- Department of Neurosurgery, Kurume University School of Medicine, Kurume, Japan
- Department of Radiology, Kurume University School of Medicine, Kurume, Japan
Correspondence Address:
Nobuyuki Takeshige
Department of Neurosurgery, Kurume University School of Medicine, Kurume, Japan
DOI:10.4103/sni.sni_245_17
Copyright: © 2018 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Nobuyuki Takeshige, Tomoko Eto, Shinji Nakashima, Kiyohiko Sakata, Hisaaki Uchikado, Toshi Abe, Motohiro Morioka. Rare case of a rapidly enlarging symptomatic arachnoid cyst of the posterior fossa in an infant: A case report and review of the literature. 07-Mar-2018;9:57
How to cite this URL: Nobuyuki Takeshige, Tomoko Eto, Shinji Nakashima, Kiyohiko Sakata, Hisaaki Uchikado, Toshi Abe, Motohiro Morioka. Rare case of a rapidly enlarging symptomatic arachnoid cyst of the posterior fossa in an infant: A case report and review of the literature. 07-Mar-2018;9:57. Available from: http://surgicalneurologyint.com/surgicalint-articles/rare-case-of-a-rapidly-enlarging-symptomatic-arachnoid-cyst-of-the-posterior-fossa-in-an-infant-a-case-report-and-review-of-the-literature/
Abstract
Background:Intracranial arachnoid cysts are space-occupying lesions that typically remain stable or decrease in size over time. Cysts in infants younger than 1 year of age are remarkably different from those in older children and adults in terms of cyst localization and enlargement. Arachnoid cysts of the posterior fossa (PFACs) are very rare in infants and do not typically grow or present with clinical symptoms, such that surgical treatment is generally considered to be unnecessary. Here, we describe an extremely rare case of an infant with a rapidly enlarging symptomatic PFAC that was successfully treated with surgery.
Case Description:A 4-month-old boy presented with increasing head circumference and a rapidly enlarging arachnoid cyst in the left posterior fossa with ventriculomegaly, which was documented using serial imaging over the preceding 2 months. We performed a microscopic resection of the cyst membrane to remove the mass effect as soon as possible and facilitate normal development. To confirm dural closure and prevent cerebrospinal fluid leakage, we also performed short-term (7 days) percutaneous long-tunneled external ventricle drainage after the surgery. Magnetic resonance imaging over a 4-year follow-up period revealed adequate reduction of the ventricle and cyst. The patient no longer exhibited progressive macrocrania and showed normal development.
Conclusion:To our knowledge, this is the second successful case of surgical treatment of an enlarging symptomatic PFAC in an infant. Our surgical strategy for the treatment of this rare case can serve as a guide for surgeons in similar future cases.
Keywords: Arachnoid cyst, cyst enlargement, hydrocephalus, posterior fossa
INTRODUCTION
Congenital arachnoid cysts are rare central nervous system malformations that represent only 1–2% of all intracranial masses.[
The characteristics of arachnoid cysts vary remarkably between infants and older children or adults. In adults, the majority of intracranial arachnoid cysts arise in the supratentorial region (90%), with the middle cranial fossa being the most common site (60%) of origin and 10–20% of arachnoid cysts occurring in the posterior fossa.[
Here, we present an extremely rare case of a 4-month-old boy who presented with a rapidly enlarging symptomatic PFAC. After considering the current options for treating symptomatic PFACs in infants,[
CASE PRESENTATION
History
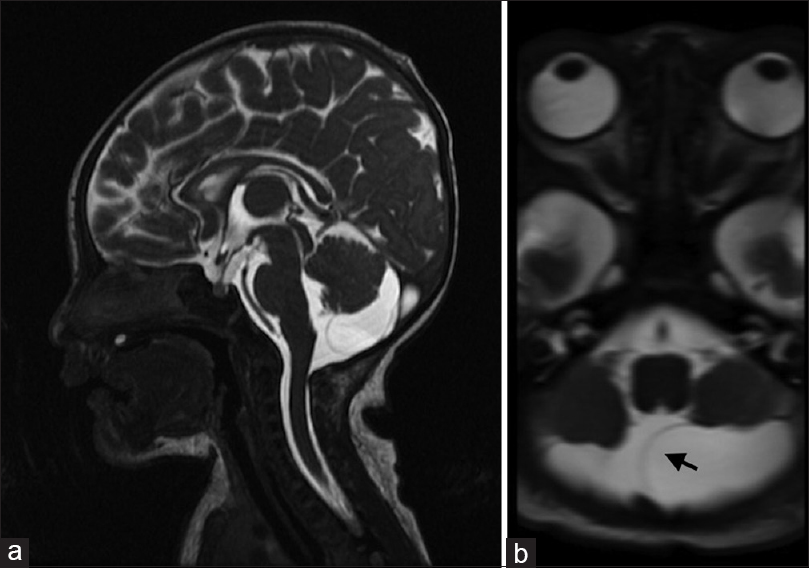
The patient in the present case was a boy that was born by vaginal delivery at 42 weeks of gestation. He had a birth weight of 2546 g, a normal head circumference (32.1 cm), and exhibited no neurological abnormalities. Based on the detection of an ultrasonographic abnormality, magnetic resonance imaging (MRI) was performed at 58 days after birth and a cystic lesion (1.2 cm × 2.9 cm at its largest diameter) was identified in the left retrocerebellar region of the posterior fossa [
Examinations
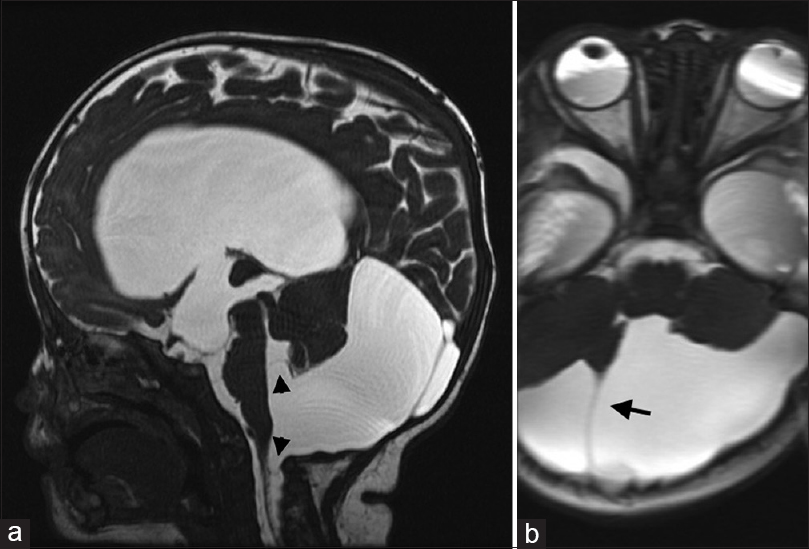
At 4 months of age, the patient's head circumference increased to 48.0 cm (>2 standard deviations above the mean for his age), and MRI showed significant enlargement of the cyst (4.0 cm × 3.5 cm at its largest diameter) with compression of the cerebellum and hydrocephalus caused by obstruction of the fourth ventricle outlets [
Figure 2
Preoperative sagittal (a) and axial (b) T2 magnetic resonance images of the patient at 4 months of age. An enlarged cystic lesion can be observed descending into the foramen magnum with the septum expanding beyond the midline (arrow). Blocked communication with the fourth ventricle, compression of the brainstem and fourth ventricle (arrowheads), and marked ventriculomegaly (stars) were evident
Surgical procedure
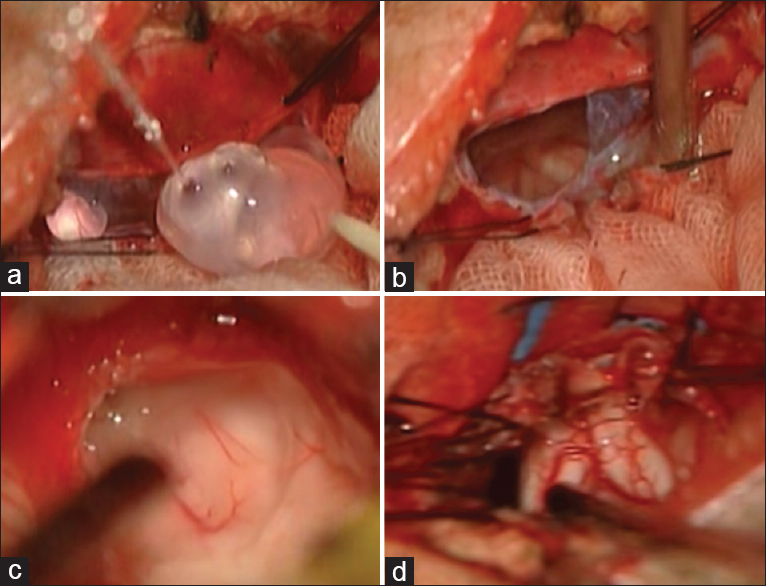
Clinical signs and symptoms of hydrocephalus were observed when the patient was 4 months of age. Thus, we performed a suboccipital craniotomy and direct microscopic treatments to resect the cyst membrane via a medial occipital approach with the patient in the prone position. This was done to restore normal communication between the Magendie and Lushka foramina and the subarachnoid space. Because the inner membrane of the cyst adhered to the rostral medullary velum and compressed the fourth ventricle, we carefully detached and resected both the outer and inner membranes of the cyst to open the fourth ventricle and cisterna magna [
Postoperative course
The postoperative course was uneventful. MRI performed 1 month after the surgery revealed that the cyst had disappeared, alleviating compression of the cerebellum and halting the patient's macrocrania. Further, the sulci of the cerebellum and the cerebellar pontine angle became easier to observe. At the last follow-up (performed 4 years postoperatively), the cyst wall was unidentifiable and the cerebellum had grown to near-normal size [
Figure 4
Computed tomography performed 4 years after the surgery. The image demonstrates absence of the septum as well as reduced compression of the brainstem and fourth ventricle. Furthermore, the image clearly depicts the sulci of the cerebellum, the cerebellopontine angle, and amelioration of the patient's obstructive hydrocephalus
DISCUSSION
An arachnoid cyst consists of a cavity lined with arachnoid cells and filled with fluid that closely resembles CSF.[
The differential diagnosis of PFACs in infants mainly includes the Dandy–Walker malformation, mega cisterna magna, and Blake's pouch cyst.[
Although very little data exist regarding the clinical characteristics of arachnoid cysts in infant cases, these characteristics have gradually become evident.[
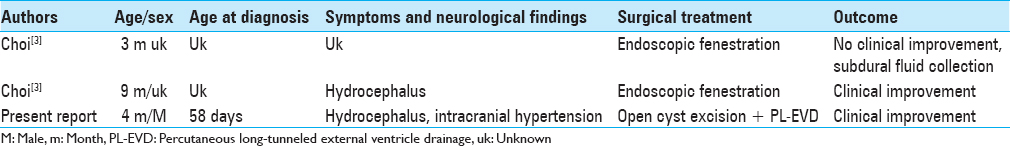
To date, only 2 cases of enlarging symptomatic PFACs and surgical treatment have been reported in infant patients [
The infratentorial space is much smaller than the supratentorial space; accordingly, mass effects related to arachnoid cysts are more probable in the infratentorial space than in the supratentorial space. Especially in infants with very small infratentorial spaces, mass effects must be removed as soon as possible to facilitate normal development.
PFACs can be particularly challenging to treat depending on the cyst size, cyst location, and the presence of obstructive hydrocephalus.[
There is relatively high risk of postoperative complications such as CSF leakage, subdural fluid collection, and meningitis after surgery on the posterior fossa, especially in infants.[
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Al-Holou WN, Yew AY, Boomsaad ZE, Garton HJL, Muraszko KM, Maher CO. Prevalence and natural history of arachnoid cysts in children. J Neurosurg Pediatr. 2010. 5: 578-85
2. Ali ZS, Lang SS, Bakar D, Storm PB, Stein SC. Pediatric intracranial arachnoid cysts: Comparative effectiveness of surgical treatment options. Childs Nerv Syst. 2014. 30: 461-9
3. Choi JW, Lee JY, Phi JH, Kim S-K, Wang KC. Stricter indications are recommended for fenestration surgery in intracranial arachnoid cysts of children. Childs Nerv Syst. 2015. 31: 77-86
4. Cincu R, Agrawal A, Eiras J. Intracranial arachnoid cysts: Current concepts and treatment alternatives. Clin Neurol Neurosurg. 2007. 109: 837-43
5. Collins CD, Hartley JC, Chakraborty A, Thompson DN. Long subcutaneous tunnelling reduces infection rates in paediatric external ventricular drains. Childs Nerv Syst. 2014. 30: 1671-8
6. Edingler P, Kaynar MY, Bozkus H, Qiplak N. Posterior fossa arachnoid cysts. Br J Neurosurg. 1999. 13: 10-7
7. Fulkerson DH, Vogel TD, Baker A, Patel N, Ackerman L, Smith JL. Cyst-ventricle stent as primary or salvage treatment for posterior fossa arachnoid cysts. J Neurosurg Pediatr. 2011. 7: 549-56
8. Gangemi M, Seneca V, Colella G, Cioffi V, Imperato A, Maiuri F. Endoscopy versus microsurgical cyst excision and shunting for treating intracranial arachnoid cysts. J Neurosurg Pediatr. 2011. 8: 158-64
9. Gnanalingham KK, Hafuente J, Thompson D, Harkness W, Hayward R. Surgical procedures for posterior fossa tumors in children: Does craniotomy lead to fewer complications than cranioectomy. J Neurosurg. 2002. 97: 821-6
10. Halani H, Mina MS, Safain G, Heilman CB. Arachnoid cyst slit valves: the mechanism for arachnoid cyst enlargement. Report of 5 cases. J Neurosurg Pediatr. 2013. 12: 62-6
11. King JAJ, Auguste KI, Halliday W, Drake JM, Kulkarni AV. Ventriculocystostomy and endoscopic third ventriculostomy/shunt placement in the management of hydrocephalus secondary to giant retrocerebellar cysts in infancy. J Neurosurg Pediatr. 2010. 5: 403-7
12. Kumagai M, Sakai N, Yamada H, Shinoda J, Nakashima T, Iwama T. Postnatal development and enlargement of primary middle cranial fossa arachnoid cyst recognized on repeat CT scan. Childs Nerv Syst. 1986. 2: 211-5
13. Lee JY, Kim JW, Phi JH, Kim SK, Cho BK, Wang KC. Enlarging arachnoid cyst: A false alarm for infants. Childs Nerv Syst. 2012. 28: 120311-
14. Marin-Sanabria EA, Yamamoto H, Nagashima T, Kohmura E. Evaluation of the management of arachnoid cyst of the posterior fossa in pediatric population: Experience over 27 years. Childs Nerv Syst. 2007. 23: 535-42
15. Matsumoto J, Kochi M, Morioka M, Nakamura H, Makino K, Hamada J. A long-term ventricular drainage for patients with germ cell tumors or medulloblastoma. Surg Neurol. 2006. 65: 74-80
16. Oberbauer RW, Haase J, Pucher R. Arachnoid cysts in children: A European co-operative study. Childs Nerv Syst. 1992. 8: 281-6
17. Parizek J, Mericka P, Nemecek S, Nemeckova J, Spacek J, Suba P. Posterior cranial fossa surgery in 454 children. Comparison of results obtained in pre-CT and CT era and after various types of management of dura mater. Childs Nerv Syst. 1998. 14: 426-38
18. Raju S, Sharma RS, Moningi S, Momin J. Neuroendoscopy for Intracranial Arachnoid Cysts in Infants: Therapeutic Considerations. J Neurol Surg. 2015. 77: 333-43
19. Rao G, Anderson RCE, Feldstein NA, Brockmeyer DL. Expansion of arachnoid cysts in children. J Neurosurg. 2015. 102: 314-7
20. Sikorski CW, Yamani B, Frim DM. Endoscopic cyst fenestration outcomes in children one year of age or less. Pediatr Neurosurg. 2004. 40: 59-63
21. Srinivasan US, Lawrence R. Posterior fossa arachnoid cysts in adults: Surgical strategy: Case series. Asian J Neurosurg. 2015. 10: 47-51
22. Tsuboi Y, Hamada H, Hayashi N, Kurimoto M, Hirashima Y, Endo S. Huge arachnoid cyst in the posterior fossa: Controversial discussion for selection of the surgical approach. Childs Nerv Syst. 2005. 21: 259-61
23. Wilkinson CC, Wilson KR, Albright AL, Pollack IF, Adelson PD.editors. Congenital arachnoid cyst and Dandy-Walker complex. Principles and Practice of Pediatric Neurosurgery. Thieme: New York; 2008. p. 162-86
24. Zada G, Krieger MD, McNatt S, Bowen I, McComb JG. Pathogenesis and treatment of intracranial arachnoid cysts in pediatric patients younger than 2 years of age. Neurosurg Focus. 2007. 22: E1-