- Department of Orthopedics School of Medicine, State University of New York at Stony Brook, NY, USA.
- Department of Neurosurgery, NYU Winthrop Hospital, Mineola, NY, School of Medicine, State University of New York at Stony Brook, NY, USA.
- Department of Clinical Professor of Neurological Surgery, School of Medicine, State University of New York at Stony Brook, NY, USA.
Correspondence Address:
Nancy E. Epstein
Department of Neurosurgery, NYU Winthrop Hospital, Mineola, NY, School of Medicine, State University of New York at Stony Brook, NY, USA.
Department of Clinical Professor of Neurological Surgery, School of Medicine, State University of New York at Stony Brook, NY, USA.
DOI:10.25259/SNI_326_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Marc Agulnick1, Benjamin R. Cohen2, Nancy E. Epstein2,3. Reconstruction of Shattered Lumbo-Sacral Junction/Pelvis Utilizing Bilateral L4-Sacrum Fibula Strut Allograft And Double Iliac Screws Plus Routine Lumbar Pedicle Screw Fixation. 15-Oct-2020;11:335
How to cite this URL: Marc Agulnick1, Benjamin R. Cohen2, Nancy E. Epstein2,3. Reconstruction of Shattered Lumbo-Sacral Junction/Pelvis Utilizing Bilateral L4-Sacrum Fibula Strut Allograft And Double Iliac Screws Plus Routine Lumbar Pedicle Screw Fixation. 15-Oct-2020;11:335. Available from: https://surgicalneurologyint.com/surgicalint-articles/10323/
Abstract
Background: A traumatically shattered lumbosacral junction/pelvis may be difficult to repair. Here the authors offer a pelvic fixation technique utilizing routine pedicle screws, interbody lumbar fusions, bilateral iliac screws/ rods/crosslinks, and bilateral fibular strut allografts from the lumbar spine to the sacrum.
Methods: A middle aged male sustained a multiple storey fall resulting in a left sacral fracture, and right sacroiliac joint (SI) dislocation. The patient had previously undergone attempted decompressions with routine pedicle screw L4-S1 fusions at outside institutions; these failed twice. When the patient was finally seen, he exhibited, on CT reconstructed images, MR, and X-rays, a left sacral fracture nonunion, and a right sacroiliac joint dislocation.
Results: The patient underwent a bilateral pelvic reconstruction utilizing right L4, L5, S1 and left L4, L5 pedicle screws plus interbody fusions (L4-L5, and L5, S1), performed from the left. Unique to this fusion construct was the placement of bilateral double iliac screws plus the application of bilateral fibula allografts from L4-sacrum filled with bone morphogenetic protein (BMP). After rod/screw/connectors were applied, bone graft was placed over the fusion construct, including the decorticated edges of the left sacral fractures, and right SI joint dislocation. We additionally reviewed other pelvic fusion reconstruction methods.
Conclusions: Here, we utilized a unique pelvic reconstruction technique utilizing pedicle screws/rods, double iliac screws/rods, and bilateral fibula strut grafts extending from the L4-sacrum filled with BMP.
Keywords: Bypass lumbar fracture, Fibula allograft, Ischial fusion, Pedicle screws, Reconstruction, Sacral disruption, Sacral fracture, Sacroiliac joint dislocation, Sacral screws
INTRODUCTION
A traumatically shattered lumbosacral junction may be difficult to repair. Here, we present a patient who had sustained a left sacral fracture, and right sacroiliac joint dislocation who had previously undergone two failed attempts at lumbo-sacral junction pelvic fusion. Here, we performed the routine placement of left-sided lumbar L4 and L5, and right-sided lumbar L4, L5, and S1 pedicle Agulnic, et al: Technical Note: Reconstruction of Shattered Lumbo-Sacral Junction/Pelvis Utilizing Bilateral L4-Sacrum Fibula Strut screws with accompanying interbody L4-L5, and L5-S1 fusions. Further, bilateral double iliac screws were connected to the L4-L5/L4-S1 pedicle screw construct. However, unique in this case was the additional placement of bilateral fibula strut allografts filled with bone morphogenetic protein (BMP) placed from the L4 levels bilaterally to the sacrum.
Video of Technique to Treat Sacral Fracture (Illustrated File)
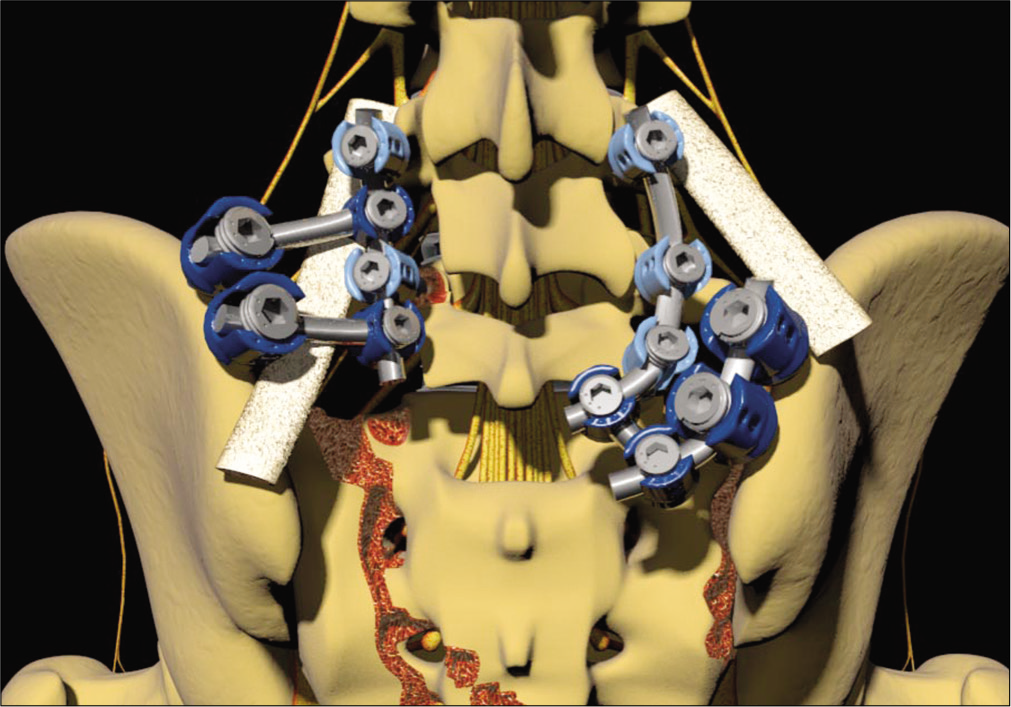
An initial midline lumbo-sacral incision is accompanied by bilateral lateral incisions over both iliac crests. All the soft tissue is then removed from the posterolateral elements between L4, and the pelvis. Using normal anatomical landmarks, bilateral pedicle screws are placed at the L4 and L5 levels, while bilateral iliac screws are placed in the pelvis. Next, the posterolateral elements are decorticated between the L4-L5 levels including the sacral ala. This is followed by the application of bilateral cadaveric fibular strut grafts filled with Bone Morphogenetic Protein (Infuse: Medtronic, Memphis, USA) to create a bridge between the lumbar transverse processes of L4 and L5 with the sacral ala. The fibula struts are secured using bone suture anchors (BSA) and FiberWire (Arthrex: 1370 Creekside Boulevard Naples, Florida). The FiberWire has an ultra-high molecular weight polyethylene multifilament core surrounded by a braided poly-ester jacket with a silicone coating for ease of handling, and knot-tying. This is followed by lumbar pedicle screw placement bilaterally (e.g. L4, L5, S1), and the application of bilateral double iliac screws; rods and cross-links are then appropriately placed, and tightened [
Figure 1:
PA Illustration of Bilateral Pelvic Fixation Construct.
After a multi-storey fall, a middle aged male sustained a left sacral fracture, and right sacroiliac joint dislocation, He had been operated on twice previously; both attempts resulted in pseudarthroses/failed fusions. Here is the illustration of the repair technique finally perfomed. This consisted of right-sided application of L4, L5, S1 pedicle screws (to address the right SI joint dislocation), and left L4 and L5 pedicle screw fixation (to address left sacral fracture). Additionally, interbody PEEK (polyetheretherketone) fusions at both L4-L5 and L5-S1, the placement of bilateral iliac screws, and the bilateral application of fibula strut allografts filled with BMP/INFUSE were placed over the transverse processes of L4 and L5 down to the sacrum. Rods were then attached along with cross-links.
Figure 2:
Left Oblique Illustration of Pelvic Fixation Construct For Left Sacral Fracture.
This image clearly shows the left-sided pedicle screws placed in L4 and L5 (not S1), and the two screws placed in the ilium on both sides. Note the completed placement of the rod/cross-link system affixed to the screws. You can also see the fibula strut graft extending from L4 to the sacrum on the left.
Figure 3:
Right Oblique Illustration of Pelvic Fixation Construct for Right Sacroiliac Joint Dislocation.
This image clearly shows the pedicle screws placed on the right side at the L4, L5, and S1 levels, plus the two screws placed in the ilium. Note the completed placement of the rod/cross-link system affixed to the screws. You can also see the fibula strut graft extending from L4 to the sacrum.
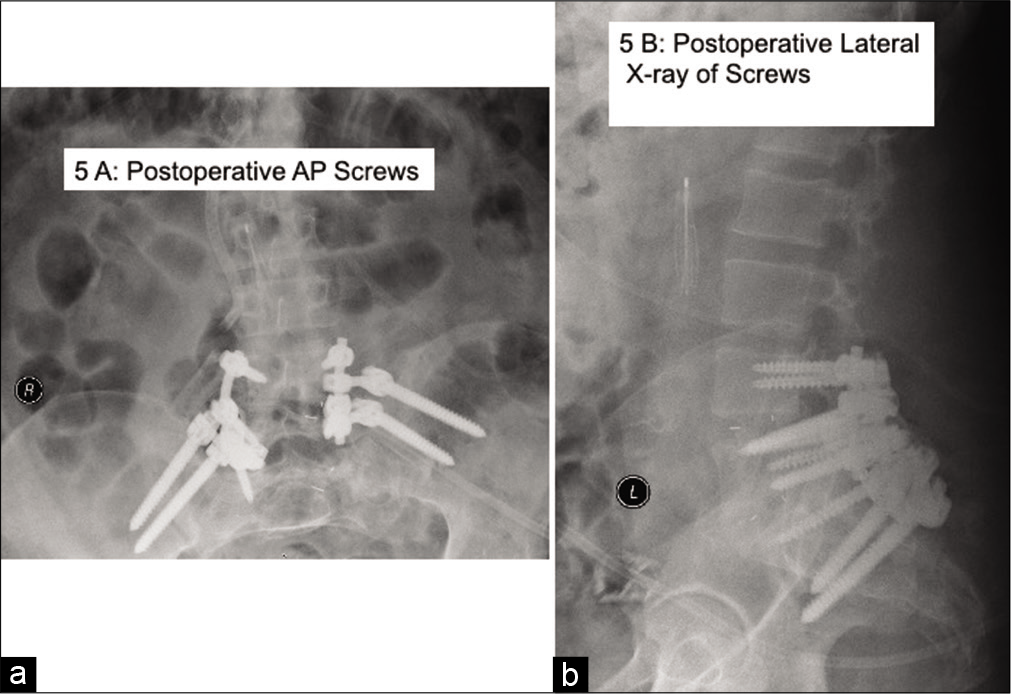
Figure 5:
(a and b) Postoperative AP and Lateral X-rays Showing Pelvic Construct.
(a) The postoperative AP X-ray shows the entire pelvic construct. On the right you can see the pedicle screws in L4, L5, and S1 while on the left, pedicle screws were found only in L4 and L5. Bilateral double iliac screws were placed, and you can see the rods, and rod/ screw connectors. Also the fibula strut was clearly visualized on the left extending over the transverse processes from L4-L5 to the sacrum; this was not so clearly seen on the right. (b) The lateral X-ray confirmed the construct as outlined above.
Case Study
A middle aged male sustained a multiple storey fall resulting in a left sacral fracutre, and right sacroiliac joint dislocation. He had previously undergone two failed decompressions with L4-S1 pedicle/screw fusions at outside institutions. When the patient was finally seen in preparation for the third surgery, the CT reconstructed images, MR, and X-rays demonstrated a persistent right sacroiliac joint dislocation, and a left sacral fracture nonunion.
Bilateral Fibula Strut Allograft, Bilateral Double Iliac Screws, and L4-S1 Pedicle/Screws
Though a midline lumbosacral incision with bilateral lateral pelvic incisions, the bone edges of the left sacral fracture nonunion, and the right sacroiliac joint dislocation were exposed, and debrided. Next, left-sided transforaminal lumbar interbody fusions utilizing PEEK cages were performed at the L4-L5, and L5-S1 levels. Additionally left-sided L4-L5 and right-sided L4-S1 pedicle screws were placed. This was followed by the application bilaterally of double iliac screws, and the placement of bilateral fibula strut allografts filled with BMP/INFUSE placed from the L4-L5 transverse processes to the sacrum [
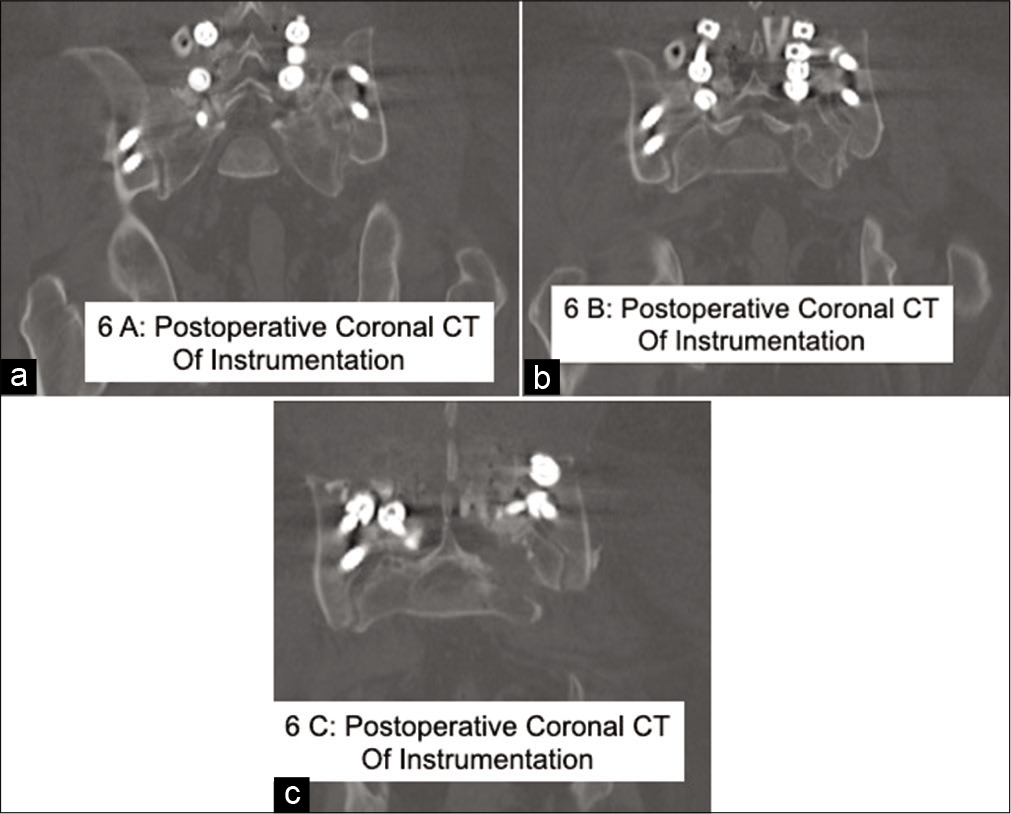
Figures 6:
(a,b, and c) 2D Bone Window CT Reconstructed Images of Final Construct.
Here are three 2D Bone Window-CT postoperative reconstructed images. (a) This coronal bone window CT demonstrated the right pedicle screws in L4, L5, and S1, the left pedicle screws in L4 and L5, and bilateral iliac screws (only partially visualized). (b) This second coronal bone window CT image taken slighlty more dorsally showed some of the rod on the right side. (c) Even further dorsally, this coronal CT bone window image showed the bilateral iliac screws.
DISCUSSION
Review of other Pelvic Reconstruction Techniques
Multiple other alternative pelvic reconstrucdtion techniques were published between 2014-2016 [
Five other studies employed additional techniques for lumbar pelvic ring reconstruction addressing various pathologies [
CONCLUSION
In the case presented, the patient had previously undergone two failed attempts to fuse the lumbar spine to the sacrum following a multi-storey fall. The trauma had resulted in a left sacral fracture, and a right-side dislocation of the sacroliliac joint. The authors successfully fused the lumbar spine to the sacrum, by first combining a lumbar (left L4, L5) and lumbosacral (L4, L5, S1) pedicle/screw/rod fixation technique with L4-L5 and L5-S1 interbody fusions. They additonally placed bilateral double sacral screws (affixed with rods/cross-links), and uniquely applied bilateral fibula strut allografts from L4-S1 filled with BMP.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Ayoub MA, Gad HM, Seleem OA. Standalone percutaneous transiliac plating of vertically unstable sacral fractures: outcomes complications and recommendations. Eur Spine J. 2016. 25: 1153-62
2. Bederman SS, Shah KN, Hassan JM, Hoang BH, Kiester PD, Bhatia NN. Surgical techniques for spinopelvic reconstruction following total sacrectomy: a systematic review. Eur Spine J. 2014. 23: 305-19
3. Chaiyamongkol W, Kritsaneephaiboon A, Bintachitt P, Suwannaphisit S, Tangtrakulwanich B. Biomechanical Study of Posterior Pelvic Fixations in Vertically Unstable Sacral Fractures: An Alternative to Triangular Osteosynthesis. Asian Spine J. 2018. 12: 967-972
4. Padalkar P, Virani N, Kathare A. Posterior Reconstruction of Vertebral Body using Expandable Cage for L5 Burst Fracture Dislocation: Case Report. J Orthop Case Rep. 2014. 4: 5-9
5. Santoro G, Braidotti P, Gregori F, Santoro A, Domenicucci M. Traumatic Sacral Fractures: Navigation Technique in Instrumented Stabilization. World Neurosurg. 2019. 131: 399-407
6. Wagner D, Kamer L, Sawaguchi T, Noser H, Uesugi M, Baranowski A. Space available for trans-sacral implants to treat fractures of the pelvis assessed by virtual implant positioning. Arch Orthop Trauma Surg. 2019. 139: 1385-1391
7. Wei R, Guo W, Yang R, Tang X, Yang Y, Ji T, Liang H. Reconstruction of the pelvic ring after total en bloc sacrectomy using a 3D-printed sacralendoprosthesis with re-establishment of spinopelvic stability: a retrospective comparative study. Bone Joint J. 2019. 101-B: 880-888
8. Xu M, Zheng K, Zhao J, Bai WZ, Yu XC. En Bloc Resection and Pelvic Ring Reconstruction for Primary Malignant Bone Tumors Involving Sacroiliac Joint. Orthop Surg. 2019. 11: 1120-1126