- Jacobs School of Medicine and Biomedical Sciences, University at Buffalo, Buffalo, New York, United States
- Department of Surgery, Buffalo General Medical Center, Buffalo, New York, United States
- Department of Neurosurgery, Longstreet Clinic, Gainesville, New York, United States
- Department of Neurosurgery, John R. Oishei Children’s Hospital, Buffalo, New York, United States
- Department of Neurosurgery, University at Buffalo Jacobs School of Medicine and Biomedical Sciences, Buffalo, New York, United States
Correspondence Address:
Renée M. Reynolds, Department of Neurosurgery, University at Buffalo Jacobs School of Medicine and Biomedical Sciences, Buffalo, New York, United States.
DOI:10.25259/SNI_187_2025
Copyright: © 2025 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Megan D. Malueg1, Hayden E. Greene2, Betsy Grunch3, Alexandra R. Spath1, Renée M. Reynolds4,5. Radiation safety practices in neurosurgery: Exploring education gaps and concerns among physicians and trainees. 30-May-2025;16:207
How to cite this URL: Megan D. Malueg1, Hayden E. Greene2, Betsy Grunch3, Alexandra R. Spath1, Renée M. Reynolds4,5. Radiation safety practices in neurosurgery: Exploring education gaps and concerns among physicians and trainees. 30-May-2025;16:207. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=13596
Abstract
Background: In this study, we investigated the adequacy of radiation safety education for neurosurgical trainees and physicians, focusing on their perceptions and concerns.
Methods: A survey was distributed through the social media platforms LinkedIn, X (formerly Twitter), and Instagram, as well as through email to individuals listed on the “2023 Neurosurgery Residency Program Information and Interview Dates” document available on the Society of Neurological Surgeons website. Surveys were distributed on December 5, 2023, January 18, 2024, and February 8, 2024. The collection of responses ceased on February 26, 2024. Data collected encompassed respondent demographics, practice and training characteristics, radiation safety knowledge and practice, and radiation exposure concerns.
Results: Of the 48 total responses received, 25 (women, 22) received from neurosurgical residents, fellows, or attending physicians were analyzed. Concerns about health, fertility, and inadequate radiation safety education were evident. Notably, 68% expressed concerns about the impact of radiation exposure on fertility and 52% on pregnancy, with 60% reporting concerns about health risks of radiation exposure. In addition, 68% found radiation safety education provided throughout their neurosurgical career unsatisfactory, with 44% feeling inadequately informed. Considerable knowledge gaps were demonstrated on assessment.
Conclusion: This study reveals prevalent concerns and knowledge gaps in radiation safety education among a geographically diverse group of practicing and training neurosurgeons. Addressing these concerns requires targeted interventions to improve radiation safety education and alleviate apprehensions among neurosurgical trainees and physicians.
Keywords: Intraoperative imaging, Minimally invasive surgical procedures, Neurosurgery, Neurosurgical education, Radiation exposure
INTRODUCTION
Minimally invasive techniques have become the standard of care for many procedures in the field of neurosurgery, increasing the use of intraoperative imaging techniques. This increasing prevalence has been observed to directly impact radiation safety practices and workplace safety for both training and practicing neurosurgeons.[
Recent surveys in the field of orthopedic surgery have highlighted an apparent deficit in both radiation safety knowledge and safety training, with trainees and attending physicians demonstrating consistently low levels of knowledge on survey assessments and only 20% of respondents reporting having received any form of training regarding radiation safety standards and practices.[
Although the impact of this over-exposure may not be seen for years, it is vital that surgeons and trainees recognize and mitigate the risks posed by exposure to intraoperative ionizing radiation. These risks are directly related to the degree and duration of exposure, with no threshold dose, and the probability of negative outcomes is proportional to the level of radiation dose.[
In this study, we sought to characterize better the receipt of training regarding radiation safety and the utilization of suggested practices and PPE. We additionally sought to quantify and characterize the level of concern among neurosurgical trainees and physicians related to regular exposure to ionizing radiation. Although several factors are known to influence rates of cumulative exposure throughout a neurosurgical career, we sought to identify concerns and patterns relevant to most neurosurgical trainees and attending physicians despite differences in location of practice or experience level.
MATERIALS AND METHODS
Research ethics and data availability
In line with the policies set forth for use by Institutional Review Boards of the United States (US) starting January 20, 2019, the methods of this study meet the criteria to qualify for Exemption 45 CFR 46.104(d)(2).[
Data collection
Data were collected through the distribution of an anonymous survey using Google Forms. The survey was distributed through various mechanisms, including through email, to all contacts for 126 residency programs listed on the “2023 Neurosurgery Residency Program Information and Interview Dates” document (
Data were collected on variables related to respondent demographics, practice and training characteristics, radiation safety practices and knowledge, and exposure concerns. Specific variables related to respondent demographics included current title, current practice or training location (country and state or territory, if applicable), age group, and number of years in and setting of practice or training. Nine multiple-choice questions were used to assess levels of respondents’ radiation safety knowledge [
Data collected pertaining to respondents’ personal experiences and practice characteristics included questions regarding how many days per week respondents operate, the average number of operations performed per day, and the percentage of operations in which respondents use intraoperative X-ray radiography. Variables related to personal radiation safety practices included the following: how often and what kinds of specific radiation PPE are used, the source of the PPE, how often the provided PPE fit the respondents correctly if dosimeter badges were used during operations, location of dosimeter badge placement, respondents’ distance from the X-ray device during fluoroscopy use, and all safety guidelines routinely followed. For questions regarding safety guidelines routinely followed and forms of radiation PPE normally used, respondents were allowed to select as many answers as applied to their practice.
Questions involving respondents’ educational self-assessment included the following: feelings of adequate knowledge of radiation safety, provision of education about radiation exposure at any point throughout neurosurgical career, the primary format of radiation safety education, rating of satisfaction with radiation safety education received, and knowledge of the general dose of radiation received with standard anteroposterior imaging specific to their typically performed procedures. Finally, respondents’ concerns and health outcomes were assessed with questions regarding any worry about the risks of radiation to health, pregnancy, or fertility, history or diagnosis of any form of cancer, specifically breast, testicular, or thyroid cancers.
Statistical analysis
All data analyses were performed with Excel software (Microsoft Corporation, Redmond, Washington, USA). Data used for analyses were limited to those provided by respondents who identified themselves as neurosurgical residents, fellows, or attending physicians. For all questions, the number (n) and percentage of respondents who chose each response were calculated. Responses to the nine questions in the radiation safety knowledge assessment were evaluated for the percentage of respondents who answered the questions correctly. All percentages calculated in statistical analysis were adjusted for fluctuations in the number of respondents for each prompt.
RESULTS
A total of 48 survey responses were received; 25 respondents reported their job titles as neurosurgical trainees or attending physicians, and only these responses were included for further analysis. Geographically, responses were received from those practicing in 8 countries (the US, Morocco, Australia, Guam, Bahrain, Egypt, Germany, and China) and 18 states within the US. Most neurosurgical trainees and attendings who responded practiced in the US (n = 18 responses, 72%), with Georgia, Florida, and Illinois contributing the majority of participants.
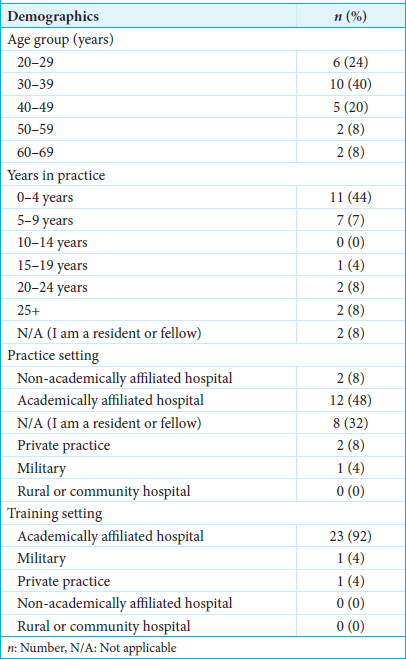
Of the neurosurgical participants, 10 (40%) were between the ages of 30 and 39 years, 6 (24%) between 20 and 29 years, and 5 (20%) between 40 and 49 years. Most respondents reported practicing between 0 and 9 years and worked at academic-affiliated hospitals. Eleven (44%) respondents reported practicing 0–4 years, and 7 (28%) had practiced 5–9 years. Of the 25 neurosurgery respondents, 23 (92%) described their training setting as an academic-affiliated hospital [
The radiation safety knowledge assessment included nine questions, which gathered 14 responses from the 25 neurosurgical participants [
In reported personal experiences and practice characteristics, 36% of respondents reported operating 5 days or more per week (n = 9), followed by 1 day at 20% (n = 5), 2 and 3 days at 16% each (n = 4), and 4 days at 12% (n = 3). Nearly half of respondents performed 1–2 operations per day (n = 13, 52%), followed by 3–4 daily operations performed (n = 10, 40%). Of respondents, 36% (n = 9) reported using intraoperative X-ray radiography in more than 50% of operations, with 28% (n = 7) using it in 25–50% of operations, and 20% (n = 5) using it in <25% of operations [
For personal radiation safety practices, most respondents reported using a lead apron (n = 22, 88%) or a thyroid shield (n = 18, 72%). A mobile radiation protection screen was only reported to be used by 36% (n = 9). In regards to the frequency of use of radiation PPE, 76% (n = 19) responded “always.” More than half of respondents, when provided with PPE, did not believe it fit correctly, with 20% reporting “never” and “sometimes” (n = 5 each). Dosimeter badges were reported as “not used” by 48% of respondents (n = 12). The response on wearing the dosimeter badge underneath lead aprons was selected by 24% of participants (n = 6). In response to safety guidelines routinely followed, 64% believed lead gowns and shields should be tested for cracks and defects annually (n = 16). Forty-four per cent also selected that fluoroscopy and all X-ray or ionizing radiation producing equipment should be calibrated annually, connections, cables, and support imaging equipment should be tested before each case, and each facility should have a radiation safety officer (n = 11) [
Thirteen participants reported feeling that they had adequate radiation safety knowledge (52%), and 15 stated that they were provided education at some point while working in neurosurgery (60%). Although 44% selected “none” for the primary format of radiation exposure education received, 24% responded as having had in-person lectures or online training courses (n = 6 each). Eleven (44%) respondents reported feeling unsatisfied with the radiation safety education received, and only 2 (8%) reported feeling satisfied [
Health risks associated with radiation exposure concerned 60% (n = 15) of respondents, and risks of radiation exposure during pregnancy were a concern for 52% (n = 13). In addition, 68% affirmed that they worry about the impact of radiation on fertility. Of the 25 respondents, 16% (n = 4) reported having been diagnosed with cancer.
DISCUSSION
The concern for radiation safety among surgeons has gained traction over recent decades. Medical literature has primarily focused on determining radiation exposure risks to patients, staff, and surgeons during individual spine and endovascular procedures. Surgical subspecialties such as urology, vascular, and orthopedics have utilized survey data to assess radiation safety knowledge and practices.[
Gaps in education, knowledge, and understanding of radiation safety
Overall, knowledge of radiation safety principles among survey participants was moderate, with only a few key questions being answered correctly by a majority. For instance, 71.4% correctly identified that increasing the surgeon’s distance from the X-ray tube by 1 meter would reduce the radiation dose to a quarter, and 85.7% knew that keeping the image intensifier close to the patient reduces the patient’s radiation exposure. These findings are consistent with the existing literature, which stresses the importance of distance and positioning in reducing radiation dose exposure. However, only 42.9% knew that the X-ray tube should be positioned under the patient, and 35.7% understood that standing on the opposite side of the tube reduces exposure in lateral C-arm imaging. These low percentages indicate a lack of critical understanding of basic protective measures, echoing similar concerns raised in other surgical fields.[
Perhaps most notably, there was a relative lack of knowledge regarding the degree and location to which radiation exposure may have the most likely negative impact on practitioners, as only 57.1% of those who filled out the knowledge assessment were able to identify the hands as the area of the body at greatest risk to radiation exposure. In addition, only 65% of participants knew that the upper outer quadrant (UOQ) of the breast is the area of highest exposure to radiation, as well as the most common site for breast cancer, which is well documented.[
In support of the likely conclusion that educational deficits may be contributing to the overall problem, a significant portion of respondents (44%) reported that they had not received formal education regarding radiation safety, and the remaining rated the education they did receive as unsatisfactory (44%) or extremely unsatisfactory (24%). The primary modes of education – when offered – were in-person lectures (24%) and online courses (24%), but no respondents reported receiving written resources or detailed practical training. Notably, radiation safety training varies widely among institutions, states, and countries, even though hospitals are required to provide formal education, and substantial research suggests the educational benefits of a formal curriculum.[
Radiation protection practices
The most important factor in the prevention of ionizing radiation is shielding. In our study, nearly all respondents used PPE most of the time, if not always, favoring either a lead apron or thyroid shield. Notably, fewer utilized other protective equipment such as lead glasses (20%) or gloves (8%) [
Despite the unique vulnerability of the breast, a recent study demonstrated that even standard lead aprons do not adequately protect the UOQ from radiation – an issue that is undoubtedly worsened by the often ill-fitting hospital-provided lead aprons, as reported by nearly 50% of survey respondents.[
Digging further into the issue, Zaidi et al.[
In the case of our study population, less than half of respondents reported regular use of a dosimeter despite 80% reporting the use of intraoperative X-ray radiography in 25% or more of their operations [
The impact of unknown or ill-limited radiation exposure should not be taken lightly. Physicians exposed to 2–5 mSv/year have a 1 in 200 attributable risk of cancer diagnosis after 15 years.[
Health and safety concerns
The importance of this study lies in the morbidity and mortality associated with radiation exposure. Deterministic effects of radiation occur in large doses, leading to cellular death and possibly resulting in hair loss, cataracts, or skin erythema. More subtle and relevant to trainees and physicians who are exposed to small doses is the cumulative cellular damage that can occur over a longer period from continued exposure, manifesting as malignancy or organ damage later in life.[
Impact of Department and Program Education and Culture
This study provides unique insight into the current inadequacies of radiation safety training and practices for neurosurgical trainees and attendings despite high levels of concern among respondents of various levels of training and practice. Highlighting these inadequacies, our respondent data demonstrate that although 60% of respondents indicated that they had received some form of radiation safety education while working in neurosurgery, 68% of respondents remained unsatisfied with the training received.
Perhaps more impactful than satisfaction with educational efforts on the topic, only half of the participants believed that they had adequate radiation safety practices implemented in their workplace. These responses suggest not only inadequate efforts at trainee and physician education regarding radiation safety but also an underutilization of workplace culture and resources to promote and support safe practices in an effort to bridge any gaps remaining after providing education on the topic. It is apparent that increased emphasis and prioritization of well-fitted and utilized radiation safety equipment are necessary to address the overall issue effectively.
Study strengths and limitations
Strengths of the study include its comprehensive assessment of radiation safety knowledge, practices, and concerns among neurosurgical professionals. By distributing the survey through various channels, including social media platforms and residency program contacts, the study provides valuable insights into the landscape of radiation safety education within neurosurgery. However, it is essential to acknowledge the limitations inherent in survey-based research, such as potential respondent biases and the inability to capture longitudinal trends. Furthermore, the small sample size of the study introduces further potential bias and limitations in terms of considering the generalization of results to the wider neurosurgical field. It highlights the limitation of the survey’s distribution through social media and email. Despite the large number of potential respondents to whom the survey was distributed (i.e., 377,000 followers and 106 residency program email addresses), it is difficult to quantify the size of the audience that would have received the survey invitation. This audience was likely further narrowed by the diffusion of responsibility in the context of public calls for survey responses or action.[
CONCLUSION
This study sheds light on the pressing issue of radiation safety education within the field of neurosurgery. The findings reveal concerns and knowledge gaps among neurosurgical trainees and physicians regarding radiation safety practices. Notably, a substantial portion of respondents expressed worries about health risks associated with radiation exposure, particularly regarding fertility and pregnancy. Furthermore, most participants found current radiation safety education in neurosurgery to be unsatisfactory. These results underscore the urgent need for targeted interventions aimed at improving radiation safety education and addressing apprehensions among neurosurgical practitioners. Radiation safety in neurosurgical education and practice is a multifaceted issue that requires multifactorial solutions; however, when the potential impact involves physician fertility and long-term health, it is of the utmost importance. Future studies are necessary to evaluate the impact of formalized radiation safety training as well as shifts in departmental and program culture on radiation safety practices and levels of exposure to trainees and physicians.
Ethical approval:
Institutional Review Board approval was not required as there are no patients in this study. The research/study complied with the Helsinki Declaration of 1964.The study is conducted in line with the policies set forth for use by Institutional Review Boards of the United States (US) starting January 20, 2019, the methods of this study meet the criteria to qualify for Exemption 45 CFR 46.104(d)(2).
Declaration of patient consent:
Patient’s consent was not required as there are no patients in this study.
Financial support and sponsorship:
Nil.
Conflicts of interest:
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation:
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Al Mohammad B, Gharaibeh M, Al Alakhras M. Knowledge and practice of radiation protection in the operating theater among orthopedic surgeons. J Med Imaging (Bellingham). 2022. 9: 066002
2. Ali MA, Salim B, Siddiqui KM, Khan MF. Attitudes and knowledge of anesthesiology trainees to radiation exposure in a Tertiary care hospital. Saudi J Anaesth. 2020. 14: 459-63
3. Alshabi YA, Yasawy MA, Makhdoom AK, Kablaghli RA, Alanazi KS, Eid SM. Knowledge regarding ionizing radiation exposure safety among orthopedic surgeons at hospitals in Al-Madinah. Cureus. 2022. 14: e30738
4. Anderson M, Goldman RH. Occupational reproductive hazards for female surgeons in the operating room: A review. JAMA Surg. 2020. 155: 243-9
5. Baumann F, Katzen BT, Carelsen B, Diehm N, Benenati JF, Peña CS. The effect of realtime monitoring on dose exposure to staff within an interventional radiology setting. Cardiovasc Intervent Radiol. 2015. 38: 1105-11
6. Beyer F, Sidarus N, Bonicalzi S, Haggard P. Beyond self-serving bias: Diffusion of responsibility reduces sense of agency and outcome monitoring. Soc Cogn Affect Neurosci. 2017. 12: 138-45
7. Bhinder J, Fakhoury E, O’Brien-Irr M, Reilly B, Dryjski M, Dosluoglu H. National survey of vascular surgery residents and fellows on radiation exposure and safety practices. J Vasc Surg. 2022. 76: 274-9.e1
8. Bhinder J, O’Brien-Irr M, Reilly B, Montross B, Khan S, Rivero M. Understanding radiation exposure and improving safety for vascular surgery trainees. J Vasc Surg. 2023. 77: 269-78
9. Bordoli SJ, Carsten CG, Cull DL, Johnson BL, Taylor SM. Radiation safety education in vascular surgery training. J Vasc Surg. 2014. 59: 860-4
10. Bowman JR, Razi A, Watson SL, Pearson JM, Hudson PW, Patt JC. What leads to lead: Results of a nationwide survey exploring attitudes and practices of orthopaedic surgery residents regarding radiation safety. J Bone Joint Surg Am. 2018. 100: e16
11. Burman S, Das A, Mahajan C, Rath GP. Radiation concerns for the neuroanesthesiologists. J Neuroanaesth Crit Care. 2021. 8: 3-11
12. Cheon BK, Kim CL, Kim KR, Kang MH, Lim JA, Woo NS. Radiation safety: A focus on lead aprons and thyroid shields in interventional pain management. Korean J Pain. 2018. 31: 244-52
13. Christakopoulos GE, Christopoulos G, Karmpaliotis D, Alaswad K, Yeh RW, Jaffer FA. Predictors of excess patient radiation exposure during chronic total occlusion coronary intervention: Insights from a contemporary multicentre registry. Can J Cardiol. 2017. 33: 478-84
14. De La Peña NM, Richter KR, Haglin JM, Pollock JR, Richter RA, Kouloumberis PE. Differences by practice year in numbers of U.S. Female neurosurgeons. World Neurosurg. 2021. 145: 363-7
15. El Zein M, Bahrami B, Hertwig R. Shared responsibility in collective decisions. Nat Hum Behav. 2019. 3: 554-9
16. Falavigna A, Ramos MB, Wong CC, Barbagallo G, Brodke D, Al-Mutair A. Commentary: Worldwide knowledge and attitude of spine surgeons regarding radiation exposure. Neurosurgery. 2018. 83: E153-61
17. Garg M, Karami V, Moazen J, Kwee T, Bhalla AS, ShahbaziGahrouei D. Radiation exposure and lifetime attributable risk of cancer incidence and mortality from low-and standard-dose CT chest: Implications for COVID-19 pneumonia subjects. Diagnostics (Basel). 2022. 12: 3043
18. Garozzo D, Rispoli R, Graziano F, Gerardi RM, Grotenhuis A, Jenkins A. Women in neurosurgery: Historical path to self-segregation and proposal for an integrated future. Front Surg. 2022. 9: 908540
19. Gilbert ES. Ionising radiation and cancer risks: What have we learned from epidemiology?. Int J Radiat Biol. 2009. 85: 467-82
20. Giordano BD, Ryder S, Baumhauer JF, DiGiovanni BF. Exposure to direct and scatter radiation with use of mini-carm fluoroscopy. J Bone Joint Surg Am. 2007. 89: 948-52
21. Godzik J, Mastorakos GM, Nayar G, Hunter WD, Tumialán LM. Surgeon and staff radiation exposure in minimally invasive spinal surgery: Prospective series using a personal dosimeter. J Neurosurg Spine. 2020. 32: 817-23
22. Günalp M, Gülünay B, Polat O, Demirkan A, Gürler S, Akkaş M. Ionising radiation awareness among resident doctors, interns, and radiographers in a university hospital emergency department. Radiol Med. 2014. 119: 440-7
23. Harris A, Loomis J, Hopkins M, Bylund J. Assessment of radiation safety knowledge among house staff exposed to fluoroscopic radiation. Urol Pract. 2019. 6: 140-5
24. Hayda RA, Hsu RY, DePasse JM, Gil JA. Radiation exposure and health risks for orthopaedic surgeons. J Am Acad Orthop Surg. 2018. 26: 268-77
25. Hsu RY, Lareau CR, Kim JS, Koruprolu S, Born CT, Schiller JR. The effect of C-arm position on radiation exposure during fixation of pediatric supracondylar fractures of the humerus. J Bone Joint Surg Am. 2014. 96: e129
26. Jenkins NW, Parrish JM, Sheha ED, Singh K. Intraoperative risks of radiation exposure for the surgeon and patient. Ann Transl Med. 2021. 9: 84
27. Jentzsch T, Pietsch CM, Stigler B, Ramseier LE, Seifert B, Werner CM. The compliance with and knowledge about radiation protection in operating room personnel: A cross-sectional study with a questionnaire. Arch Orthop Trauma Surg. 2015. 135: 1233-40
28. Kaplan DJ, Patel JN, Liporace FA, Yoon RS. Intraoperative radiation safety in orthopaedics: A review of the ALARA (as low as reasonably achievable) principle. Patient Saf Surg. 2016. 10: 27
29. Keene RR, Hillard-Sembell DC, Robinson BS, Novicoff WM, Saleh KJ. Occupational hazards to the pregnant orthopaedic surgeon. J Bone Joint Surg Am. 2011. 93: e1411-5
30. Kesari KK, Agarwal A, Henkel R. Radiations and male fertility. Reprod Biol Endocrinol. 2018. 16: 118
31. Kesavachandran CN, Haamann F, Nienhaus A. Radiation exposure of eyes, thyroid gland and hands in orthopaedic staff: A systematic review. Eur J Med Res. 2012. 17: 28
32. Khamtuikrua C, Suksompong S. Awareness about radiation hazards and knowledge about radiation protection among healthcare personnel: A quaternary care academic center-based study. SAGE Open Med. 2020. 8:
33. Kiang SC, Huh AS, Davis JR, Abou-Zamzam AM, Tomihama RT. Health care system-wide analysis identifies high radiation use factors and behaviors in surgery. Am Surg. 2021. 87: 616-22
34. Landford WN, Stewart T, Abousy M, Ngaage LM, Kambouris A, Slezak S. A roadmap for navigating occupational exposures for surgeons: A special consideration for the pregnant surgeon. Plast Reconstr Surg. 2021. 147: 513-23
35. Maghsoudi B, Mortazavi SM, Khademi S, Vatankhah P. Evaluation of radiation exposure pattern and radiation absorbed dose resulting from occupational exposure of anesthesiologists to ionizing radiation. J Biomed Phys Eng. 2017. 7: 271-8
36. Malik AT, Rai HH, Lakdawala RH, Noordin S. Does surgeon experience influence the amount of radiation exposure during orthopedic procedures? A systematic review. Orthop Rev (Pavia). 2019. 11: 7667
37. Marci R, Mallozzi M, Di Benedetto L, Schimberni M, Mossa S, Soave I. Radiations and female fertility. Reprod Biol Endocrinol. 2018. 16: 112
38. Mechlenburg I, Daugaard H, Søballe K. Radiation exposure to the orthopaedic surgeon during periacetabular osteotomy. Int Orthop. 2009. 33: 1747-51
39. Mehlman CT, DiPasquale TG. Radiation exposure to the orthopaedic surgical team during fluoroscopy: “How far away is far enough?. ” J Orthop Trauma. 1997. 11: 392-8
40. Miller DL, Vañó E, Bartal G, Balter S, Dixon R, Padovani R. Occupational radiation protection in interventional radiology: A joint guideline of the cardiovascular and interventional radiology society of Europe and the society of interventional radiology. Cardiovasc Intervent Radiol. 2010. 33: 230-9
41. National Research Council Committee on Health Effects of Exposure to Low Levels of Ionizing Radiati, editors. Health effects of exposure to low levels of ionizing radiations: Time for reassessment?. Washington, DC: National Academies Press (US)., National Academy of Sciences; 1998. p.
42. Nugent M, Carmody O, Dudeney S. Radiation safety knowledge and practices among Irish orthopaedic trainees. Ir J Med Sci. 2015. 184: 369-73
43. Office for human research protections. 45CFR 46 U.S Department of Health and Human Services. Available from: https://www.hhs.gov/ohrp/regulations-and-policy/regulations/45-cfr-46/index.html [Last accessed on 2024 Mar 13].
44. Plonsker JH, Benzil D, Air EL, Woodrow S, Stippler M, BenHaim S. Gender equality in neurosurgery and strategic goals toward a more balanced workforce. Neurosurgery. 2022. 90: 642-7
45. Rowantree SA, Currie C. Orthopaedic surgeons’ knowledge and practice of radiation safety when using fluoroscopy during procedures: A narrative review. Radiography (Lond). 2024. 30: 274-81
46. Sidwell RA, Smith HL, Halsey JP, McFarlane MJ. Surgical resident radiation knowledge, attitudes, practices, and exposures. J Surg Educ. 2016. 73: 1032-8
47. Simpson AK, Whang PG, Jonisch A, Haims A, Grauer JN. The radiation exposure associated with cervical and lumbar spine radiographs. J Spinal Disord Tech. 2008. 21: 409-12
48. Smith M, Thatcher MD, Davidovic F, Chan G. Radiation safety education and practices in urology: A review. J Endourol. 2024. 38: 88-100
49. Spetzler RF. Progress of women in neurosurgery. Asian J Neurosurg. 2011. 6: 6-12
50. Srinivasan D, Than KD, Wang AC, La Marca F, Wang PI, Schermerhorn TC. Radiation safety and spine surgery: Systematic review of exposure limits and methods to minimize radiation exposure. World Neurosurg. 2014. 82: 1337-43
51. Stack SW, Eurich KE, Kaplan EA, Ball AL, Mookherjee S, Best JA. Parenthood during graduate medical education: A scoping review. Acad Med. 2019. 94: 1814-24
52. Tomei KL, Hodges TR, Ragsdale E, Katz T, Greenfield M, Sweet JA. Best practices for the pregnant neurosurgical resident: Balancing safety and education. J Neurosurg. 2023. 138: 1758-65
53. Tunçer N, Kuyucu E, Sayar Ş, Polat G, Erdil İ Tuncay İ. Orthopedic surgeons’ knowledge regarding risk of radiation exposition: A survey analysis. SICOT J. 2017. 3: 29
54. Van Nortwick SS, Leonard DA, Finlay AK, Chou L, Valone LC. Methods for reducing intraoperative breast radiation exposure of orthopaedic surgeons. J Bone Joint Surg Am. 2021. 103: 1646-51
55. Van Papendorp LW, Suleman FE, Hanekom H. The knowledge, awareness and practices of radiation safety amongst orthopaedic surgeons. SA J Radiol. 2020. 24: 1806
56. Vosbikian MM, Ilyas AM, Watson DD, Leinberry CF. Radiation exposure to hand surgeons’ hands: A practical comparison of large and mini C-arm fluoroscopy. J Hand Surg Am. 2014. 39: 1805-9
57. Walsh DF, Thome AP, Mody KS, Eltorai AE, Daniels AH, Mulcahey MK. Radiation safety education as a component of orthopedic training. Orthop Rev (Pavia). 2019. 11: 7883
58. Yoon I, Slesinger TL, editors. Radiation exposure in pregnancy. StatPearls. Treasure Island, FL: StatPearls Publishing; 2025. p. Available from: https://www.ncbi.nlm.nih.gov/books/NBK551690 [Last accessed on 2025 May 19]
59. Yu E, Khan SN. Does less invasive spine surgery result in increased radiation exposure? A systematic review. Clin Orthop Relat Res. 2014. 472: 1738-48
60. Zaidi HA, Montoure A, Nakaji P, Bice A, Tumialán LM. A 5-year retrospective analysis of exposure to ionizing radiation by neurosurgery residents in the modern Era. World Neurosurg. 2016. 86: 220-5