- Department of Orthopaedics, Sagar Hospitals, Bengaluru, Karnataka, India
- Department of Neurosurgery, Sagar Hospitals, Bengaluru, Karnataka, India
Correspondence Address:
Narottam Das, Department of Orthopaedics, Sagar Hospitals, Bengaluru, Karnataka, India.
DOI:10.25259/SNI_115_2025
Copyright: © 2025 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Narottam Das1, Pranathi Chandana2, Manmeet Singh Chhabra2, Praveen L. Basanagoudar1. Quadrangular space schwannoma affecting the axillary nerve. 02-May-2025;16:164
How to cite this URL: Narottam Das1, Pranathi Chandana2, Manmeet Singh Chhabra2, Praveen L. Basanagoudar1. Quadrangular space schwannoma affecting the axillary nerve. 02-May-2025;16:164. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=13532
Abstract
BackgroundSchwannomas are benign neural tumors originating primarily from Schwann cells associated with cranial and spinal nerves, which are a well-known medical entity. However, their occurrence in the extremities, particularly those involving the axillary nerve, is a rare phenomenon with limited literature documentation.
Case DescriptionWe present a case of a 29-year-old male who complained of painful swelling in the posterior shoulder region. Further diagnostic investigations, including ultrasound and magnetic resonance imaging, unveiled the presence of a subdeltoid tumor situated in the quadrangular space, originating from the axillary nerve.
ConclusionThis case report documents our experience in successfully surgically excising this rare benign axillary nerve tumor using an extracapsular approach. Intraoperative neural monitoring was employed to safeguard neural integrity. Our case highlights the importance of a high degree of suspicion, early diagnosis, and meticulous surgical techniques in managing such uncommon nerve sheath tumors while preserving neurological function.
Keywords: Neuro-monitoring, Schwannoma, Tumor
INTRODUCTION
Schwannomas are relatively uncommon encapsulated neoplasms that typically occur in the brain and spine. However, they can also develop less frequently from peripheral nerves within the appendicular skeleton.[
Intermuscular schwannomas are even rarer tumors, characterized by slow growth and presenting as soft-tissue masses. In this report, we share our experience of managing a case of intermuscular axillary nerve schwannoma. We detail its clinical presentation, diagnostic radiological characteristics, the use of intraoperative neuro-monitoring to safeguard axillary nerve function, and successful surgical management.
CASE PRESENTATION
A 29-year-old gentleman initially sought medical attention due to right shoulder pain persisting for 3 days following heavy weightlifting. On clinical examination, the patient exhibited painful shoulder rotation and limited abduction. X-rays of the right shoulder in the anteroposterior and lateral views were normal. The initial suspicion was a right rotator cuff injury, and the patient was managed conservatively with pain medications and an arm pouch application for a week. A magnetic resonance imaging (MRI) of the right shoulder was advised only if pain persisted despite supportive management. Despite these initial interventions, the patient continued to experience persistent pain.
He returned with complaints of swelling on the posterior aspect of the right shoulder, along with progressive right shoulder pain. He also reported weakness in the right shoulder, manifesting as difficulty in reaching his back with his right arm. Clinical examination revealed a partially mobile, oval, firm, and tender lump measuring 4 cm × 2 cm at the posteroinferior border of the deltoid muscle, with no secondary skin changes or neural deficits [
The patient was evaluated with an MRI shoulder, which showed a well-circumscribed lesion measuring approximately 2.13 × 3.48 × 3.38 (A × H × T) cm in diameters across the intermuscular plane, superficial to teres minor, infraspinatus, and the deltoid muscle. The lesion was hypointense on T1-weighted and heterogenous intensity on fluid-attenuated inversion recovery sequences, with homogenously enhancing contrast.
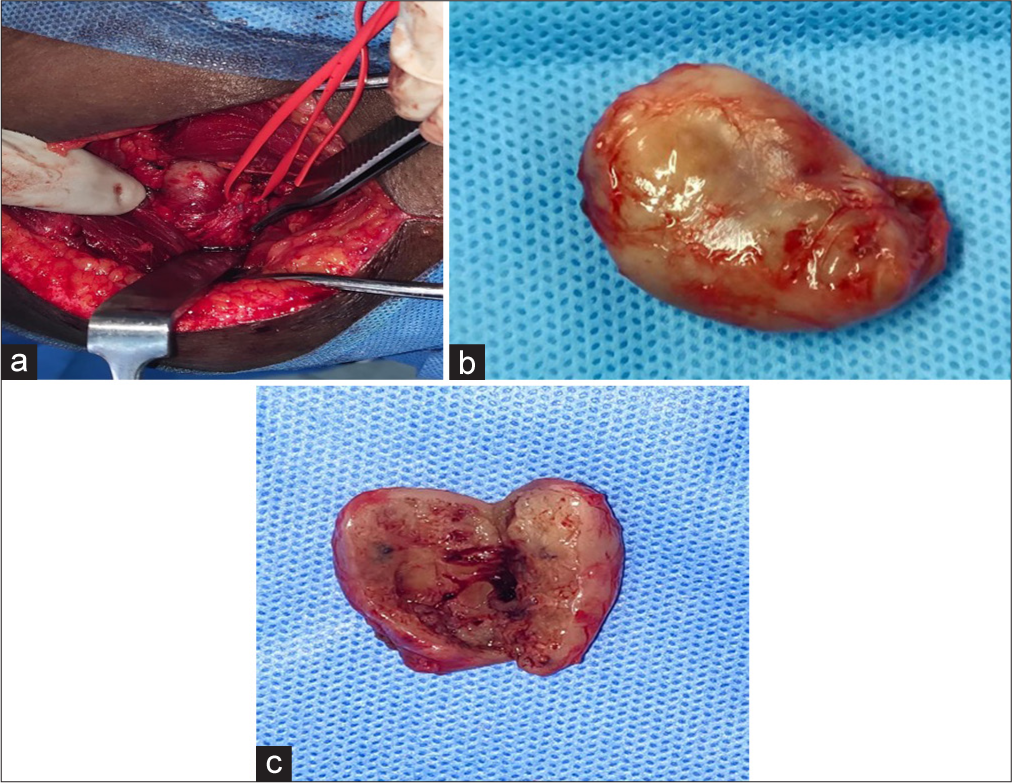
The patient underwent a complete en bloc excision of the tumor using an extracapsular dissection technique, employing a posterior shoulder approach under general anesthesia. The patient was positioned in the left lateral position, and the margins of the swelling were marked. Intraoperative nerve monitoring probes were placed within the deltoid muscle, away from the surgical dissection plane, and connected to the neuromonitoring device (NIM ECLIPSE). The surgical dissection carried along the avascular plane situated between the posterior border of the deltoid muscle anteriorly and the lateral head of the triceps muscle posteriorly. The quadrangular space was exposed, and the tumor was seen arising from the axillary nerve below the posterior margin of the deltoid muscle. The tumor capsule was meticulously dissected from the axillary nerve, employing an operative neuro-microscope, ensuring complete tumor excision while safeguarding the nerve through continuous nerve action potential monitoring. Intraoperative findings revealed a firm, well-encapsulated tumor originating from the right axillary nerve.
A gross histopathological examination of the tumor revealed a gray-white tumor measuring 3 cm × 2 cm × 2 cm. The tumor was encapsulated, with the cut section displaying tiny cystic areas with hemorrhages. Microscopic examination of sections from the tumor demonstrated a benign spindle cell tumor composed of fascicles of spindle cells arranged in both hypocellular (Antoni A) and hypercellular areas (Antoni B). The spindle cells featured tapered bipolar nuclei, while areas of hyalinization, edema, and thick-walled blood vessels were also observed. No atypia, necrosis, or mitosis were noted, consistent with a diagnosis of Schwannoma [
Figure 2:
(a) Intraoperative photo – an axillary incision was made, followed by a meticulous dissection to access the tumor. (b) Excised tumor specimen, measuring approximately 4 cm× 4 cm. (c) A gross pathology examination of the excised tumor revealed it to be split in half, displaying a cystic component
DISCUSSION
Schwannomas arising in the quadrangular space represent a rare entity causing posterior shoulder pain. Due to their infrequent occurrence and deep-seated location, they present substantial challenges in terms of both diagnosis and treatment.[
In the case presented here, the initial suspicion was a partial rotator cuff injury. However, further evaluation led to the diagnosis of an axillary nerve schwannoma, which was found to exert significant compression on the right axillary nerve, closely mimicking quadrilateral space syndrome. Previous literature has documented mass lesions as potential causes of quadrilateral space syndrome, including ganglia, glenoid labral cysts, osteochondromas, bone spurs, and fracture hematomas.[
Early diagnosis of schwannomas can be challenging due to their slow growth. MRI is the preferred diagnostic modality, offering critical information about tumor size, deep-seated location, and its anatomical relationship with adjacent structures. On MRI, schwannomas typically appear as distinct, homogeneously enhancing lesions [
Figure 3:
(a and b) Magnetic resonance imaging of right shoulder showing a circumscribed irregularly ovoid area of heterogenous signals, measuring approximately 2.13 × 3.48 × 3.38 (A × H × T) cm in diameters across the intermuscular plane, superficial to teres minor, infraspinatus muscles, and the deltoid muscle.
Differentiating between schwannomas and neurofibromas is crucial. Schwannomas are typically encapsulated and eccentrically positioned within the nerve, whereas neurofibromas lack these characteristics.
While imaging studies are valuable, they cannot provide a definitive diagnosis, making biopsy a more conclusive approach. Fine-needle aspiration is an option, although it may not delineate tissue architecture patterns.[
The primary treatment of choice for Schwannomas is surgical excision of the tumor while minimizing the risk of neurological deficits. Early surgical intervention is recommended to prevent an increase in tumor size, which could heighten the risk of post-surgical neurological deficits. The two main surgical techniques for treating Schwannomas are extracapsular and intracapsular enucleation, both of which have demonstrated effectiveness in various studies. In our case, the patient underwent complete tumor excision en bloc with the extracapsular dissection technique through a posterior approach. Although intracapsular enucleation has been favored in some studies,[
CONCLUSION
In this case study, we shared our experience with the extracapsular surgical excision of a rare benign tumor affecting the axillary nerve. This case underscores the importance of a multidisciplinary approach, accurate diagnosis, and meticulous surgical technique in effectively treating such uncommon nerve sheath tumors while preserving neurological function.
Ethical approval
The Institutional Review Board has waived the ethical approval for this study.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Basso E, Maistrello L, Delfinis CP, Ferraresi S. Axillary nerve schwannoma at the quadrilateral space: Report of a case. Acta Sci Clin Case Rep. 2020. 1: 14-6
2. Boutsen Y, De Coene B, Hanson P, Deltombe T, Gilliard C, Esselinckx W. Axillary schwannoma masquerading as cervical radiculopathy. Clin Rheumatol. 1999. 18: 174-6
3. Colonna MR, Costa AL, Mastrojeni C, Rizzo V, Nirta G, Angileri FF. Giant sacral schwannoma excised under intraoperative neuromonitoring in an elderly patient: Case report. J Surg Case Rep. 2021. 2021: rjab460
4. Date R, Muramatsu K, Ihara K, Taguchi T. Advantages of intra-capsular micro-enucleation of schwannoma arising from extremities. Acta Neurochir (Wien). 2012. 154: 173-8
5. Dubuisson A, Reuter G, Kaschten B, Martin D, Racaru T, Steinmetz M. Management of benign nerve sheath tumors of the brachial plexus: Relevant diagnostic and surgical features. About a series of 17 patients (19 tumors) and review of the literature. Acta Neurol Belg. 2021. 121: 125-31
6. El Andaloussi Y, Abkari I, Bleton R. Schwannome du nerf axillaire (à propos d’un cas) [Axillary nerve schwannoma (case report)]. Chir Main. 2008. 27: 232-4
7. Hong SW, Cho WY, Kim JO, Chun CG, Shim KY, Bok GH. Gastric schwannoma diagnosed by endoscopic ultrasonography-guided trucut biopsy. Clin Endosc. 2013. 46: 284-7
8. Hung CY, Chang KV, Chen PT, Ho YT, Han DS, Chen WS. Sonoelastography for the evaluation of an axillary schwannoma in a case of quadrilateral space syndrome. Clin Imaging. 2014. 38: 360-3
9. Kumar PA, Islary B, Ramachandra R, Naik T. Axillary nerve schwannoma: A rare case report. Asian J Neurosurg. 2017. 12: 787-9
10. Manohar N, Balasubramaniam A, Kumar MS, Rao K, Srinivas D, Chakrabarti D. Intraoperative neuromonitoring during sciatic nerve schwanomma excision: Utility of evoked potentials. J Neurosurg Anesthesiol. 2019. 31: 261-2
11. Moond V, Diwaker P, Golamari R, Jain R. Intramuscular ancient schwannoma of the axillary nerve. BMJ Case Rep. 2021. 14: e239445
12. Nasrollah N, Trimboli P, Bianchi D, Taccogna S. Neck schwannoma diagnosed by core needle biopsy: A case report. J Ultrasound. 2015. 18: 407-10
13. Perez-Roman RJ, Shelby Burks S, Debs L, Cajigas I, Levi AD. The risk of peripheral nerve tumor biopsy in suspected benign etiologies. Neurosurgery. 2020. 86: E326-32
14. Salunke AA, Chen Y, Tan JH, Chen X, Foo TL, Gartner LE. Intramuscular schwannoma: Clinical and magnetic resonance imaging features. Singapore Med J. 2015. 56: 555-7
15. Sengul D, Sengul I, Karinoglu U, Apan OC, Oksuz H, Apan A. A rare case of axillary Schwannoma. Ann Ital Chir. 2019. 8: S2239253X19030470
16. Tatar IG, Yilmaz KB, Arikok A, Bayar B, Akinci M, Balas S. Cystic schwannoma of the axillary region: Imaging findings of a rare disease. Case report. Med Ultrason. 2015. 17: 126-8