- Department of Neurosurgery, Avicenne Military Hospital of Marrakech, Mohammed V University in Rabat, Morocco
- Department of Neurosurgery, State University of New York (SUNY), Upstate Medical University, Syracuse, New York, USA
- Department of Surgery, Avicenne Military Hospital of Marrakech, Mohammed V University in Rabat, Morocco
Correspondence Address:
Ali Akhaddar
Department of Surgery, Avicenne Military Hospital of Marrakech, Mohammed V University in Rabat, Morocco
DOI:10.4103/sni.sni_329_18
Copyright: © 2018 Surgical Neurology International This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.How to cite this article: Ali Akhaddar, Walter Hall, Mohammed Ramraoui, Mehdi Nabil, Ahmed Elkhader. Primary tuberculous psoas abscess as a postpartum complication: Case report and literature review. 28-Nov-2018;9:239
How to cite this URL: Ali Akhaddar, Walter Hall, Mohammed Ramraoui, Mehdi Nabil, Ahmed Elkhader. Primary tuberculous psoas abscess as a postpartum complication: Case report and literature review. 28-Nov-2018;9:239. Available from: http://surgicalneurologyint.com/surgicalint-articles/9095/
Abstract
Background:Primary psoas abscess is an unusual clinical entity rarely encountered in the postpartum period. Only seven cases have been reported to date. Here, we present a woman with a primary psoas abscess caused by Mycobacterium tuberculosis and occurred 2 months following a normal vaginal birth. We highlight the difficulties in the management of this uncommon condition in light of the relevant literature.
Case Description:A 34-year-old woman who was previously healthy was presented at 2 months’ postpartum with important right sciatica and low back pain without fever. Examination of the abdomen revealed tenderness in the right iliac fossa but obstetric/gynecologic and neurologic examinations were normal. The patient had an elevated C-reactive protein level and computed tomography (CT)-scan demonstrated a large psoas abscess on the right side without sacroiliac or spine abnormalities. Initial posterior lumbar percutaneous drainage was useful, but no pathogens were identified. The patient was discharged home with oral antibiotics therapy (amoxicillin/clavulanate and metronidazole). Four weeks later, the follow-up CT-scan showed a re-accumulation of the abscess cavity. Subsequently, the patient underwent a right anterolateral laparotomy with a retroperitoneal approach for abscess drainage. Again, no microorganisms were found. However, diagnosis of tuberculosis was established on histopathologic study. She was successfully treated with antituberculous drugs with a good outcome.
Conclusions:Most primary psoas abscesses present with a delay in diagnosis because of the rarity of this infectious disease, the lack of specific symptoms and signs, and its similarity to many differential diagnoses. When suspected, CT-scan and/or magnetic resonance imaging help in making an accurate diagnosis and facilitate percutaneous or open surgical drainage of the abscess. Correct and fast identification of the microorganisms in addition to appropriate usage of antibiotic regimen improves the outcome.
Keywords: Complication, infection, postpartum, psoas abscess, recurrence, tuberculosis, vaginal delivery
INTRODUCTION
Since the first description of psoas (or iliopsoas) muscle abscess by Herman Mynter in 1881,[
We present a woman who was found to have a primary tuberculous psoas abscess in the postpartum requiring two surgical drainages. We highlight the difficulties in the management of this uncommon condition in light of the relevant literature.
CASE REPORT
After a normal pregnancy and an uneventful vaginal birth of a healthy female infant, a 34-year-old biparous woman presented 2 months’ postpartum with significant right sciatic-like back pain. She had no significant past medical history. The symptoms were initially misdiagnosed as a sciatic neuropathy and she was treated symptomatically at another medical center with a good outcome. On examination, she was afebrile and her vital signs were within normal limits. The examination of the abdomen revealed mild tenderness in the right iliac fossa but her obstetric/gynecologic examination was normal. In addition, the examination of the respiratory, cardiovascular, and central nervous systems revealed no abnormalities.
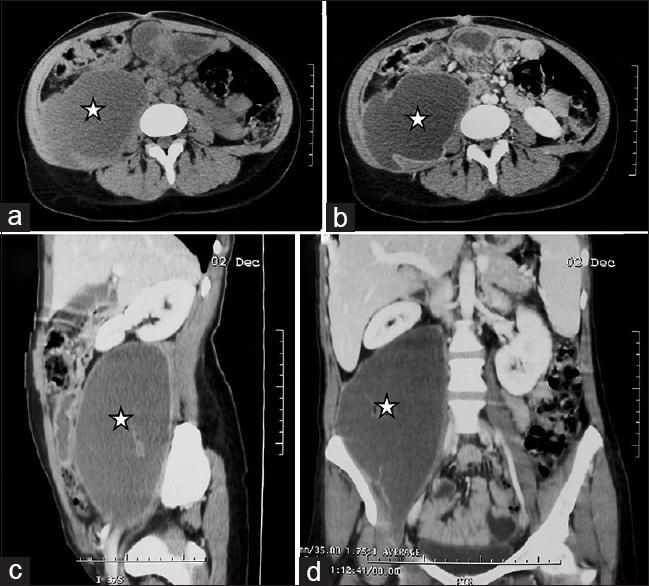
Initial blood tests showed a leukocytosis of 7.3, a hemoglobin of 10.9 g/dL, a raised C-reactive protein (CRP) level of 102 mg/L, and a normal procalcitonin level at 0.316 ng/mL. Serology tests were negative for human immunodeficiency virus (HIV-1 and HIV-2). Spinal lumbar and abdominal computed tomography scans (CT-scan) surprisingly showed a large right psoas abscess measuring 18 × 10 × 8 cm (a volume of about 720 mL) [
Figure 1
Axial abdominal and pelvic CT-scan before (a) and after (b) contrast injection. Sagittal (c) and coronal (d) abdominal reconstructions following contrast administration. There was a large right psoas muscle abscess (stars) displacing the right kidney upward. Note the presence of ring enhancement
Posterior lumbar percutaneous drainage of the abscess was performed. Approximately, 570 mL of purulent fluid was obtained and a drain was left in place [
Figure 2
Operative view demonstrating posterior percutaneous drainage of the purulent collection above the right iliac crest (a). Follow-up abdominal CT scan 2 days after drainage of the abscess. Note the placement of the percutaneous drain (arrows) and the near complete resolution of the retroperitoneal collection (b). A follow-up axial abdominal CT scan with contrast injection 6 months postoperatively showing the absence of recurrent abscess (c)
Four weeks later, there was no recurrence of neurological symptoms except for mild low back pain. However, a repeat CT-scan of the abdomen and the pelvis showed a re-accumulation of the right psoas collection measuring approximately 400 mL. Subsequently, she underwent a right anterolateral minilaparotomy with a retroperitoneal approach for open abscess drainage. Again, no microorganisms were identified on culture. However, a diagnosis of tuberculosis was established after identification of epitheloid giant cells and caseous necrosis on the fibrotic abscess wall biopsy. The patient made an uneventful recovery and was discharged home on postoperative day 5. A follow-up CT-scan showed no re-accumulation of the abscess. She was successfully treated with antituberculous chemotherapy for 6 months with good clinical and radiological outcomes [
DISCUSSION
In obstetrical practice, postpartum infection usually involves the uterus and adjacent pelvic structures presenting with typical and predictable symptoms and signs. However, musculoskeletal and focal neurological infections can rarely be seen in the postpartum period.[
The psoas muscle is in near proximity to anatomical structures such as the thoraco-lumbo-sacral spine, iliac lymph nodes, abdominal aorta, kidneys, ureters, pancreas, jejunum, sigmoid colon, and appendix. For this reason, infections of intra-abdominal organs can spread to the iliopsoas muscle. The important blood supply of this muscle is supposed to predispose it to hematogenous spread from occult sites of infection.[
The clinical presentation of a psoas abscess is often variable and nonspecific.[
Psoas muscle abscess is often initially misdiagnosed as muscle strain, acute myositis, contusion, hematoma, septic pelvic thrombophlebitis, perinephric abscess, pyelonephritis, acute appendicitis, pelvic or spinal osteomyelitis, trochanteric bursitis, sacroiliitis, cellulitis, or necrotizing fasciitis. In addition, tumors arising from the structures within the pelvis or lumbar area may mimic a psoas abscess.[
Laboratory tests reveal nonspecific signs of inflammation: marked elevation of the erythrocyte sedimentation rate and CRP levels, an increased peripheral white blood cell count, and occasionally anemia. Blood cultures may be positive for a particular organism causing the abscess. HIV test is recommended, as this is a cause for immunosuppression predisposing to the development of PPA. In endemic areas, every effort should be made to ensure that the mycobacterium is excluded by acid-fast staining and culture techniques.[
CT-scan and magnetic resonance imaging (MRI) are the best radiological modalities for diagnosis because of the low sensitivity and specificity of ultrasound.[
S. aureus is the most frequently identified pathogen in patients with PPA (about 90% of cases). Secondary psoas abscess is usually caused by enteric bacteria such as Streptococcus species (4.9%) and Escherichia coli (2.8%).[
The pathogenesis of PPA in the postpartum period remains unclear. It has been suggested that trauma during delivery may cause an asymptomatic hematoma within the psoas muscle which can become infected.[
Treatment should be started as soon as a clinical diagnosis of psoas abscess is confirmed. The administration of appropriate antibiotics and prompt surgical drainage are necessary when a large suppurative collection is found. Antibiotic coverage should include staphylococcal species and enteric organisms. Antimicrobial adjustments should be based on the report of the abscess fluid culture and sensitivity testing.[
If treated early and adequately, most patients with PPA will be cured without further complications or recurrent infection.[
CONCLUSION
PPA is an uncommon but serious clinical entity rarely encountered in neurosurgery, obstetrics, and gynecology. This clinical problem may occur as a postpartum complication but a delay in diagnosis is common because of its insidious development and lack of specific (localizing) symptoms and signs. When PPA is suspected, the CT-scan and MRI help in making an accurate diagnosis and will facilitate the percutaneous or open drainage of the purulent collection. Correct identification of the causative microorganisms and prompt and appropriate usage of antimicrobial therapy can result in improved clinical outcome and reduce neurological morbidity. Therefore, psoas abscess must be considered in the differential diagnosis for patients with low back and leg pain even in the absence of fever.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Akhaddar A.editors. Spinal tuberculosis. Atlas of Infections in Neurosurgery and Spinal surgery. Switzerland: Springer International Publishing; 2017. p. 249-275
2. Akhaddar A, Elmostarchid B, Boucetta M. Primary subdural empyema after spontaneous vaginal delivery. Surg Infect (Larchmt). 2009. 10: 363-4
3. Akhaddar A, Mahi M, Harket A, Elmostarchid B, Belhachemi A, Elasri A. Brainstem tuberculoma in a postpartum patient. J Neuroradiol. 2007. 34: 345-6
4. Aydogmus S, Sen Selim H, Eris S, Kelekci S. A rare complication of caesarean delivery: Iliopsoas abscess. Acta Obstet Gynecol Scand. 2014. 93: 1071-2
5. Bhattacharya R, Gobrial H, Barrington JW, Isaacs J. Psoas abscess after uncomplicated vaginal delivery: An unusual case. J Obstet Gynaecol. 2008. 28: 544-6
6. Biswas R, Baghel V, Shanker S. A gibbus in puerperium. BMJ Case Rep. 2008. 2008: bcr0620080154-
7. Chawla K, D’Souza A, N SB, Mukhopadhayay C. Primary tubercular psoas abscess: A rare presentation. J Infect Dev Ctries. 2012. 6: 86-8
8. Desandre AR, Cottone FJ, Evers ML. Iliopsoas abscess: Etiology, diagnosis, and treatment. Am Surg. 1995. 61: 1087-91
9. Dinc H, Onder C, Turhan AU, Sari A, Aydin A, Yuluğ G. Percutaneous drainage of tuberculous and nontuberculous psoas abscesses. Eur J Radiol. 1996. 23: 130-4
10. Garagiola DM, Tarver RD, Gibson L, Rogers RE, Wass JL. Anatomic changes in the pelvis after uncomplicated vaginal delivery: A CT study on 14 women. Am J Roentgenol. 1989. 153: 1239-41
11. Garner JP, Meiring PD, Ravi K, Gupta R. Psoas abscess-not as rare as we think?. Colorectal Dis. 2007. 9: 269-74
12. Kumar S, Malhotra N, Chanana C, Lal S. Psoas abscess in obstetrics. Arch Gynecol Obstet. 2009. 279: 247-9
13. Kwan A, Bhanshaly A, Wright C. Iliopsoas abscess: An unusual cause of postpartum sepsis. Obstet Med. 2009. 2: 30-1
14. Lai YC, Lin PC, Wang WS, Lai JI. An update on Psoas Muscle Abscess: An 8-Year experience and review of literature. Int J Gerontol. 2011. 5: 75-9
15. Lau SK, Woo PC, Yim TC, To AP, Yuen KY. Molecular characterization of a strain of group a streptococcus isolated from a patient with a psoas abscess. J Clin Microbiol. 2003. 41: 4888-91
16. Liu XQ, Li FC, Wang JW, Wang S. Postpartum septic sacroiliitis misdiagnosed as sciatic neuropathy. Am J Med Sci. 2010. 339: 292-5
17. Mallick IH, Thoufeeq MH, Rajendran TP. Iliopsoas abscesses. Postgrad Med J. 2004. 80: 459-62
18. Mynter H. Acute psoitis. Buffalo Med Surg J. 1881. 21: 202-10
19. Patil A, Gatongi DK, Haque L, Mires G. Primary psoas abscess following spontaneous vaginal delivery. J Obstet Gynaecol. 2006. 26: 565-9
20. Ricci MA, Rose FB, Meyer KK. Pyogenic psoas abscess: Worldwide variations in etiology. World J Surg. 1986. 10: 834-43
21. Saylam K, Anaf V, Kirkpatrick C. Successful medical management of multifocal psoas abscess following cesarean section: Report of a case and review of the literature. Eur J Obstet Gynecol Reprod Biol. 2002. 102: 211-4
22. Scheepers NJ, van Bommel PF, Bleker OP. Psoas abscess related to spontaneous abortion, intra-uterine contraceptive device and curettage. Acta Obstet Gynecol Scand. 1993. 72: 223-4
23. Shah PN, Rane VA, Moolgaoker AS. Retroperitoneal abscess complicating a normal delivery. Br J Obstet Gynaecol. 1992. 99: 160-1
24. Shahabi S, Klein JP, Rinaudo PF. Primary psoas abscess complicating a normal vaginal delivery. Obstet Gynecol. 2002. 99: 906-9
25. Shinohara T, Kagawa K, Okano Y, Sawada T, Kobayashi T, Takikawa M. Disseminated tuberculosis after pregnancy progressed to paradoxical response to the treatment: Report of two cases. BMC Infect Dis. 2016. 16: 284-
26. Suzaki A, Takazoe M. Successful medical management of multilocular psoas abscess in a pregnant woman with Crohn's disease: A case report. J Nihon Univ Med Ass. 2011. 70: 50-3
27. Thomas A, Albert AS, Bhat S, Sunil KR. Primary psoas abscess--diagnostic and therapeutic considerations. Br J Urol. 1996. 78: 358-60
28. Wong JG. The psoas signs. Well-described but often forgotten physical examination findings of iliopsoas inflammation. N C Med J. 1993. 54: 598-600
29. Young OM, Werner E, Sfakianaki AK. Primary psoas muscle abscess after an uncomplicated spontaneous vaginal delivery. Obstet Gynecol. 2010. 116S2: 477-9