- Department of Neurosurgery, All India Institute of Medical Sciences, Patna, Bihar, India
- Department of Obstetrics and Gynecology, All India Institute of Medical Sciences, Patna, Bihar, India
Correspondence Address:
Vikas Chandra Jha, Department of Neurosurgery, All India Institute of Medical Sciences, Patna, Bihar, India.
DOI:10.25259/SNI_965_2024
Copyright: © 2025 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Vikas Chandra Jha1, Rahul Jain1, Achintya Ajaya1, Sangam Jha2, Gaurav Verma1, Nikhil Dhage1, Anant Parashar1, Vivek Sharan Sinha1, Nitish Kumar1. Primary congenital intracranial lipoma with extracranial extension in a pediatric patient: A case report and literature review. 07-Mar-2025;16:80
How to cite this URL: Vikas Chandra Jha1, Rahul Jain1, Achintya Ajaya1, Sangam Jha2, Gaurav Verma1, Nikhil Dhage1, Anant Parashar1, Vivek Sharan Sinha1, Nitish Kumar1. Primary congenital intracranial lipoma with extracranial extension in a pediatric patient: A case report and literature review. 07-Mar-2025;16:80. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=13432
Abstract
BackgroundCongenital intracranial lipomas are rare, representing only 0.1–0.5% of brain tumors, and are typically asymptomatic. An extracranial component is exceedingly rare, usually reported in slow-growing adult cases. This report presents a unique case of a rapidly growing congenital intracranial lipoma with extracranial extension in a pediatric patient.
Case DescriptionA 3-year-old girl with a progressively enlarging forehead mass, present since birth, was found to have a large interhemispheric lipoma (12 × 10 × 9 cm) extending into the left lateral ventricle and connected to an extracranial mass (17 × 10 × 10 cm) through a frontal bone defect. Additional findings included corpus callosal agenesis and venous drainage from the scalp lesion into the superior sagittal sinus. The microsurgical intervention involved the excision of the extracranial lipoma and subtotal resection of the intracranial component, preserving critical neurovascular structures.
ConclusionThis case of rapid lipoma growth in a pediatric patient is atypical, differing from slow-growing, asymptomatic presentations in adults. High-magnification microsurgery and Doppler guidance facilitated safe resection with a positive outcome. This case highlights the need for further research into developmental factors and rapid growth mechanisms in pediatric intracranial lipomas with extracranial components, potentially representing a distinct clinical entity.
Keywords: Extracranial extension, Microsurgery, Outcome, Pediatric intracranial lipoma
INTRODUCTION
Intracranial lipomas are rare, constituting only 0.1–0.5% of all primary brain tumors.[
Intracranial lipomas tend to be positioned near midline structures, frequently appearing in cerebral cisterns such as the quadrigeminal, superior cerebellar peduncle, suprasellar, cerebellopontine angle, and Sylvian cisterns. Their morphology can vary; posterior lesions, typically smaller, are often curvilinear and situated near the corpus callosum, whereas larger, tubulonodular forms are more likely found anteriorly.[
Several hypotheses have been proposed to elucidate the genesis of intracranial lipomas, though much remains uncertain, especially regarding cases with both intracranial and extracranial components.[
CASE DETAILS
A 3-year-old girl presented with a progressively enlarging forehead mass that had been present since birth. The lesion was initially the size of a lemon; however, it increased to the current size of presentation within the previous 1 year. Clinical examination showed a firm, subcutaneous lesion over the frontal region, accompanied by distinct craniofacial features, including hypertelorism (increased distance between the eyes), a flattened nasal bridge, and low-set ears [
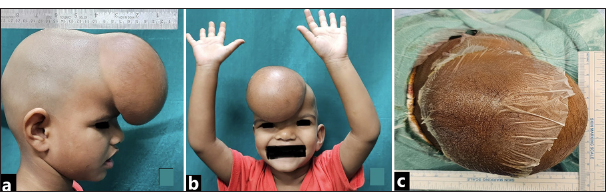
Figure 1:
(a) Preoperative clinical photograph of a 5-year-old male presenting with a frontal subcutaneous lipoma. The lesion, initially noticed after the 1st year of life, has rapidly grown in the past year, impairing vision and causing progressive headaches. The right lateral view shows the lesion’s extracranial portion, measuring approximately 15 cm × 10 cm × 10 cm, with a similar dimension intracranially, connected by a lipofibromatous band, as observed intraoperatively in subsequent images. (b) Preoperative frontal photograph illustrating the patient’s hypertelorism and forehead swelling, with no focal neurological deficit. (c) Preoperative image from the cranial end, showing external measurement of the lipoma dimensions (15 cm × 10 cm) with a scale.
Initial imaging with a non-contrast computed tomography scan of the head identified a well-defined, fat-density mass in the subcutaneous plane of the forehead [
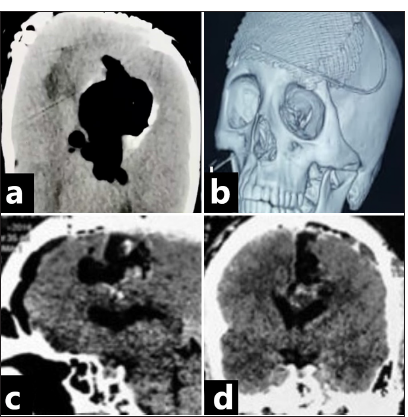
Figure 2:
(a) Preoperative noncontrast computed tomography (NCCT) axial head scan, showing a hypodense mass in the anterior interhemispheric fissure extending anteriorly, with associated bony defect. (b) Preoperative 3D reconstruction of NCCT showing a midline calvarial defect with bony deformation. (c) Magnetic resonance imaging (MRI) T1-weighted axial view showing a hyperintense mass in the anterior interhemispheric fissure, compressing the frontal horns of the bilateral lateral ventricles and extending into the body of the left lateral ventricle. (d) MRI T2-weighted (T2W) axial view revealing a hyperintense mass in the anterior interhemispheric fissure with flow voids, including an intralesional vessel traversing the lesion anteriorly and another flow void in the extracranial portion. (e) MRI T2W sagittal section demonstrating the intracranial interhemispheric lipoma, with a connecting stalk to the extracranial scalp lesion in the subcutaneous plane in the frontal region. Agenesis of the corpus callosum is noted posteroinferiorly. (f) MRI T2W coronal section showing the anterior cerebral arteries passing through the lesion.
A subsequent brain magnetic resonance imaging (MRI) provided greater detail, showing a non-enhancing, lobulated mass measuring 12 cm × 10 cm × 9 cm within the anterior interhemispheric fissure, extending into the left lateral ventricle. The lesion displayed a characteristic fat signal across all sequences, with peripheral blooming seen on susceptibility-weighted imaging. A large fat-density subcutaneous lesion (15 cm × 10 cm × 10 cm) was also observed in the frontal region, connected to the interhemispheric lesion by a thin lipomatous stalk. The MRI also confirmed corpus callosal agenesis and venous drainage from the scalp lesion into the superior sagittal sinus. The distal A2 and A3 segments of both anterior cerebral arteries were observed traversing the interhemispheric lipoma [
The surgical approach involved excising the frontal subcutaneous lipoma and the affected bone, resecting the connecting lipomatous stalk, and performing a subtotal excision of the interhemispheric lipoma [
Figure 3:
(a) Intraoperative photograph post-scalp incision, revealing a subcutaneous lipomatous mass overlying the dura in the midline. (b) Intraoperative image after dural elevation, showing dilated, tortuous cortical veins in the anterior frontal cortex on the right, mirrored on the contralateral side. (c) Intraoperative photograph displaying the lipomatous mass following excision. (d) Post-excision intraoperative image showing the dura repair with a synthetic graft and titanium mesh cranioplasty following maximal safe resection of the intracranial lipoma and extracranial mass excision.
Reconstruction was completed with titanium mesh cranioplasty. The procedure and postoperative course were smooth, and the patient experienced no neurological deficits [
Figure 4:
(a) Postoperative axial magnetic resonance imaging brain with contrast, taken at 18 months follow-up, showing successful excision of the lipoma’s extracranial and intracranial portions, with no ventriculomegaly or recurrence. (b) Follow-up 3D coronal front view of the head at 18 months, showing no residual bony defect and tissue growth over the titanium mesh, restoring the contour and covering the bony defect. (c) Postoperative sagittal non-contrast computed tomography (NCCT) brain at 18 months follow-up shows excision with postoperative changes, absence of lesion regrowth, and no ventriculomegaly. (d) Postoperative coronal NCCT brain with contrast at 18 months follow-up, revealing no ventriculomegaly or recurrence of the lipoma, with postoperative changes.
DISCUSSION
Primary congenital multiple intracranial lipomas with an extracranial component are rare, and very few case reports are available[
Most patients in the presenting age group are asymptomatic, and such rapid growth has not been reported. The condition causes visual difficulties and difficulty breathing due to the projecting frontal mass compressing the root of the nose, causing hypertelorism and obstruction in vision. This patient had no history of seizure, headache, papilledema, or any neurological deficit reported in earlier reported symptomatic cases. In this patient, the involvement of interhemispheric fissure and extension along fissures to lateral ventricle was probably going to cause a mass effect and features of obstructive hydrocephalus, so we planned for microsurgical intervention and correction of cosmetic issues caused by the projection of subcutaneous mass and the defect in the frontal bone. Different studies have reported poor results for surgical excision.[
We want to convey that even though we operated on our patient as she showed rapid growth of lipoma as per description by the patient’s parents, who gave a history of extracranial component size increase as the reason they decided to seek medical opinion, based on previous studies that we opted for maximal safe resection of lipoma to avoid potential long-term deficits arising out of vascular injury.
CONCLUSION
This case highlights the rare presentation of primary congenital multiple intracranial lipomas with an extracranial component in a pediatric patient, contrasting with the typical slow-growing, asymptomatic nature of such lesions predominantly observed in adults. The rapid growth and large size of the lipoma underscore the possibility of atypical developmental pathways, suggesting a need for further research into the embryological origins and molecular mechanisms driving accelerated growth in pediatric lipomas. Microsurgical excision was essential not only to alleviate potential mass effects and prevent complications like obstructive hydrocephalus but also to address cosmetic concerns associated with extracranial extension. High-magnification microscopy and intraoperative Doppler guidance proved instrumental in achieving safe, near-total resection with excellent outcomes and no neurological deficits. This case underscores the importance of precise surgical techniques and may inform future management strategies, especially for pediatric patients with large congenital lipomas with extracranial extensions.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Aggarwal N, Gehlot KB, Kumar SD, Khan NK. Frontal subcutaneous lipoma associated with interhemispheric lipoma, lipomeningocele, and corpus callosal dysgenesis in a young adult: CT and MRI findings. Indian J Radiol Imaging. 2018. 28: 22-6
2. Alam A, Sree Ram MN, Sahu S. Lipoma of the corpus callosum: Diagnosis using magnetic resonance imaging. Med J Armed Forces India. 2006. 62: 299-300
3. Chao SC, Shen CC, Cheng WY. Microsurgical removal of sylvian fissure lipoma with pterion keyhole approach-case report and review of the literature. Surg Neurol. 2008. 70: 85-90
4. Charry JD, Calle-Toro J, Serrano S, Areiza J, Gutiérrez D, Caquimbo L. Lipoma of the callosum corpus: A case report and literature review. Rev Chil Neurocir. 2021. 46: 98-101
5. El Marrakchi M, Zian N, Hajhouji F, Laghmari M, Ghannane H, Jallo G. Association of limited dorsal myeloschizis and corpus callosum lipoma: A case report and literature review. Surg Neurol Int. 2024. 15: 151
6. Elgassim MA, Wafer A, Ahmed A, Elfaki A, Satti A, Anjum S. Intracranial lipoma extending extracranially in a five-year-old patient. Cureus. 2022. 14: e21816
7. Given CA, Fields TM, Pittman T. Interhemispheric lipoma connected to subcutaneous lipoma via lipomatous stalk. Pediatr Radiol. 2005. 35: 1110-2
8. Jiménez Caballero PE. Interhemispheric lipoma associated with agenesis of the corpus callosum. Neurologia. 2012. 27: 515-7
9. Karabağ H, Cakmak E, Celik B, Iplikçioğlu AC. Pericallosal lipoma associated with subcutaneous lipoma in an adult. J Neurosci Rural Pract. 2014. 5: 91-3
10. Karakas O, Karakas E, Boyacı FN, Celik B, Cullu N. Anterior interhemispheric calcified lipoma together with subcutaneous lipoma and agenesis of corpus callosum: A rare manifestation of midline craniofacial dysraphism. Jpn J Radiol. 2013. 31: 496-9
11. Konomatsu K, Kakisaka Y, Sato S, Kubota T, Soga T, Ukishiro K. “Caterpillar sign” in corpus callosum associated with curvilinear pericallosal lipoma in MRI: A case report. Radiol Case Rep. 2024. 19: 2058-61
12. Kudoh H, Sakamoto K, Kobayashi N. Lipomas in the corpus callosum and the forehead, associated with a frontal bone defect. Surg Neurol. 1984. 22: 503-8
13. Mitilian D, Haddad D, Lenoir M, Boudjemaa S, Vazquez MP, Picard A. Interhemispheric lipoma associated with frontal subcutaneous lipoma. J Plast Reconstr Aesthet Surg. 2009. 62: e427-9
14. Rana D, Kulkarni S, Zuberi J, Berlin F. Frontal subcutaneous lipoma associated with large interhemispheric lipoma and corpus callosum agenesis. Radiol Case Rep. 2021. 17: 816-20
15. Sari A, Dinç H, Gümele HR. Interhemispheric lipoma associated with subcutaneous lipoma. Eur Radiol. 1998. 8: 628-30
16. Seidl Z, Vaneckova M, Vitak T. Intracranial lipomas: a retrospective study. Neuroradiol J. 2007. 28: 30-6
17. Taglialatela G, Galasso R, Taglialatela G, Conforti R, Volpe A, Galasso L. Lipomas of corpus callosum. Neuroanatomy. 2009. 8: 39-42
18. Thapa Ashish Jung. Lipoma of the corpus callosum: Fat in the brain. Nepal Journal of Neuroscience. 2021. 18: 76-9
19. Truwit CL, Barkovich AJ. Pathogenesis of intracranial lipoma: an MR study in 42 patients. AJNR Am J Neuroradiol. 1990. 11: 665-74
20. Yildiz H, Hakyemez B, Koroglu M, Yesildag A, Baykal B. Intracranial lipomas: importance of localization. Neuroradiology. 2006. 48: 1-7
21. Yilmaz MB, Genc A, Egemen E, Yilmaz S, Tekiner A. Pericallosal lipomas: A series of 10 cases with clinical and radiological features. Turk Neurosurg. 2016. 26: 364-8