- Department of Surgery, Section of Neurosurgery, University of Puerto Rico, San Juan, Puerto Rico
Correspondence Address:
Orlando De Jesus, Department of Surgery, Section of Neurosurgery, University of Puerto Rico, San Juan, Puerto Rico.
DOI:10.25259/SNI_1077_2024
Copyright: © 2025 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Christian I. Rios-Vicil, Orlando De Jesus. Prostate adenocarcinoma dural metastasis mimicking a subacute subdural hematoma. 21-Feb-2025;16:60
How to cite this URL: Christian I. Rios-Vicil, Orlando De Jesus. Prostate adenocarcinoma dural metastasis mimicking a subacute subdural hematoma. 21-Feb-2025;16:60. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=13392
Abstract
BackgroundPatients with malignancies that have a propensity to develop dural metastasis can present a dural infiltration mimicking a subdural hematoma. Dural metastases originating from prostate cancer mimicking a subdural hematoma are rare.
Case DescriptionThe authors describe the case of a 66-year-old man with a history of prostate adenocarcinoma with vertebral metastases who complained of headaches, weakness, anorexia, and dizziness for 1 month. A head computed tomography scan without contrast demonstrated a right pan-hemispheric subdural collection, which was reported to be a subacute subdural hematoma. Due to the patient’s history of prostate carcinoma, brain magnetic resonance imaging (MRI) with and without gadolinium was requested before the surgery, which showed substantial enhancement of the subdural collection, suggesting a tumoral collection. Based on the MRI findings, an open biopsy was performed, revealing extensive bone infiltration and a thickened dura with a large subdural tumoral component suggestive of disseminated pachymeningeal carcinomatosis. No hematoma was identified.
ConclusionThis case report demonstrated how metastatic lesions can mimic subdural hematomas. This disease carries a poor prognosis. Diagnosing and managing this rare entity warrants high suspicion to guide the patient and the family members in decision-making.
Keywords: Dural metastasis, Leptomeningeal carcinomatosis, Pachymeningeal carcinomatosis, Prostate adenocarcinoma, Subdural hematoma
INTRODUCTION
Patients with malignancies that tend to develop dural metastasis could present pachymeningeal carcinomatosis. The most frequent primary cancers associated with intracranial dural metastasis are breast, prostate, and lung.[
CASE PRESENTATION
A 66-year-old man with a history of prostate adenocarcinoma diagnosed 13 years before and vertebral metastases 1 year ago complained of headaches, weakness, anorexia, and dizziness for 1 month. The patient and family members denied any recent trauma. On examination, he was alert and oriented in person and place. He had no motor or sensory deficits. The head CT scan without contrast showed a slight hyperdense right pan-hemispheric subdural collection, causing an 8 mm shift of midline structures [
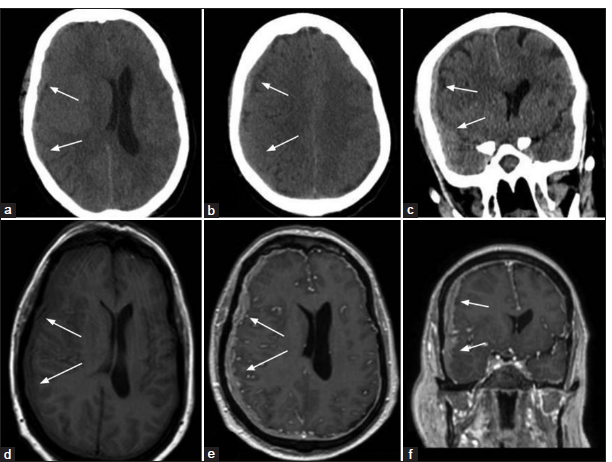
Figure 1:
Head computed tomography (a and b) without contrast axial images and (c) coronal image show the slight hyperdense pan-hemispheric subdural collection on the right side (white arrows), causing an 8-mm shift of midline structures. Brain magnetic resonance imaging (MRI) (d) axial T1 image without gadolinium shows a slight hypointense subdural collection (white arrows); (e) brain MRI axial T1 image and (f) coronal T1 image with gadolinium show substantial enhancement of the subdural collection (white arrows) and the shift of midline structures.
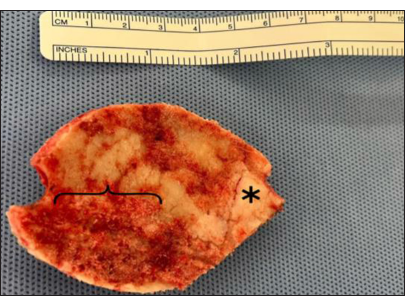
We assessed that the collection probably represented pachymeningeal carcinomatosis; therefore, a craniotomy with tumor biopsy was recommended. Due to severe thrombocytopenia of 36,000 per microliter of blood, a transfusion of platelets was given before the operation, increasing the platelet count to 96,000. A frontotemporal craniotomy was performed. The craniotomy bone was grossly infiltrated with tumoral cells and was discarded [
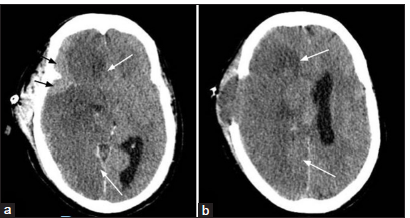
Figure 3:
Head computed tomography (a and b) without contrast axial images 5 days postoperative showing a complete acute ischemic stroke in the distribution of the right middle cerebral artery (white arrows). Black arrows indicate the subdural tumor collection at the sphenoid wing/Sylvian fissure region.
DISCUSSION
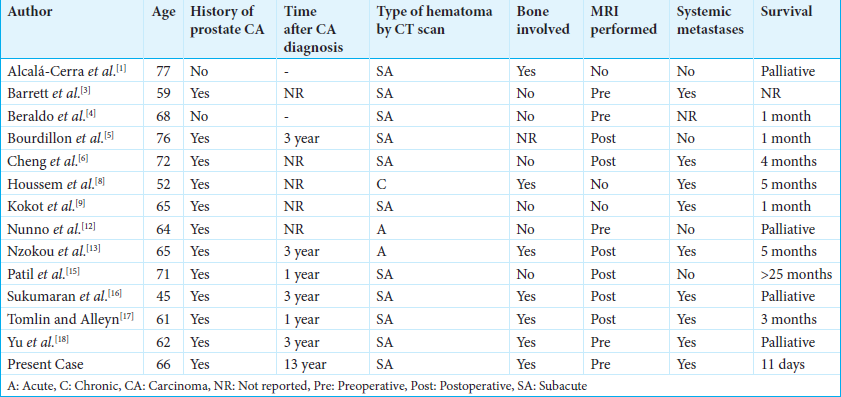
Case reports have documented subdural hematomas containing prostate tumor nodules within the subdural space.[
A brain MRI with gadolinium can identify pachymeningeal carcinomatosis substantially better, allowing finer delineation of the enhancing extra-axial collection.[
CONCLUSION
Metastatic subdural collections can mimic a subdural hematoma. The management of the patient should not be based only on imaging studies. Patients with metastatic dural infiltration and pachymeningeal carcinomatosis carry a poor prognosis due to their advanced primary disease and the infiltration of the brain and pachymeninges. These metastatic collections warrant high diagnostic suspicion to guide patients and their family members in clinical decision-making.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript, and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Alcalá-Cerra G, Gutiérrez-Paternina JJ, Niño-Hernández LM, Sabogal-Barrios R, Moscote-Salazar LR, Suárez-Jaramillo K. Metástasis dural como manifestación inicial de cáncer de próstata [Dural metastasis as the first manifestation of prostate cancer]. An Sist Sanit Navar. 2011. 34: 513-7
2. Aleksić V, Joković M, Ilić R, Bogosavljević V, Đurović B. Dural metastasis of prostate carcinoma misdiagnosed as a bilateral subdural hematoma: A case report. Neurocirugia (Astur: Engl Ed). 2020. 2020: S1130-1473 (20)30108-1
3. Barrett C, Rodrigues D, Bradey N, Strachan R. Intracranial metastasis masquerading as acute subdural haematoma. Br J Neurosurg. 2008. 22: 444-6
4. Beraldo RF, Gatto LA, Golff IF, Alchieri TG, Pereira MC, Demartini Z. Dural metastasis of prostate cancer mimicking chronic subdural hematoma. Neurol India. 2024. 72: 209-10
5. Bourdillon P, Apra C, Cornu P, Chauvet D. An unexpected subdural collection: Story of a prostatic metastasis. Clin Genitourin Cancer. 2016. 14: e405-7
6. Cheng YK, Wang TC, Yang JT, Lee MH, Su CH. Dural metastasis from prostatic adenocarcinoma mimicking chronic subdural hematoma. J Clin Neurosci. 2009. 16: 1084-6
7. Dearborn JL, Urrutia VC, Zeiler SR. Stroke and cancer-A complicated relationship. J Neurol Transl Neurosci. 2014. 2: 1039
8. Houssem A, Helene C, Francois P, Salvatore C. “The subdural collection” a great simulator: Case report and literature review. Asian J Neurosurg. 2018. 13: 851-3
9. Kokot K, Dzierżanowski J, Krakowiak M, Fercho J, Yuser R, Kosel L. Dural metastasis of prostate carcinoma mimicking intracranial hematoma: A case report and literature review. J Surg Case Rep. 2024. 2024: rjae014
10. Laigle-Donadey F, Taillibert S, Mokhtari K, Hildebrand J, Delattre JY. Dural metastases. J Neurooncol. 2005. 75: 57-61
11. Nayak L, Abrey LE, Iwamoto FM. Intracranial dural metastases. Cancer. 2009. 115: 1947-53
12. Nunno A, Johnson MD, Wu G, Li YM. Metastatic prostate cancer mimicking a subdural hematoma: A case report and literature review. J Clin Neurosci. 2018. 55: 109-12
13. Nzokou A, Magro E, Guilbert F, Fournier JY, Bojanowski MW. Subdural metastasis of prostate cancer. J Neurol Surg Rep. 2015. 76: e123-7
14. O’Meara C, Mahasneh T, Wilson P, I’Ons B, Alkhawaja D. Dural prostate metastasis resembling a chronic subdural haematoma. J Surg Case Rep. 2012. 2012: 7
15. Patil S, Veron A, Hosseini P, Bates R, Brown B, Guthikonda B. Metastatic prostate cancer mimicking chronic subdural hematoma: A case report and review of the literature. J La State Med Soc. 2010. 162: 203-5
16. Sukumaran M, Mao Q, Cantrell DR, Jahromi BS, Potts MB. Holohemispheric prostate carcinoma dural metastasis mimicking subdural hematoma: Case report and review of the literature. J Neurol Surg Rep. 2022. 83: e23-8
17. Tomlin JM, Alleyne CH. Transdural metastasis from adenocarcinoma of the prostate mimicking subdural hematoma: Case report. Surg Neurol. 2002. 58: 329-31 discussion 331
18. Yu WL, Sitt CM, Cheung TC. Dural metastases from prostate cancer mimicking acute sub-dural hematoma. Emerg Radiol. 2012. 19: 549-52