- Department of Neurosurgery, Southern Tohoku General Hospital, Koriyama, Japan.
- Department of Neurosurgery, Tokyo D Tower Hospital, Koto-Ku, Japan
- Department of Neuroradiology, Southern Tohoku General Hospital, Koriyama, Japan.
Correspondence Address:
Yuta Kobayashi, Department of Neurosurgery, Southern Tohoku General Hospital, Koriyama, Japan.
DOI:10.25259/SNI_106_2024
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Yuta Kobayashi1, Shunsuke Satoh1, Yugo Kishida2, Hiromi Goto1, Daichi Fujimori1, Akinori Onuki1, Kazuo Watanabe1, Noriaki Tomura3. Primary intraosseous cavernous hemangioma of the clivus: A case report and literature review. 31-May-2024;15:177
How to cite this URL: Yuta Kobayashi1, Shunsuke Satoh1, Yugo Kishida2, Hiromi Goto1, Daichi Fujimori1, Akinori Onuki1, Kazuo Watanabe1, Noriaki Tomura3. Primary intraosseous cavernous hemangioma of the clivus: A case report and literature review. 31-May-2024;15:177. Available from: https://surgicalneurologyint.com/surgicalint-articles/12922/
Abstract
Background: The radiographic presentation of the primary intraosseous cavernous hemangiomas (PICHs) is nonspecific. We report a case of clival PICH mimicking a chordoma with a literature review.
Case Description: A 57-year-old woman presented with diplopia that started a few days before the presentation. She had transient diplopia at the right lateral gaze and upper gaze with normal eye movement. The symptoms disappeared spontaneously 1 week later. She had no other complaints or neurological deficits. Computed tomography revealed an intraosseous mass lesion and bone erosion of the middle and lower clivus, extending laterally to the right occipital condyle. Magnetic resonance imaging (MRI) showed hyperintense and hypointense components on T2- and T1-weighted images, respectively. The lesion was larger than on MRI performed 10 years earlier. Chordoma or chondroma was considered a possible preoperative diagnosis. An endoscopic transsphenoidal approach removed the tumor. In the operating view, the lesion appeared as “moth-eaten” bony interstices filled with vascular soft tissue. Histologically, an intraosseous cavernous hemangioma was diagnosed.
Conclusion: Diagnosis before surgery is difficult without characteristic radiographic findings. When making a differential diagnosis of malignant skull lesions, PICH should be considered.
Keywords: Case report, Cavernous hemangioma, Clivus, Endoscope, Transsphenoidal surgery
INTRODUCTION
Primary intraosseous cavernous hemangiomas (PICHs) are rare, benign osteolytic tumors that are vascular in origin. PICHs constitute 0.2% of all bone neoplasms [
CASE REPORT
History
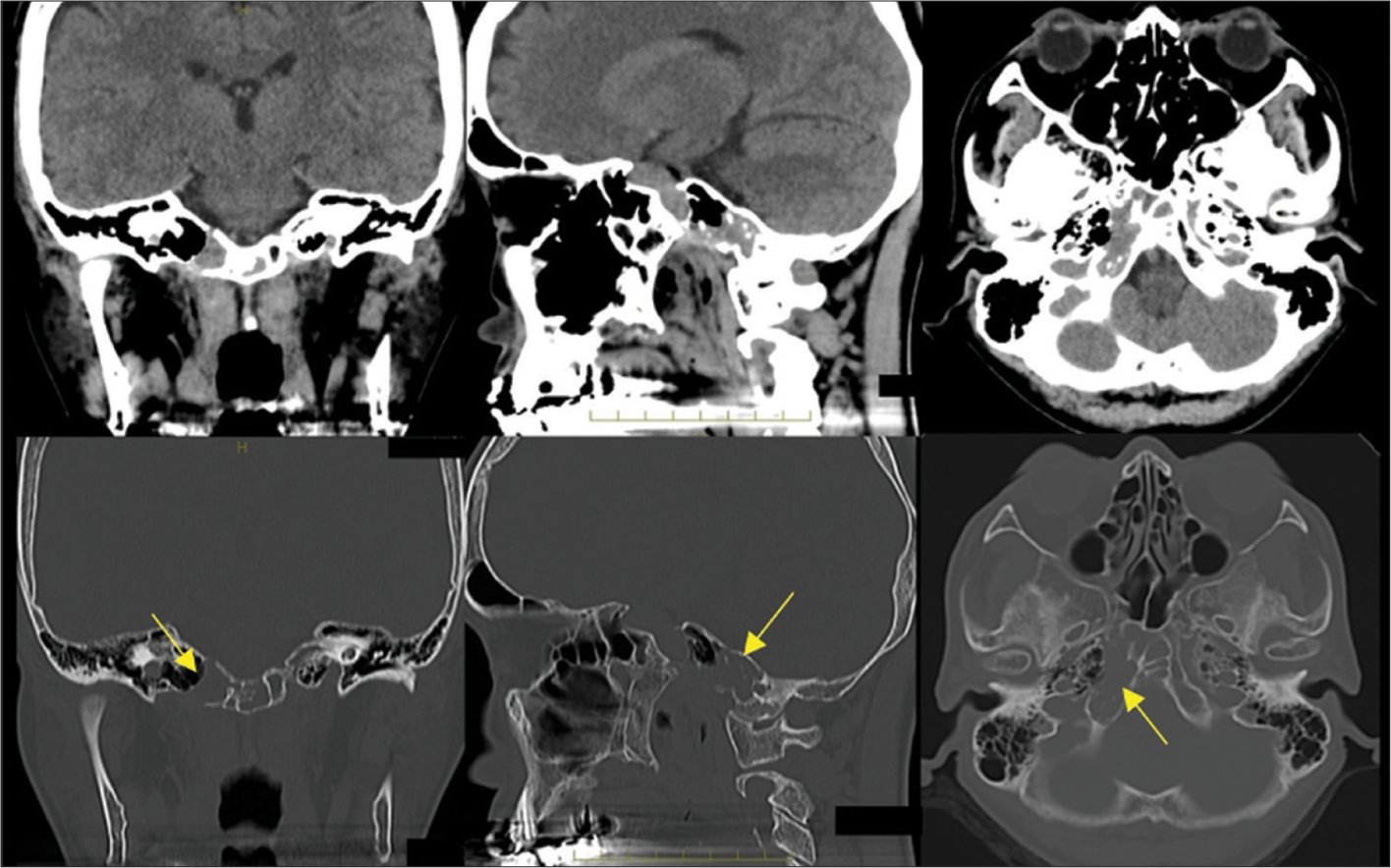
A 57-year-old woman came to our hospital with diplopia, which had started a few days before the presentation. At presentation, she had transient diplopia in the right lateral and upper gaze, with normal eye movement. Her symptoms disappeared spontaneously 1 week later, and she had no other symptoms or neurological deficits. Computed tomography (CT) showed an intraosseous mass lesion and bone erosion of the middle and lower clivus, extending laterally to the right occipital condyle [
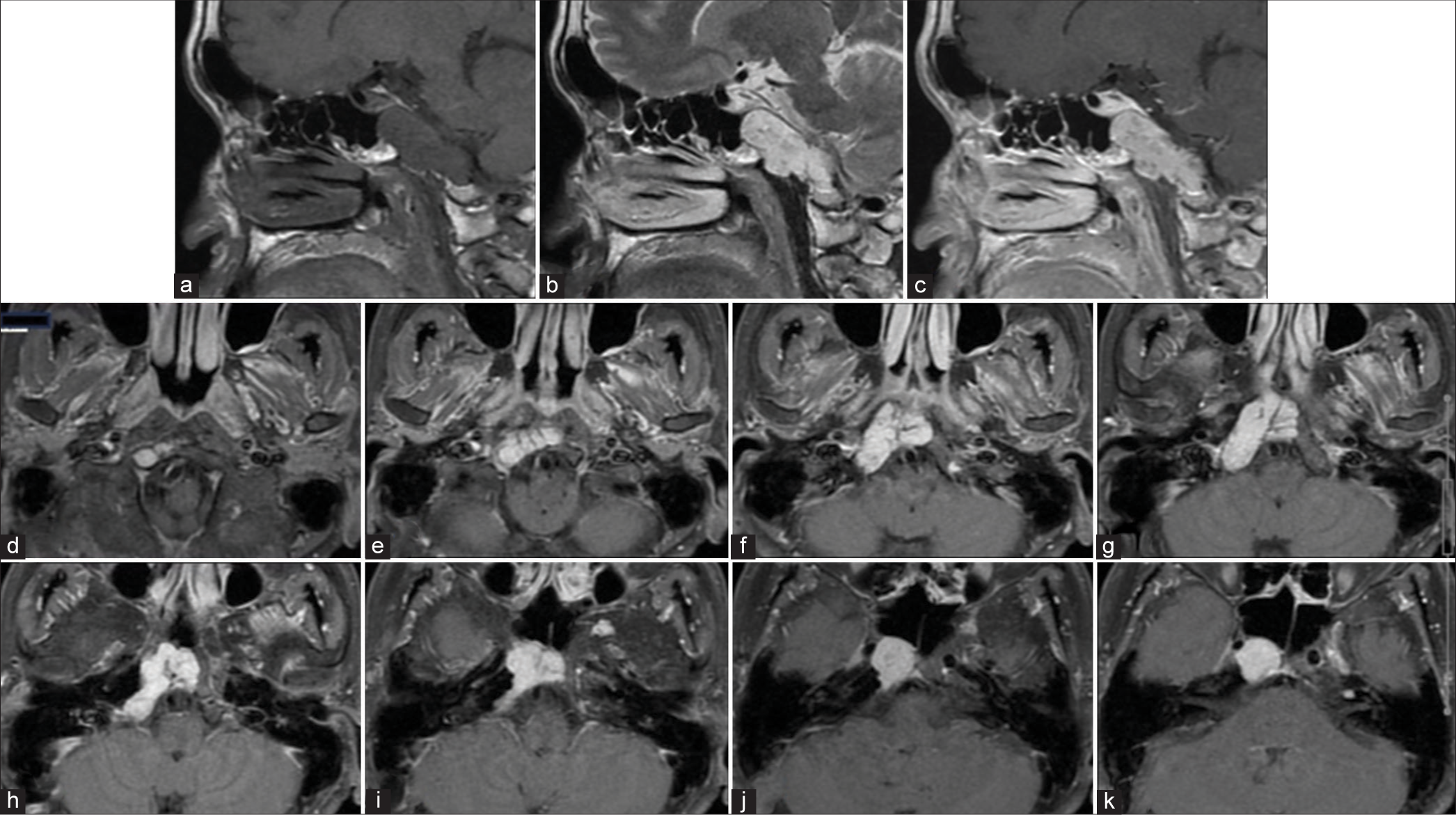
Figure 2:
(a) Magnetic resonance imaging showing hypointensity on T1-weighted imaging and (b) hyperintense components on T2-weighted imaging in the lesion. (c) After gadolinium administration, the tumor is markedly enhanced in a homogenous fashion. (d-k) The axial images show the tumor area. On the upper side, the tumor became markedly enhanced in a homogenous fashion. On the upper side, the tumor protrudes in the sphenoidal sinus.
Treatment
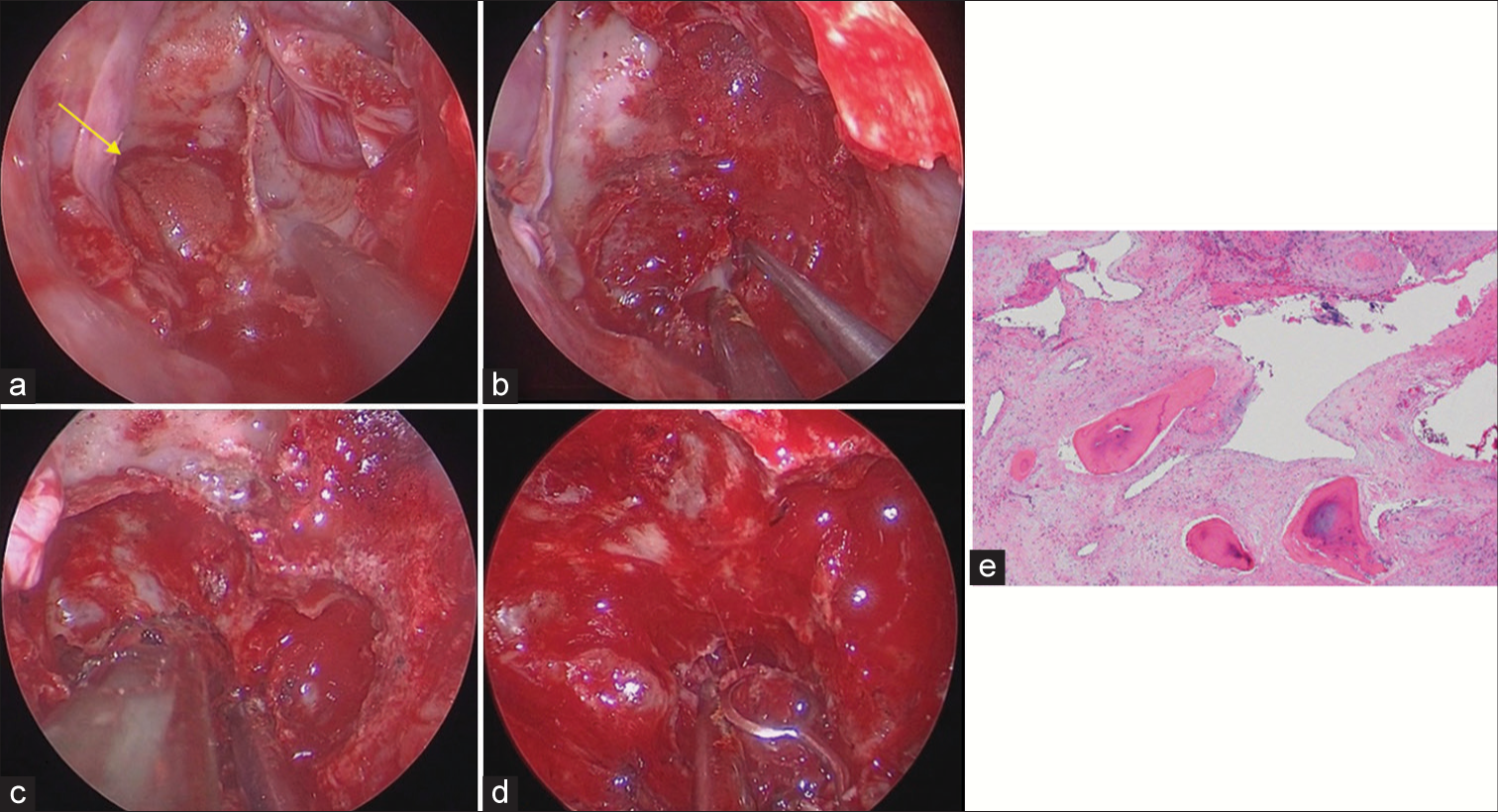
Tumor resection using an endoscopic transnasal transsphenoidal trans ethmoidal approach was planned. A surgical navigation system was used to aid in the intraoperative localization of the lesion. Tumor resection was performed through the right nasal cavity. Using a zero-degree endoscope, we opened the ethmoidal bra and posterior ethmoidal sinus and passed it to the sphenoidal sinus. The middle turbinate was translocated laterally, and the anterior wall of the sphenoid bone was drilled through the nasal septum. A protruding tumor was observed through the cortical bone [
Figure 3:
(a) Inside the sphenoid sinus, the protruding tumor (arrow) can be seen extending throughout the cortical bone. (b-d) Along the preserved cortical bone, the tumor was exfoliated and coagulated. (e) A single layer of flattened endothelial cells scattered amid bony trabeculae bordered the thin-walled vascular channels shown by pathological testing, which was consistent with an intraosseous cavernous hemangioma.
The gross inspection did not indicate the tumor to be either a chondroma or chondrosarcoma, and hemangioma was suspected. We subsequently exfoliated the preserved cortical bone and coagulated the tumor capsule. The tumor capsule was expansive, noninvasive in the bone, and contiguous in the multiple cavities. The cavities were opened with a drill, and the tumor was removed with the capsule preserved, and we did not encounter uncontrollable bleeding in that way [
The preserved mucous membrane of the sphenoid sinus was spread into the cavity and fixed with fibrin glue. Pathological examination revealed an intraosseous cavernous hemangioma [
Postoperative course
The patient was moved from the operating room to the intensive care unit following successful extubation. She remained at the neurological baseline and was transferred to the regular floor on the 1st postoperative day (POD).
She was discharged from the hospital on POD9 with her neurological condition stable. Postoperative MRI [
Figure 4:
(a) In the spoiled gradient recalled acquisition in the steady state-gradient refocused axial image and (b and c) T1-weighted magnetic resonance imaging using gadolinium-based contrast coronal and sagittal images, the residual tumor (arrows) can be seen in the central area of the clivus covered with the cortical bone.
DISCUSSION
PICHs are rare, benign, osteolytic tumors that are vascular in origin. PICHs generally occur in adults, and patients are predominantly women in their fourth–fifth decades of life. PICHs of the skull primarily affect the frontal and parietal bones but rarely involve the base of the skull.[
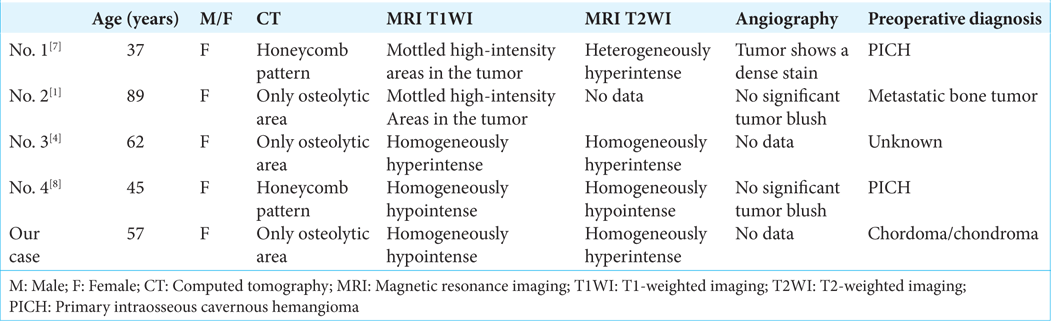
A review of the English literature revealed that only four reported cases of clival PICH were reported.[
Typical CT signs, such as a honeycomb pattern, are most likely helpful for diagnosis; however, some cases lack these findings.[
As very few cases of skull base PICH have been reported in the literature, there is currently no consensus on proper management.[
CONCLUSION
PICH of the skull base frequently mimics other, more typical tumors of the skull base, including chordoma. Herein, we reported a case of a clival PICH mimicking chordoma and further provided a review of all other previously reported cases. Symptoms at presentation varied in each case. In our case, she had transient diplopia. We believe that the cause of the transient symptom is that repeated bleeding and fluctuated size of PICH made compression to the VIth cranial nerve stronger temporarily. Diagnosis of PICH before surgery can be difficult without characteristic radiographic findings, but the improvement or fluctuations of symptoms may indicate no malignant tumors with a progressive course. When making a differential diagnosis of malignant skull lesions, PICH should be considered.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Gologorsky Y, Shrivastava RK, Panov F, Mascitelli J, Signore AD, Govindaraj S. Primary intraosseous cavernous hemangioma of the clivus: Case report and review of the literature. J Neurol Surg Rep. 2013. 74: 17-22
2. Liu JK, Burger PC, Harnsberger HR, Couldwell WT. Primary intraosseous skull base cavernous hemangioma: Case report. Skull Base. 2003. 13: 219-28
3. Peterson DL, Murk SE, Story JL. Multifocal cavernous hemangioma of the skull: Report of a case and review of the literature. Neurosurgery. 1992. 30: 778-81
4. Serrano L, Archavlis E, Januschek E, Ulrich PT. High risk of cerebrospinal fluid leakage in surgery of a rare primary intraosseous cavernous hemangioma of the clivus showing meningeal infiltration: A case report and review of the literature. Surg Neurol Int. 2015. 6: S117-23
5. Singh U, Kalavakonda C, Venkitachalam S, Patil S, Chinnusamy R. Intraosseous hemangioma of sella: Case report and review of literature. World Neurosurg X. 2019. 3: 100030
6. Sweet C, Silbergleit R, Mehta B. Primary intraosseous hemangioma of the orbit: CT and MR appearance. Am J Neuroradiol. 1997. 18: 379-81
7. Tashiro T, Inoue Y, Nemoto Y, Shakudo M, Mochizuki K, Katsuyama J. Cavernous hemangioma of the clivus: Case report and review of the literature. AJNR Am J Neuroradiol. 1991. 12: 1193-4
8. Vanhoenacker FM, De Praeter G, Kools D, Voormolen M, Parizel PM. Unusual lesion of the clivus: Diagnosis and discussion. Skeletal Radiol. 2011. 40: 243-4
9. Yang Y, Guan J, Ma W, Li Y, Bing X, Zuyuan R. Primary intraosseous cavernous hemangioma in the skull. Medicine (Baltimore). 2016. 95: e3069