- Department of Neurosurgery, Aso Iizuka hospital, 3-83 Yoshio-machi, Iizuka, Fukuoka
- Department of Neurosurgery, Aso Iizuka hospital, 3-83 Yoshio-machi, Iizuka, Fukuoka
- Department of Graduate School of Medical and Dental Sciences, Kagoshima University, Kagoshima
- Department of Pathology, Graduate School of Medical Sciences, Kyushu University
- Department of Surgery, Oita Medical Center, Oita, Japan
Correspondence Address:
Kenji Miki
Department of Neurosurgery, Aso Iizuka hospital, 3-83 Yoshio-machi, Iizuka, Fukuoka
DOI:10.25259/SNI-84-2019
Copyright: © 2019 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Kenji Miki, Koji Yoshimoto, Yuichi Yamada, Akira Kabashima, Daisuke Kuga, Yoshinao Oda, Koji Iihara. Rapid growth of metastatic brain tumor from gastric undifferentiated pleomorphic sarcoma: A case report. 24-Apr-2019;10:74
How to cite this URL: Kenji Miki, Koji Yoshimoto, Yuichi Yamada, Akira Kabashima, Daisuke Kuga, Yoshinao Oda, Koji Iihara. Rapid growth of metastatic brain tumor from gastric undifferentiated pleomorphic sarcoma: A case report. 24-Apr-2019;10:74. Available from: http://surgicalneurologyint.com/surgicalint-articles/9279/
Abstract
Background:Brain metastasis from undifferentiated pleomorphic sarcoma (UPS) is a rare occurrence, and its clinical course is little known. In this report, we investigate a case of a rapidly growing brain metastasis from gastric UPS.
Case Description:An 82-year-old man with a known gastric tumor, pathologically compatible with UPS, underwent partial gastrectomy at an outside facility. 3 months later, a 4-cm brain tumor was detected, which was completely resected. The patient was diagnosed with metastatic tumor from previously treated gastric UPS. Within 2 months of the initial resection, a large recurrent mass was detected in the same location, which was again removed. Although the patient underwent radiotherapy and chemotherapy for other metastatic tumors, he died 5 months after the second craniotomy.
Conclusions:Brain metastasis from gastric UPS is rare and difficult to treat. Although aggressive treatment, such as surgical intervention, may improve patient survival in some cases, the timing of treatment is challenging because cerebral metastasis rapidly grows and and patients frequently suffer from synchronous systematic metastasis. Therefore, early detection and close follow-up of rapidly progressing brain metastasis are important to improve treatment outcomes.
Keywords: Brain metastasis, metastatic tumor, undifferentiated pleomorphic sarcoma
INTRODUCTION
Undifferentiated pleomorphic sarcoma (UPS) mostly occurs in the extremities and deep-seated soft tissuesbut has been reported to be found on the limbs (68%) and in the abdominal cavity/retroperitoneum (16%).[
CASE REPORT
This case report is a sequel to that by Kabashima et al.[
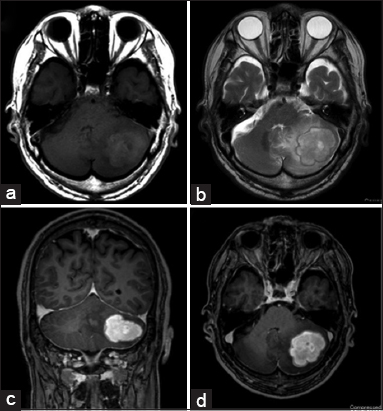
The patient underwent standard suboccipital craniotomy without navigation or monitoring, performed in the prone position, and the cerebellar tumor was completely resected. The consistency of the white–yellow tumor tissue was dense, and the tissue plane between tumor and normal brain was clearly identified and microscopic gross total resection was achieved, and his postoperative course was uneventful. Postoperative MRI (within 24 h) and contrast MRI (within 72 h) revealed complete resection of the tumor [
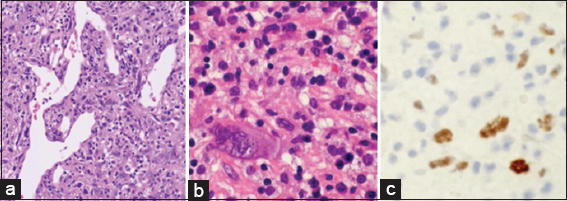
Histopathological analysis showed a proliferation of spindle-to-polygonal-shaped tumor cells with enlarged irregular nuclei and eosinophilic cytoplasm arranged in sheet-like patterns, accompanied by chronic inflammatory infiltration and hemangiopericytomas Staghorn-type branching vessels [
Figure 3
Hematoxylin and eosin (H and E) staining (a) low-power field, (b) high-power field) showed a proliferation of spindle-to-polygonal-shaped cells with irregular nuclei and eosinophilic cytoplasm arranged in a sheet-like pattern, accompanied by chronic inflammatory infiltration and hemangiopericytomas Staghorn-like branching vessels. Immunochemical staining for p53 marker was positive (c).
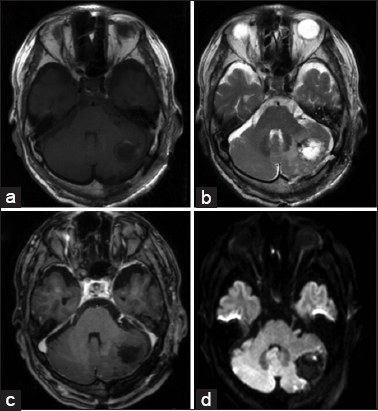
The patient underwent repeat brain imaging after 1 and ½ months at follow-up, and no apparent brain tumor residual or recurrence was observed. Only 2 weeks after that last visit, the patient started complaining of headache and nausea. A repeat MRI was ordered, which revealed a 4-cm recurrent cerebellar tumor in the same region, indicating that the 4-cm mass must have grown almost entirely within 2 weeks’ window. Since 2 weeks prior, he had undergone a non-contrast CT with 5-mm slice thickness. Systemic restaging was not performed because the pathological diagnosis was not clear. Again, the patient was taken to surgery and the recurrent tumor mass was completely resected. Histopathological findings were indistinguishable from the previous metastatic tumor again with a MIB-1 labeling index of 37%. After the second operation, the patient received focused brain radiation therapy with added local irradiation (40Gy/20Fr) and three dimensional intensity-modulated radiation therapy (30 Gy/3 Fr) to the tumor cavity. However, a second 9-mm metastatic brain tumor appeared in the temporal lobe. In addition, at the time of radiation therapy to the two lesions of the CNS, further metastatic tumors were detected in the patient’s tonsils. Although systemic chemotherapy was initiated adriamycin (30 mg/m2) plus ifosfamide (2 g/m2) (AI) at an age-adjusted dose of 75% and administered together with dexamethasone coverage;[
DISCUSSION
Sarcoma is a malignant mesenchymal tumor that originates from connective tissue of visceral organs, the digestive tract, and other soft tissues.[
Brain metastasis from sarcoma is uncommon event, and the frequency of brain metastasis in cases of metastatic systemic soft tissue sarcoma (STS) is 1–4%.[
There are a few reports of brain metastasis from sarcoma of the gastrointestinal tract and its poor prognosis.[
The prognosis of brain metastasis from UPS is not fully understood. Based on data from a case series of brain metastasis from STSs, the median survival of patients was 11.8 months.[
The National Comprehensive Cancer Network guidelines for soft tissue tumors state that surgery is the most effective treatment, combined with either chemotherapy or radiotherapy depending on the patient’s performance status.[
In our case, both the initial and the recurrent metastatic brain tumors were rapidly growing. The first brain metastasis was detected only 2 months after gastrectomy, despite a localized primary tumor (T2N0M0). Moreover, the recurrent brain metastasis was detected again within only 2 months after craniotomy. Despite successful gross total resection and adjuvant treatment, our patient died 6 months after developing his first symptom.
Compared to other gastric cancers, this growth rate of the tumor was considered high, as the mean interval from gastrectomy to the diagnosis of brain metastasis has been reported to be 9.6 months.[
Based on our experience with this infrequent UPS brain metastasis, we want to alert neurosurgical oncologists to consider the possibility of brain metastasis from these rare gastric UPSs in their differential. We recommend that the brain should be frequently screened by MRI after resection of such a gastric tumor because UPS brain metastasis has shown rapid growth and it may be difficult to detect them clinically on early routine checkups if there are no symptoms. Further studies are needed to identify the best treatment algorithm which may include surgery, SRS, and adjuvant chemotherapy.
CONCLUSIONS
Brain metastasis from gastric UPS is rare. Although the tumor growth is rapid and aggressive treatment is important, accurate pathological diagnosis is difficult due to the tumor’s rarity and its rapid progression. To detect metastatic CNS tumors from UPS early, routine MRI screening should be considered.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. We got patient’s consent for his images and other clinical information to be reported in the journal. On his passing, we obtained informed consent from his wife, as the next of kin. The consent was obtained with the understanding that names and initials will not be published, and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Agaimy A, Gaumann A, Schroeder J, Dietmaier W, Hartmann A, Hofstaedter F. Primary and metastatic high-grade pleomorphic sarcoma/malignant fibrous histiocytoma of the gastrointestinal tract:An approach to the differential diagnosis in a series of five cases with emphasis on myofibroblastic differentiation. Virchows Arch. 2007. 451: 949-57
2. Chua C, Raaj J, Pan S, Farid M, Lee JF, Ho ZC. Brain metastasis in sarcoma:Does metastasectomy or aggressive multi-disciplinary treatment improve survival outcomes. Asia Pac J Clin Oncol. 2016. 12: e16-22
3. Espat NJ, Bilsky M, Lewis JJ, Leung D, Brennan MF. Soft tissue sarcoma brain metastases. Prevalence in a cohort of 3829 patients. Cancer. 2002. 94: 2706-11
4. Fletcher CD, Unni KK, Mertens F.editorsWorld Health Organization Classification of Tumors:Pathology and Genetics of Tumors of Soft Tissue and Bone. Lyon: IARC Press; 2002. p.
5. Fox BD, Patel A, Suki D, Rao G. Surgical management of metastatic sarcoma to the brain. J Neurosurg. 2009. 110: 181-6
6. Honoré C, Méeus P, Stoeckle E, Bonvalot S. Soft tissue sarcoma in france in 2015:Epidemiology, classification and organization of clinical care. J Visc Surg. 2015. 152: 223-30
7. Jo VY, Fletcher CD. WHO classification of soft tissue tumours:An update based on the 2013 (4th) edition. Pathology. 2014. 46: 95-104
8. Kabashima A, Kimura K, Sanefuji K, Masunari S, Haraoka S, Maekawa S. Acase of primary gastric undifferentiated high-grade pleomorphic sarcoma diagnosed with chief complaint of fever:A case report and literature review. Surg Case Rep. 2017. 3: 41-
9. Kasakura Y, Fujii M, Mochizuki F, Suzuki T, Takahashi T. Clinicopathological study of brain metastasis in gastric cancer patients. Surg Today. 2000. 30: 485-90
10. Kasper E, Mahadevan A. Stereotactic radiosurgery for sarcoma. JSM Neurosurg Spine. 2014. 2: 1032-
11. Kataoka K, Tanaka K, Mizusawa J, Kimura A, Hiraga H, Kawai A. Arandomized phase II/III trial of perioperative chemotherapy with adriamycin plus ifosfamide versus gemcitabine plus docetaxel for high-grade soft tissue sarcoma:Japan clinical oncology group study JCOG1306. Jpn J Clin Oncol. 2014. 44: 765-9
12. Matushansky I, Charytonowicz E, Mills J, Siddiqi S, Hricik T, Cordon-Cardo C. MFH classification:Differentiating undifferentiated pleomorphic sarcoma in the 21stcentury. Expert Rev Anticancer Ther. 2009. 9: 1135-44
13. [Last accessed 2016 Apr 12]. Available from: https://www.nccn.org/patients/guidelines/sarcoma.
14. Postovsky S, Ash S, Ramu IN, Yaniv Y, Zaizov R, Futerman B. Central nervous system involvement in children with sarcoma. Oncology. 2003. 65: 118-24
15. Rathakrishnan V, Arianayagam S, Kumar G. Primary malignant fibrous histiocytoma of the stomach:(a case report). Australas Radiol. 1989. 33: 302-4
16. Shibuya H, Azumi N, Onda Y, Abe F. Multiple primary malignant fibrous histiocytoma of the stomach and small intestine. Acta Pathol Jpn. 1985. 35: 157-64
17. Tanaka H, Sasayama T, Nishihara M, Arai A, Kawamura A, Kanomata N. Brain metastasis of undifferentiated sarcoma and response to temozolomide treatment. Case report. Neurol Med Chir (Tokyo). 2010. 50: 689-93
18. Wada Y, Matsushita T, Sarumaru S, Ryo J, Isobe H, Satoh B. Malignant fibrous histiocytoma of the stomach:Report of two cases. Surg Today. 1998. 28: 296-300
19. Weiss SW, Enzinger FM. Malignant fibrous histiocytoma:An analysis of 200 cases. Cancer. 1978. 41: 2250-66
20. Wiersema AM, Wobbes T, Pruszczynski M, van der Sluis RF. Malignant fibrous histiocytoma of the stomach during pregnancy:A case report. Eur J Obstet Gynecol Reprod Biol. 1998. 80: 71-3
21. Yoo H, Nam BH, Yang HS, Shin SH, Lee JS, Lee SH. Growth rates of metastatic brain tumors in nonsmall cell lung cancer. Cancer. 2008. 113: 1043-7