- Department of Neurosurgery, University of Missouri, School of Medicine, Columbia, Missouri, United States
- Department of Neurosurgery, University of Illinois, College of Medicine, Chicago, Chicago, Illinois, United States
- Department of Neurosurgery, University of Missouri, Columbia, Missouri, United States
Correspondence Address:
Sabrina Maria Genovese, Department of Neurosurgery, University of Missouri, School of Medicine, Columbia, Missouri, United States.
DOI:10.25259/SNI_795_2024
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Sabrina Maria Genovese1, Jakov Tiefenbach2, Ravi A. Nunna3, Andrew Youkilis3. Rare histiocytic neoplasm: A case report. 22-Nov-2024;15:431
How to cite this URL: Sabrina Maria Genovese1, Jakov Tiefenbach2, Ravi A. Nunna3, Andrew Youkilis3. Rare histiocytic neoplasm: A case report. 22-Nov-2024;15:431. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=13242
Abstract
Background: Histiocytic neoplasms are defined by too many histiocytes accumulating in various tissues, including the skin, bones, lymph nodes, and central nervous system. They are uncommon blood-related disorders that constitute
Case Description: A 76-year-old male presented with the month of slowly progressive bilateral lower extremity weakness (i.e., right > left) accompanied by decreased left-sided sensation below the T7 level. The enhanced thoracic magnetic resonance (MR) imaging documented an intradural intramedullary nodule at the T5 level with a syrinx extending from C7 to T10. The patient underwent a T4–T6 laminectomy for complete resection of the lesion. CD163 and CD68 studies highlighted a small, spindled-shaped tumor with occasionally enlarged histiocytes without co-positivity for S100. Pathologically, the lesion was considered an isolated intramedullary thoracic LCH.
Conclusion: A 76-year-old male presented with progressive paraparesis of 1 month’s duration attributed to an enhanced MR-documented T5 single intramedullary T5 thoracic LCH that was successfully resected.
Keywords: Histiocytic neoplasm, Histiocytosis-X, Langerhans cell histiocytosis, Rosai–Dorfman disease, Spine
INTRODUCTION
Histiocytic neoplasms make up <1% of cancers found in soft tissues and lymph nodes.[
CASE REPORT
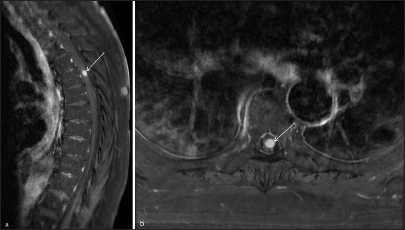
A 76-year-old male presented with progressive bilateral lower extremity paraparesis of 1 month’s duration accompanied by a left-sided T7 pin level. His neurologic examination showed mild right-sided (i.e., 4/5 hip flexion) but predominantly left-sided weakness (i.e., left 2/5 hip flexion/knee extension and 3/5 dorsiflexion/plantar flexion), accompanied by decreased pin appreciation on the left below the T7 level. The contrast thoracic MR showed a single intramedullary nodule at the T5 level with a syrinx extending from C7 to T10 [
Surgery
The patient underwent a T4–T6 laminectomy for complete resection of the intradural intramedullary C5 spinal cord lesion under neuromonitoring (Motor-evoked potential/Somatosensory-evoked potentials). The mass was pale yellow-whitish in color, well-encapsulated, and firm. Total en bloc excision was accomplished as there was a clear margin of demarcation of the tumor from the cord.
Pathology
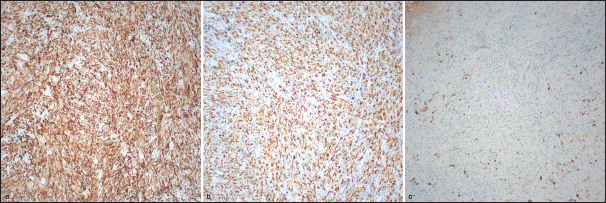
Pathologic findings were diagnostic for an isolated intramedullary thoracic histiocytic neoplasm comprised of chronic inflammation with histiocytes. CD163 and CD68 studies highlighted small, spindled-shaped, and occasionally enlarged histiocytes [
Postoperative course
Postoperatively, the patient was nearly paraplegic, requiring transfer to an inpatient rehabilitation center. When reexamined at 4 postoperative months, left lower extremity motor function had improved to 3–4/5 proximal/distal, with the right-sided function now at 4–5/5. Nevertheless, he exhibited persistently decreased pin appreciation bilaterally below the T8 level.
DISCUSSION
Pathological diagnosis of histiocytosis
Confirmation of histiocytosis requires both biopsy and histological analysis. H&E stains revealed large, foamy histiocytic cells, while the basic immunohistochemistry panel included CD163/CD68, S100, CD1a, Langerin/CD207, cyclin D1, and factor XIIIa.[
Treatment of histiocytosis
The treatment for histiocytic neoplasms includes surgical resection, steroids, imiquimod, radiation therapy, and complex chemotherapy regimens [
CONCLUSION
A 76-year-old male with 1 month of progressive paraparesis/left-sided T7 pin level underwent a T4–T6 laminectomy to remove an MR-documented enhancing single intramedullary T5 lesion; pathologically, the tumor was a LCH. Four months postoperatively, the patient exhibited an improved although moderate residual paraparesis, but with residual decreased bilateral pin appreciation below the T8 level.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Abu-Bonsrah N, Goodwin CR, Crane GM, Abiola G, Sciubba DM. Langerhans cell histiocytosis of the cervical spine. Spine J. 2016. 16: e11-2
2. Allen CE, Ladisch S, McClain KL. How I treat Langerhans cell histiocytosis. Blood. 2015. 126: 26-35
3. El Molla M, Mahasneh T, Holmes SE, Al-Khawaja D. Rare presentation of rosai-dorfman disease mimicking a cervical intramedullary spinal cord tumor. World Neurosurg. 2014. 81: 442.e7-9
4. Emile JF, Abla O, Fraitag S, Horne A, Haroche J, Donadieu J. Revised classification of histiocytoses and neoplasms of the macrophage-dendritic cell lineages. Blood. 2016. 127: 2672-81
5. Go RS, Jacobsen E, Baiocchi R, Buhtoiarov I, Butler EB, Campbell PK. Histiocytic neoplasms, version 2.2021, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw. 2021. 19: 1277-303
6. Hamilton B, Connolly ES, Mitchell WT. Isolated intramedullary histiocytosis-X of the cervical spinal cord: Case report. J Neurosurg. 1995. 83: 716-8
7. Jones MP, Rueda-Pedraza ME. Extranodal sinus histiocytosis with massive lymphadenopathy presenting as an intramedullary spinal cord tumor: A case report. Am J Hematol. 1997. 54: 253-7
8. Nayef RF, Ossama AM, John TG, John RJ, John LF. Histiocytosis-X of the spinal cord: A case report. Neurosurgery. 1986. 19: 837-40
9. Osenbach RK. Isolated extranodal sinus histiocytosis presenting as an intramedullary spinal cord tumor with paraplegia: Case report. J Neurosurg. 1996. 85: 692-6
10. Rocha-Maguey J, Felix-Torrontegui JA, Cabrera-López M, Gutiérrez-Castro M, Montante-Montes D. A new case of cervical intramedullary sinus histiocytosis causing paraplegia and review of the literature. Surg Neurol Int. 2016. 7: 9
11. Sandoval-Sus JD, Sandoval-Leon AC, Chapman JR, Velazquez-Vega J, Borja MJ, Rosenberg S. Rosai-Dorfman disease of the central nervous system: Report of 6 cases and review of the literature. Medicine (Baltimore). 2014. 93: 165-75
12. Yamagata T, Takami T, Yamamoto N, Tanaka S, Wakasa K, Ohata K. Primary intramedullary langerhans cell histiocytosis of the thoracic spinal cord. Neurol Med Chir (Tokyo). 2013. 53: 245-8