lymphomas. Primary CNS presentations are exceptionally rare, and only three cases, including ours, have described the presentation of extranodal NK/T-cell lymphoma as a pituitary mass. Patients with primary CNS extranodal NK/T-cell lymphoma typically experience an aggressive clinical course with a poor prognosis. PPLs, though also rare tumors, are typically of B-cell origin and commonly involve the sphenoid sinus. Biopsy of sphenoid mucosa may be a safer alternative to pituitary biopsy for diagnosis and should be considered in appropriate cases.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Alaggio R, Amador C, Anagnostopoulos I, Attygalle AD, de Oliveira Araujo IB, Berti E, editors. The 5th edition of the World Health Organization classification of haematolymphoid tumours: Lymphoid neoplasms. Leukemia. 2022. 36: 1720-48
2. Duan L, Liu J, Zhang Y, Cui L, Zhai X, Pan B. Primary pituitary lymphoma in immunocompetent patients: A report on two case studies and the review of literature. Front Endocrinol (Lausanne). 2020. 11: 562850
3. Erdag N, Bhorade RM, Alberico RA, Yousuf N, Patel MR. Primary lymphoma of the central nervous system: typical and atypical CT and MR imaging appearances. AJR Am J Roentgenol. 2001. 176: 1319-26
4. Ferrante E, Ferraroni M, Castrignanò T, Menicatti L, Anagni M, Reimondo G. Non-functioning pituitary adenoma database: A useful resource to improve the clinical management of pituitary tumors. Eur J Endocrinol. 2006. 155: 823-9
5. Ghione P, Qi S, Imber BS, Seshan V, Moskowitz A, Galasso N. Modified SMILE (mSMILE) and intensity-modulated radiotherapy (IMRT) for extranodal NK-T lymphoma nasal type in a single-center population. Leuk Lymphoma. 2020. 61: 3331-41
6. Grommes C, DeAngelis LM. Primary CNS lymphoma. J Clin Oncol. 2017. 35: 2410-8
7. Jaffe ES, editors. World Health Organization classification of tumors. Pathology and genetics of tumors of hematopoietic and lymphoid tissues. France: IARC Publications; 2001. p. 185-7
8. Kashyap R, Rai Mittal B, Manohar K, Harisankar CN, Bhattacharya A, Singh B. Extranodal manifestations of lymphoma on [18F]FDG-PET/CT: A pictorial essay. Cancer Imaging. 2011. 11: 166-74
9. Landman RE, Wardlaw SL, McConnell RJ, Khandji AG, Bruce JN, Freda PU. Pituitary lymphoma presenting as fever of unknown origin. J Clin Endocrinol Metab. 2001. 86: 1470-6
10. Liu JK, Sayama C, Chin SS, Couldwell WT. Extranodal NK/T-cell lymphoma presenting as a pituitary mass: Case report and review of the literature. J Neurosurg. 2007. 107: 660-5
11. Matsuyama J, Harada Y. Pituitary adenomas invading the sphenoid sinus. Skull Base. 2006. 16: A058
12. Melmed S, Kaiser UB, Lopes MB, Bertherat J, Syro LV, Raverot G. Clinical biology of the pituitary adenoma. Endocr Rev. 2022. 43: 1003-37
13. Metgud RS, Doshi JJ, Gaurkhede S, Dongre R, Karle R. Extranodal NK/T-cell lymphoma, nasal type (angiocentric T-cell lymphoma): A review about the terminology. J Oral Maxillofac Pathol. 2011. 15: 96-100
14. Pongpruttipan T, Sukpanichnant S, Assanasen T, Wannakrairot P, Boonsakan P, Kanoksil W. Extranodal NK/T-cell lymphoma, nasal type, includes cases of natural killer cell and αβ, γδ, and αβ/γδ T-cell origin: A comprehensive clinicopathologic and phenotypic study. Am J Surg Pathol. 2012. 36: 481-99
15. Qin L, Li Y, He Y, Zeng R, Pan T, Zuo Y. Successful treatment of primary CNS Extranodal NK/T-Cell lymphoma with surgery and chemotherapy combined with sintilimab: A case report and literature review. Onco Targets Ther. 2022. 15: 1-11
16. Ramakrishnan VR, Suh JD, Lee JY, O’Malley BW, Grady MS, Palmer JN. Sphenoid sinus anatomy and suprasellar extension of pituitary tumors: Clinical article. J Neurosurg. 2013. 119: 669-74
17. Sánchez-Romero C, Bologna-Molina R, Paes de Almeida O, Santos-Silva AR, Prado-Ribeiro AC, Brandão TB. Extranodal NK/T cell lymphoma, nasal type: An updated overview. Crit Rev Oncol Hematol. 2021. 159: 103237
18. Tarabay A, Cossu G, Berhouma M, Levivier M, Daniel RT, Messerer M. Primary pituitary lymphoma: An update of the literature. J Neurooncol. 2016. 130: 383-95
19. Tse E, Kwong YL. The diagnosis and management of NK/T-cell lymphomas. J Hematol Oncol. 2017. 10: 85
20. Velho V, Guha A, Naik H, Bhople L, Jain N. Unravelling hitherto unreported masses camouflaged as pituitary macro adenomas. Asian J Neurosurg. 2018. 13: 1005-7
21. Villwock JA, Villwock M, Deshaies E, Goyal P. Significant increases of pituitary tumors and resections from 1993 to 2011. Int Forum Allergy Rhinol. 2014. 4: 767-70
22. Wu W, Ren K, Li N, Luo Q, Zhou H, Hai T. Central nervous system involvement at initial diagnosis of extranodal NK/T-cell lymphoma: A retrospective study of a consecutive 12-year case series. Ann Hematol. 2023. 102: 829-39
23. Yang XL, Liu YB. Advances in pathobiology of primary central nervous system lymphoma. Chin Med J (Engl). 2017. 130: 1973-9
24. Yu F, Wang J, Ke Z, Zhang Y, Xu L, Zhang H. EBV-positive Nodal T-Cell and NK-Cell Lymphoma: A Study of 26 cases including a subset with strong CD30 expression mimicking anaplastic large cell lymphoma. Am J Surg Pathol. 2024. 48: 406-16